"Discount 20 mg nolvadex visa, breast cancer ribbon template".
K. Onatas, M.A., M.D., Ph.D.
Vice Chair, Stanford University School of Medicine
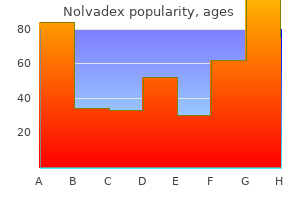
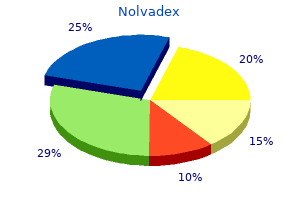
Anagen effluvium, which the loss of growing hairs, is most commonly seen during radiation and chemotherapy treatments for cancer. What puzzling cause of asymmetrical hair loss in a child will sometimes cause an intern to pull his or her hair out? Trichotillomania is hair loss as a result of self-manipulation, such as rubbing, twirling, or pulling. The most common physical finding is unequal hair lengths in the same region without evidence of epidermal changes of the scalp. Behavior modification, along with the application of petroleum or oil to the hair to make pulling more difficult, is the treatment of choice. Rarely a child will swallow the hair and develop vomiting because of the formation of a gastric trichobezoar (hairball). The term flag sign refers to alternating bands of decreased pigment or structural changes of the hair shaft. Children with blond or light-colored hair can develop green hair after long-term exposure to chlorinated swimming pools. Soaks, open-toed sandals, properly fitting shoes, topical or systemic antibiotics, incision and drainage, or surgical removal of the lateral portion of the nail may all be used. Proper instruction on nail care, including straight rather than arc trimming, is mandatory. Acute paronychia (inflammation of the nail fold, usually with abscess formation) is most commonly caused by S. The treatment of acute paronychia includes the oral administration of antistaphylococcal antibiotics. Chronic paronychia is most often caused by Candida albicans and often involves a history of chronic water exposure. Although rarely inflamed, there is edema of the nail folds and separation of the folds from the nail plate. A bacterial culture may reveal a variety of gram-positive and gram-negative organisms. A healthy 7-year-old child who develops progressive yellowing and increasing friability of all nails over a period of 12 months likely has what condition? The progressive development of rough nails with longitudinal grooves, pitting, chipping, ridges, and discoloration occurring in isolation in school-aged children has been given this name, although not all nails need be involved. The etiology remains unclear, and most cases resolve spontaneously without scarring. The nail changes, however, may herald other conditions, such as alopecia areata, lichen planus, and psoriasis. Spread occurs directly by contact with an infected individual or indirectly through the use of shared combs, brushes, or hats. For unknown reasons, infestation is nearly 35 times more likely among whites than blacks. It can be a vector for other diseases, such as epidemic typhus, trench fever, and relapsing fever. A search for lice should be made in any school-aged child presenting with scalp itching. Nits (lice eggs) are found in greatest density on the parietal and occipital areas. On physical examination, an actual louse (wingless, grayish insects about 3 to 4 mm) may be difficult to find, although one should easily be able to find nits. The nits are first attached to the hair close to the surface of the scalp and are oval and flesh colored. When the louse emerges, the empty egg case, or nit, appears white in color and remains firmly attached to the hair shaft as the hair grows out (see. Malathion, a weak organophosphate cholinesterase inhibitor, is currently an approved prescription topical treatment for resistant head lice and their eggs. It should be used in a well-ventilated area given its odor and precautions also include increased absorption through open sores. Once an infestation of lice has been properly treated, the nits are not viable or contagious. Despite this, many schools will not allow children with nits to attend, although this nit-free policy has not been shown to be of benefit for controlling outbreaks.
Another diagnosis to be differentiated is paroxysmal torticollis (also known as Grisel syndrome) [6, 10]. This rare condition particularly affects small children and manifests itself in the form of a severe torticollis that usually occurs after a peripharyngeal infection. Examination of the atlantoaxial joint in cadavers has shown the presence of a system of lymphovenous anastomoses in the epidural sinus which is responsible for the drainage of septic exudates in peripharyngeal inflammation. Since no lymph node stations are present, exudates spread out directly in the C1/C2 joint. Grisel syndrome usually resolves spontaneously, although immobilization is occasionally required, while atlantoaxial arthrodesis is indicated in very rare cases. Another important differential diagnosis is a tumor in the cervical spine (particularly an osteoblastoma) or a soft tissue tumor. Examination by an ophthalmologist is indicated particularly if no restriction in passive mobility or shortening of the sternocleidomastoid muscle is found [11]. Additionally, a unilateral hearing difficulty can lead to a habitual oblique positioning of the head. The differential diagnosis should also include the possibility of secondary muscular torticollis, which occurs Conservative treatment for the neonate consists of physiotherapy, the aim of which is to stretch the shortened sternocleidomastoid muscle. In a substantial proportion of cases it is possible to rectify the problem even during the first year of life. Since we assume that the fibrosis is due to a muscle necrosis arising from a compartment syndrome, cortisone treatment is not particularly appropriate as it achieves the opposite in actually promoting the necrosis. Nor do we primarily employ immobilization with a cervical collar or plaster fixation as stretching of the muscle might only occur in the extreme position, which is unacceptable for small children. Since the prognosis for successful conservative treatment is not so good after the first year, the orthopaedist must then decide whether surgery is indicated. Surgical treatment the surgical treatment involves a distal tenotomy of the clavicular and/or sternal part of the sternocleidomastoid muscle, depending on the section that is actually shortened. If possible, a non-shortened section should be left intact since the sternocleidomastoid muscle is very 120 3. If both sections of the muscle are completely fibrotic, one section must be lengthened in a Z-shape. Since the facial nerve and its branches pass directly through the area of the attachment of the sternocleidomastoid, the risk of injury is relatively high. The argument cited in favor of a proximal tenotomy is that the scar is less visible on the hairline. However, we do not believe that this argument is particularly strong since scars in the anterior part of the neck almost always look very good because the skin is not very taut in this area. The treatment is by no means completed with this (relatively minor and safe) operation. The sternocleidomastoid muscle must be stretched for several months until scar formation has concluded. The scar in the muscle has a strong tendency to retract, and this trend must be counteracted very consistently. We support the physical therapy with a cervical collar that inclines the head towards the opposite side. We do not believe that plaster fixation is very useful postoperatively since the muscle is not adequately stretched when in a position of slight lateral inclination, thus ruling out intensive physiotherapy. They should be encouraged to look in the mirror each day for a prolonged period and concentrate on a straight posture. If tumorous thickening is also present in addition to the muscle shortening, however, the prognosis is not so good [2]. In older children with pronounced facial scoliosis this will often persist and no longer correct itself spontaneously. Cheng J, Chen T, Tang S, Shum S, Wong M, Metreweli C (2001) Snapping during manual stretching in congenital muscular torticollis. Engin C, Yavuz S, Sahin F (1997) Congenital muscular torticollis: is heredity a possible factor in a family with five torticollis patients in three generations?
This appliance can also be used to test how a patient would react to a corrective, stabilizing procedure in which the flexor carpi ulnaris muscle is transferred, in one of various ways, to the extensor carpi radialis brevis or longus muscles (Operation according to Green [10]). A preoperative botulinum toxin A injection will preclude any functional deterioration resulting from a loss of power of the transferred muscle. A wrist arthrodesis can also produce a functional improvement by providing extra stability [19]. Additional procedures on the pronator quadratus muscle may be indicated at the same time, particularly if the improvement in the rotation of the forearm and hand is of prime concern. If active supination up to the neutral position only is possible, the pronator quadratus muscle or the pronator teres muscle should be lengthened. If active supination is absent, but free movement is possible passively, transfer of the pronating muscles is indicated. If movement restriction without pronatory activity is present, the pronator quadratus is lengthened and can be transferred at a later date (Table 3. A possible alternative to muscle weakening by surgical lengthening is the injection of botulinum toxin A. For fixed flexion deformities of the wrist or a concurrent troublesome instability, an arthrodesis of the wrist can produce good results. When correctly performed this procedure can also be employed for young patients without growth disturbances. In addition to the pronation-flexion position of the wrist, the whole hand is often 489 3. If the patient has undergone previous surgery, however, and severe finger deformities persist, operations for correcting the finger function and position must be considered as a supplement to the transfer of the flexor carpi ulnaris muscle (Table 3. The options for correcting the adduction-pronation deformity of the thumb are listed in Table 3. In the swan-neck deformity of the fingers (see above) it is usually sufficient to correct the wrist contracture. Muscle surgery is generally inadvisable in patients with athetotic atactic-dystonic syndromes in view of the risk of overshooting deformities in the opposite direction, which then usually become more troublesome than the originally treated primary deformities (for example, a hyperextension develops after a flexion contracture at the elbow). Consequently, conservative measures tend to be more appropriate than surgical interventions, although stabilizing operations (usually arthrodeses) may be required in some cases. It is technically difficult, however, to provide sufficient stability by internal fixation until the arthrodesis has consolidated. In one patient, for example, we have had to stabilize a wrist arthrodesis with two plates instead of just one. Despite a plaster dressing postoperatively, a further operation was required to correct a pseudarthrosis. Recent studies have shown that deteriorations are unlikely to occur after operations on the upper extremity. Patients undergoing surgery for purely cosmetic reasons have usually benefited from a functional improvement as well [18, 7]. However, the more proximal the lesion, the more likely abnormal sprouting will occur. In view of these considerations, surgical procedures on the upper extremities should be indicated more liberally, subject to the requirement that, as with all functional procedures, reliable and adequate follow-up treatment is provided. Various mechanisms can produce the lesion, from simple stretching to tearing of nerve fibers or the avulsion of the roots from the spinal cord. Etiology and pathogenesis Plexus palsies of the upper extremity can occur at birth as a result of manipulations. Infants in a breech presentation are particularly at risk, although these are almost always delivered by cesarean section nowadays. Older children and adults can suffer plexus lesions of the upper, or more rarely the lower, extremity in traffic accidents (particularly motorcycle accidents) [15]. No basic distinction is made between plexus lesions in the neonate and the adult [17]. If the nerve is not completely severed or torn, the axon will regrow from Sensation and motor activity can be tested in older children and adults. The striking finding in neonates is a failure to move the arm, which hangs limply with the elbow extended and does not even move when the typical infant reflexes are elicited.
Despite many earlier studies demonstrating reticulocytosis and increased hematocrit following treatment with erythropoietin, the modest effect of treatment on the number of transfusions and volume transfused in milliliters has raised questions regarding its efficacy. Because the smallest, most immature infants are frequently transfused before the onset of the effects of erythropoietin, the patients may not experience any decrease in the number of donors to which they are exposed. Furthermore, recent data have raised the question of whether the promotion of neovascularization by erythropoietin could result in an increased incidence of retinopathy of prematurity. Therefore, at the present time, there is wide variation in the use of this hormone. Erythropoietin is currently being investigated as an adjunct therapy to prevent brain injury. Erythropoietin for infants with hypoxic ischemic encephalopathy, Curr Opin Pediatr 22:139145, 2010. If fetomaternal hemorrhage is suspected as a cause of neonatal anemia, how is this diagnosed? The Kleihauer-Betke test detects the presence of fetal cells in the maternal circulation. Because fetal hemoglobin is resistant to elution with acid, the treatment of a maternal blood smear with acid will result in darkly stained fetal cells among the maternal "ghost" cells. One percent fetal cells in the maternal circulation indicates a bleed of about 50 mL. If a gastric aspirate contains blood shortly after birth, what test can determine whether the blood is swallowed maternal blood or fetal hemorrhage? This test relies on the increased sensitivity of adult hemoglobin to alkali as compared with fetal hemoglobin. Adult hemoglobin gives a pink color that becomes yellow in 2 minutes or less, thereby indicating the denaturation of hemoglobin. Polycythemia is defined by a venous hematocrit of 65% because this exceeds the mean hematocrit found in normal newborns by two standard deviations. As the central venous hematocrit rises above 65%, there is an increase in viscosity. In neonates, some of the increase in viscosity with polycythemia is ameliorated by the lower viscosity of plasma. Because direct measurements of blood viscosity are not readily available in most laboratories, a high hematocrit level is thought to be the best indirect indicator of hyperviscosity. Because polycythemia results from a diverse array of etiologies, it is difficult to determine whether outcome depends more on etiology or the chronic elevation of viscosity. Many authorities recommend a partial exchange transfusion, regardless of symptoms, in infants with a central venous hematocrit level of at least 70% (because of the correlation with laboratory-measured hyperviscosity) or in those with a central hematocrit level of 65% or higher if there are signs and symptoms attributable to polycythemia. Describe the preferred method for partial exchange transfusions in polycythemic neonates. Partial exchange transfusions can be performed through an umbilical venous catheter, an umbilical arterial catheter, or a peripheral venous catheter. Aliquots equal to 5% of the estimated blood volume are withdrawn and historically have been replaced either with freshfrozen plasma, Plasmanate, 5% albumin, or normal saline. Adult plasma poses the risk for transfusion-acquired infections and may actually raise neonatal blood viscosity, whereas albumin offers no proven benefit. Therefore, the amount of blood volume to be exchanged with readily available crystalloid may be calculated using the following formula: Blood volume to be exchanged ј Observed hematocrit А desired hematocrit Observed hematocrit Вblood volume В weight рkgЮ 91. Based on numerous studies, a normal platelet count in neonates of any viable gestational age is defined as more than 150,000/mm3. However, counts in the 100,000 to 150,000/mm3 range are frequently seen in healthy newborns. Consequently, patients with counts in this latter category should have repeat counts as well as further studies if illness is suspected. Surveys of neonatologists reveal tremendous variability in the thresholds used for transfusion of platelets especially because most are given prophylactically and are given not to treat active bleeding. Because the risk for bleeding is greatest in the first week of life, consensus opinion offers the guidelines shown in Table 12-10. What features on physical examination suggest a specific cause of thrombocytopenia? What are the two main types of neonatal thrombocytopenia caused by maternal antibody? Babies generally appear well, do not have hepatosplenomegaly, and have thrombocytopenia that persists for 3 to 12 weeks postnatally.
Particular care should be taken to avoid tissue trauma or jaw dislocation when tracheal or nasogastric tubes are inserted. During artificial ventilation, low airway pressures should be used to reduce the risk of a pneumothorax. If conduction defects are present, the temporary insertion of a pacemaker should be considered. If this is declined, delivery by elective Caesarean section at 32 weeks has been recommended (Lurie et al 1998), and close observation for signs of vascular or bowel rupture maintained in the postpartum period. Analysis of literature reports of surgical complications over 20 years, associated with vascular or bowel surgery, showed a high incidence of reperforations, anastomotic leaks, haemorrhage, aneurysms, and vascular dissection. The authors suggest that colonic perforations should be treated with total colectomy and end ileostomy. If vascular surgery must be done, simple vessel ligation, rather than reconstruction, should be attempted (Bergqvist 1996, Freeman et al 1996). Bibliography Anstey A, Mayne K,Winter M et al 1991 Platelet and coagulation studies in EhlersDanlos syndrome. Beighton P, De Paepe A, Steinmann B et al 1998 EhlersDanlos syndromes: revised nosology, Villefranche, 1997. De Paepe A 1996 the EhlersDanlos syndrome: a heritable collagen disorder as a cause of bleeding. Dolan P, Sisko F, Riley E 1980 Anesthetic considerations for EhlersDanlos syndrome. Goldstein M, Miller R 1997 Anesthesia for cesarean delivery in a patient with EhlersDanlos syndrome. The direction of the shunt, and hence the presence or absence of cyanosis, depends on a number of factors. These include hypoxaemia, the pulmonary and systemic pressure differences, and the intravascular volume. Sleep studies have shown that there is a nocturnal deterioration in arterial oxygen saturation, which seems to be related to ventilation/perfusion distribution abnormalities occurring in the supine position (Sandoval et al 1999). Complications include thrombosis secondary to polycythaemia, air embolus, bacterial endocarditis, gout, cholelithiasis, and hypertrophic osteoarthropathy. Contributory factors to the pulmonary hypertension are hypoxia, high pulmonary blood flow, and high left atrial pressure. Irreversible structural changes take place in the small vessels, causing pulmonary vascular obstruction and a reduction in the size of the capillary bed. The pulmonary artery pressure is the same as, or sometimes exceeds, the systemic arterial pressure. The incidence of this syndrome is decreasing because of the more vigorous approach to diagnosis and treatment of congenital heart disease in childhood. In a longterm study of 188 patients over a median period of 31 years, noncardiac surgery with general anaesthesia carried risks of 23. A lower mortality (10%) was quoted in a series of nonparturients, but only half involved general anaesthesia (Raines et al 1996). Presenting symptoms include dyspnoea, tiredness, episodes of cyanosis, syncope, or chest Anaesthetic problems 1. Reductions in systemic arterial pressure by myocardial depression or loss of sympathetic tone are potentially dangerous. A direct correlation between systemic pressure and oxygen saturation was found in a patient undergoing laparoscopic cholecystectomy (Sammut & Paes 1997). General anaesthesia tends to be favoured, since the reduction in systemic vascular resistance associated with regional blockade increases the shunt. However, successful use of epidural anaesthesia for bilateral inguinal herniorrhaphy (Selsby & Sugden 1989), and Caesarean section (Spinnato et al 1981), have been reported. Termination of pregnancy is usually recommended in the first trimester, but is still associated with a mortality of 7%. An increased haemoglobin level in early pregnancy was the only abnormality in one patient, but the significance was not recognised.