"Buy discount drospirenone 3.03mg online, birth control options over 40".
V. Owen, M.B.A., M.B.B.S., M.H.S.
Clinical Director, Northwestern University Feinberg School of Medicine
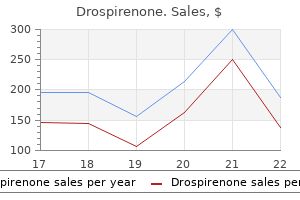
The majority of lab results demonstrate a colonization of gram-positive bacteria (5). Despite these findings, the policy of stethoscope cleaning method and frequency is not established yet (8). Studies show that regular cleaning can greatly reduce the contamination of stethoscope with bacteria (4). Therefore, due to the importance of stethoscope cleaning in reducing the infection and the lack of available information globally and in Saudi Arabia about the method and frequency of stethoscope cleaning by medical practitioners. A backup soft copy version as well as a hard copyprintdated,savedandsecuredaftereachdataentery update. Since the study used aself-administeredquestionnairewithoutaskingforany identification,thenfillingofthequestionnaireistakenas assent. The respondents informed about the purpose of thestudy,eitherverballyorasawrittenparagraphonthe cover page of the questionnaire especially related to how the data used and for what purpose. The questionnairehave5mainsections,includingpersonal characteristics, the awareness of importance of the subject, frequency of stethoscope cleaning, method of stethoscope cleaning, and barriers of stethoscope cleaning(seeappendix1). Questionnaire is distributed by the researchers to all respiratory therapists in intensive care units on their free time, along with a letter of information about the study and its objectives. Staff consent and complete the anonymous questionnaire at their convince time by themselves and return them to the researchers. Table 2: training on cleaning technique of stethoscope (n = 64) Frequency Received proper training 13 Not Received proper 51 training Percentage 20. Table 4: frequency of cleaning stethoscope (n = 64) Betweeneverypatient Several times a shift Once daily Several times a month Other/Cannotremember Frequency Percentage 24 37. Hyder reported that none of respondents has ever clean their stethoscope between every patient, and also the frequency is higher than a previousstudyinPhilippinesdonebyAfrica-Purinoet al. Yet,thefrequencyofcleaningislowconsidering the risk of cross-infection posted by contamination of stethoscope(5)(7). Table 6: method of cleaning of stethoscope (n = 64) Alcohol swap Alcohol hand gel Alcohol spray Anti-septicwipes Soap and water Dry cloth Other Frequency 33 16 33 7 0 0 0 Percentage 51. Prevalence of methicillin-resistant Staphylococcus aureus on the stethoscopes of emergency medical services providers. Cross-sectional study of frequency and factors associated with stethoscope cleaning amongmedicalpractitionersinPakistan. Antibiotics haesideeffects and can damage arious body organs includinglier,kidney, brain, blood, skin, eyes. The main sideeffectsinclude lierdamagethatisoneofthemajor factors of lier inefficiencyinasignificant number of people taking this medication Therefore taking these medications face limitations due to the fact that one of the major side effects of Gentamicin is creating hepaotoxicity (3,4). This will cause damage to membrane lipids, proteins and nucleic acids which leads to lier toxicity, dysfunction andinjury(6). Body weight: All animals were weighed before and after treatment with using digital electronic balance. Serum Preparation: At the end of experimental period, rats were fasted for (10) hrs, anaesthetized withketamine(75mg/kg)combinedwithxylazine (2. Blood samples were collected by heart puncture in non- heparinized tubes, centrifuged at (4000) rpm for (10) minutes (12). The mean differences between the aerages of the studied traits were determined at the probability leel of (0. Histopathological Examination: Light microscopic of lier examination using H&E (400X) stain in control rats showed the normal structure (Fig:1A). By seerely altering mitochondrial function inthelier,drugscaninduce hepatic necrosis, causing cystolytic hepatitis, and can progress into lier failure (17). According to (20) increased catabolism and anorexia are responsible for decreased food intake and causes body weight loss and as well as loss of the tubularcells,inoled in renal water reabsorption leads to dehydration and decreases body weight (21). Oxidatie stress is one of the key mechanisms responsible for lier damage and disease progression. Antioxidants, on the other hand, try to combat the oxidatie stress and minimize its deteriorated effects (24). Based on the 362 Indian Journal of Public Health Research & Development, January 2019, Vol. Preentionof hepatotoxicity with Curcuma longa and Rosmarinus officinalisingentamicintreatedguineapigs. Proteolytic actiity and immunogenicity of oral bromelain within the gastrointestinal tract of mice.
Contraindications · Increased intracranial pressure (signs and symptoms, raised blood pressure, fundoscopic signs). Visualise a vertical line between the highest point of both iliac crests and its transection with the midline of the spine (at level between vertebrae L 3-4). Gently puncture skin with spinal needle at the identified mark and point towards the umbilicus. Ensure that the child lies supine for the next 4 to 6 hours, continue monitoring child till he or she recovers from the sedation. Complications · Headache or back pain following the procedure (from arachnoiditis). The open method (without the metal introducer) of chest tube cannulation is the preferred method except in neonates ii. Bluntly dissect through the subcutaneous tissue and puncture the parietal pleura with the tip of the clamp. For drainage of air, roll the child slightly to the opposite side for easier manoeuvring and advancement of the chest tube. However, for drainage of empyema, roll the child slightly towards same side and point the catheter tip posteriorly and proceed with the rest of the procedure. Place the tip of the chest tube at the incision, point the tip anteriorly for drainage of air and posteriorly for drainage of empyema. Withdraw the introducer partially and advance the chest tube till the desired length. The water should bubble (if pneumothorax) and the fluid moves with respiration if chest tube is in the pleural space. Secure the chest tube with pulse string sutures or sterile tape strips in neonates. Indicated in tension pneumothorax as an emergency measure to decompress the chest until a chest tube is inserted. Gently insert catheter perpendicularly through the second intercostal space, over the top of the third rib, at the midclavicular line while applying a small negative pressure as the needle is advanced. When this happens, remove the needle while leaving the branula in situ to allow the tension pneumothorax to decompress. Prepare the angiocatheter by attaching the T connector to the needle hub and connect the other end of the T-connector to a 3-way stopcock which is connected to a syringe. Insert the angiocatheter at about 1cm below the xiphoid process at angle of 20-30o to the skin and advance slowly, aiming at the tip of the left shoulder while applying light negative pressure with the syringe. Once air or fluid returns in the T connector stop advancing the catheter and aspirate a small amount to confirm positioning. Remove the T connector from the angiocatheter and rapidly hold your finger over the needle hub. Estimate the length of nasogastric tube inserted by measuring the tube from the nostril and extending it over and around the ear and down to the epigastrium. For orogastric tube insertion, the length of tube inserted equal to the bridge of the nose to the ear lobe and to appoint halfway between the lower tip of sternum and the umbilicus. Re-check by plunging air into stomach whilst listening with a stethoscope, or check acidity of stomach contents. Site of puncture is at a point in the outer 1/3 of a line drawn from the umbilicus to the anterior superior illiac spine. Remove the needle and reconnect the catheter to the syringe and aspirate the amount required. Insert the needle attached to a 5cc syringe perpendicular or slightly caudally to the skin, 0. Pass catheter in gently till urine is seen then advance a few centimetres further. Identify site for aspiration - posterior iliac crest preferred, upper anterior-medial tibia for child < 3 months old. Lie child supine for the next 4 to 6 hours and observe for blood soaking the gauze in a child with bleeding diasthesis. Guideline statement 2005: Management of procedure-related pain in children and adolescents.
Disseminated tuberculosis may be associated with tuberculous meningitis, necessitating a lumbar puncture if clinical suspicion of meningeal involvement exists. The clinical picture is similar to that of latestage tuberculosis and is also associated with severe diarrhea. The course is protracted, and the diagnosis is often made by demonstration of the organisms in the blood using the lysiscentrifugation method or on tissue biopsy. Early initiation of amphotericin B therapy is critical while awaiting diagnostic studies. Symptoms and Signs-In addition to features that may localize the primary site of infection, additional information useful for planning empirical therapy include the travel history, tuberculin skin test status, history of exposure to or previous infection with mycobacteria or endemic fungi, and recent use of antibiotics. Besides the primary infection site, examination should focus on potential sites of dissemination, including a careful funduscopic examination, inspection of skin and mucous membranes, and a search for lymphadenopathy and hepatosplenomegaly. Urine culture for fungi and mycobacteria, blood cultures using the lysis-centrifugation method for mycobacteria and fungi, serum antigen for C. Biopsy of suspicious skin or mucosal lesions, lymph nodes, spleen, liver, or bone marrow should be performed expeditiously if results of other studies are unrevealing. Special stains for microorganisms are necessary along with traditional histologic examinations. Cultures from biopsy specimens for many potential organisms may take 46 weeks to yield results. Mass lesions can present in a variety of ways, including symptomatic neurologic deficits, altered mental status, or change in personality. In conjunction with the clinical presentation, imaging studies sometimes may be able to distinguish infection, malignancy, or an inflammatory process. Empirical therapy for toxoplasmosis should be initiated in critically ill patients with focal ring-enhancing brain lesions pending results of serum Toxoplasma titers. Patients with mass lesions and increased intracranial pressure may require endotracheal intubation, ventilatory support, corticosteroids to decrease cerebral edema, antiseizure prophylaxis, and frequent neurologic evaluation. Treatment Patients with sepsis accompanied by hypotension, altered mental status, severe localized infection, or any organ system dysfunction should receive immediate antimicrobial therapy after appropriate cultures have been obtained. Empirical antibiotic treatment should be directed at possible bacterial pathogens; suspicion of fungal or mycobacterial dissemination should prompt initiation of appropriate targeted therapy. In such patients, antifungal and antimycobacterial agents should be considered early; in addition, these antimicrobial regimens also should be considered in any patient who is deteriorating clinically on antibacterial therapy alone. Patients with disseminated tuberculosis can be treated initially with regimens used for pulmonary tuberculosis (see above). If intravenous therapy is necessary, azithromycin plus amikacin or ciprofloxacin should be considered. Elevated opening pressure should be managed with serial (daily) lumbar punctures to reduce pressure to less than 200 mm H2O, or 50% of opening pressure. Patients often present with fever and headache, sometimes in conjunction with nonspecific neurologic findings, including weakness, fatigue, dizziness, lack of alertness, visual changes, and seizures. In contrast to these mild abnormalities, India ink preparations are positive in 4070%; positive cultures are the "gold standard" of diagnosis. Opening pressure always should be measured because it has important prognostic significance. For example, elevated opening pressure of the cerebrospinal fluid (>250 mm H2O) correlates with high cryptococcal polysaccharide antigen, poor clinical response, and decreased short-term survival. Patients with cryptococcal meningitis should be treated with amphotericin B, 609 Dermatologic Problems in the Intensive Care Unit Kory J. Thermoregulation, containment of body fluids, and protection of internal organs and structures from environmental insults are some of the vital functions performed by the skin. The skin is readily available for examination, so inspection often provides important clues to underlying diseases. This chapter focuses on the following categories of cutaneous disorders in the critically ill patient: common skin disorders, drug eruptions, purpura, life-threatening dermatoses, and cutaneous manifestations of infections. Any substance applied to the skin, including tape, cleansing agents, and topical medications, may be the offender. An eruption that appears to improve but subsequently becomes worse may be due to a contact dermatitis from an applied medication. Clinical Features the morphology and distribution of the lesions, as well as the history of exposure, are diagnostic. Clinically, a circumscribed vesiculobullous eruption on a base of erythema, confined to the area of the contact, is the hallmark of contact dermatitis.
A summary of the life cycle of the parasite and the sites of therapeutic interventions are presented in Figure 36. Metabolites of primaquine are believed to act as oxidants that are responsible for the schizonticidal action as well as for the hemolysis and methemoglobinemia encountered as toxicities. Pharmacokinetics: Primaquine is well absorbed on oral administration and is not concentrated in tissues. It is rapidly oxidized to many compounds, the major one being the deaminated drug. Adverse effects: Primaquine has a low incidence of adverse effects, except for drug-induced hemolytic anemia in patients with genetically low levels of glucose-6-phosphate dehydrogenase2 (Figure 36. Other toxic manifestations observed after large doses of the drug include abdominal discomfort, especially when administered in combination with chloroquine (which may affect patient compliance), and occasional methemoglobinemia. Granulocytopenia and agranulocytosis are rarely seen, except in patients with lupus or arthritis (both conditions are aggravated by the drug). Chloroquine specifically binds to heme, preventing its polymerization to hemozoin. The increased pH and the accumulation of heme result in oxidative damage to the membranes, leading to lysis of both the parasite and the red blood cell. Pharmacokinetics: Chloroquine is rapidly and completely absorbed following oral administration. The drug concentrates in erythrocytes, liver, spleen, kidney, lung, melanin-containing tissues, and leukocytes. Chloroquine is dealkylated by the hepatic mixed-function oxidase system, but some metabolic products retain antimalarial activity. Both parent drug and metabolites are excreted predominantly in the urine (Figure 36. Adverse effects: Side effects are minimal at the low doses used in the chemosuppression of malaria. At higher doses, many more toxic effects occur, such as gastrointestinal upset, pruritus, headaches, and blurring of vision (Figure 36. Chloroquine should be used cautiously in patients with hepatic dysfunction or severe gastrointestinal problems or in patients with neurologic or blood disorders. Chloroquine can cause electrocardiographic changes, because it has a quinidine-like effect. Resistance: Resistance of plasmodia to available drugs has become a serious medical problem throughout Africa, Asia, and most areas of Central and South America. Mefloquine is absorbed well after oral administration and concentrates in the liver and lung. It has a long half-life (17 days) because of its concentration in various tissues and its continuous circulation through the enterohepatic and enterogastric systems. Adverse reactions at high doses range from nausea, vomiting, and dizziness to disorientation, hallucinations, and depression. Electrocardiographic abnormalities and cardiac arrest are possible if mefloquine is taken concurrently with quinine or quinidine. These drugs are reserved for severe infestations and for malarial strains that are resistant to other agents, such as chloroquine. Taken orally, quinine is well distributed throughout the body and can reach the fetus. The major adverse effect of quinine is cinchonismв"a syndrome causing nausea, vomiting, tinnitus, and vertigo. These effects are reversible and are not considered to be reasons for suspending therapy. Drug interactions include potentiation of neuromuscular-blocking agents and elevation of digoxin levels if taken concurrently with quinine. Quinine absorption is retarded when the drug is taken with aluminum-containing antacids. Artemisinin (or one of its derivatives) is available for the treatment of severe, multidrug-resistant P.