"Cheap 25 mg sildenafila overnight delivery, erectile dysfunction fix".
X. Jerek, M.B.A., M.B.B.S., M.H.S.
Professor, Stanford University School of Medicine
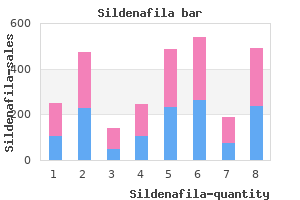
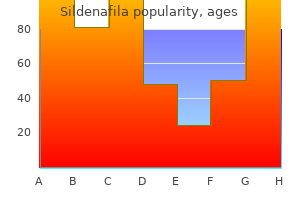
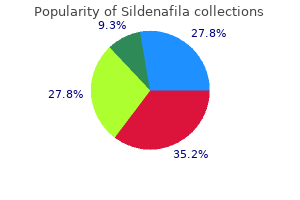
The screw-shaped, threaded implants are rotated into the bone recipient site like a screw with a handpiece or handheld wrench after preparing an osteotomy site that is slightly smaller in diameter than the implant threads. Thus the threads engage the walls of the prepared osteotomy site and provide vertical stabilization. The cylinder-shaped, threadless implants are pushed or tapped into a recipient site that is prepared with a diameter and shape that is nearly identical to that of the implant. Vertical stability comes from the apical end of the implant seating into the bottom of the osteotomy site. Center, Brеnemark screw-shaped, threaded design with external hex and machined surface. Left and right, Cylindrical, threadless design with hydroxyapatite-coated (left) and titanium plasmasprayed (right) surfaces. The threaded implants are more widely used because they usually provide superior initial stability in bone, and vertical positioning of the implant during placement can be more precisely controlled. Some screw-shaped, threaded implants are tapered to resemble the conical shape of a natural tooth root. Tapered implant designs help to minimize apical bone fenestration, allow for the placement of implants into narrower apical sites (between closely approximating roots), and are amenable to immediate placement into anterior extraction sockets (Figure 76-2). ImplantSurfaceTopography(Microdesign) It is generally believed that the textured surfaces accelerate the initial healing phase and enhances bone formation at the implant surface. Although these surfaces achieve secondary stability and integration earlier, progressive bone loss can occur if the rough surface of the implant becomes exposed to oral fluid and microorganisms. Therefore, when using implants with macroscopically rough surfaces, care must be taken to ensure complete submersion of the rough surface in bone with sufficient crestal bone thickness around the implant. Thinner areas of crestal bone have a greater risk of bone loss over time, which can expose the surface to contamination with oral bacteria, leading ultimately to infection and bone loss. However, when compared to implants with "rough" surfaces, machined surfaces provide weaker secondary stability and consequently result in lower success rates in poor-quality or grafted bone12 (Figure 763, C). Figure762 Conically shaped, threaded implant is helpful to minimize apical bone fenestration and also useful in placing implants into extraction sockets immediately. These implant surface modifications have been shown to enhance the bone-to-implant contact and strength of resistance compared with machinedsurface implants. For some patients, depending on individual preferences and complexity of the case, conscious sedation (oral or intravenous) may be indicated (see Chapter 60). Once the patient understands the proposed treatment and has questions answered, a written informed consent should be obtained for the procedure. ImplantSitePreparation Some basic principles must be followed to achieve osseointegration with a high degree of predictability4,6,7 (Box 76-1). The surgical site should be kept aseptic and the patient appropriately prepared and draped for an intraoral surgical procedure. It is recommended that the patient rinse with chlorhexidine gluconate for 30 seconds immediately before the procedure. Every effort should be made to maintain a sterile surgical field at all times and to avoid contamination of the implant surface. Implant sites should be prepared using gentle, atraumatic surgical techniques with a constant reminder to avoid overheating the bone. Finally, implants should be stable and allowed to heal without movement for a time. Implant site preparation should be completed with an atraumatic surgical technique that avoids overheating of the bone during preparation of the recipient site. When these clinical guidelines are followed, successful osseointegration occurs predictably for submerged6 and nonsubmerged15 dental implants. Well-controlled studies of patients with good plaque control and appropriate occlusal forces have demonstrated that root form, endosseous dental implants show little change in bone height around the implant. Regardless of the type of surgical approach, the implant must be placed in healthy bone to achieve osseo-integration, and an atraumatic technique must be followed to avoid damage to bone or vital structures. Bone quality at the recipient site influences the interface between bone and implant. Clinical studies have shown that areas of the jaw exhibiting thin layers of cortical bone and large cancellous spaces, such as the posterior maxilla, have significantly lower success rates than areas of denser bone structures. First, the implant can be stabilized if there is sufficient quantity and quality of bone.
If released to water, acetonitrile is not likely to adsorb to soil and sediment particles. Acetonitrile is expected to be removed from water bodies through volatilization as the chemical hydrolysis and bioaccumulation potential for this chemical are low. Occupational Safety and Health Administration permissible exposure limit ј 40 ppm (70 mg m А 3). National Institute for Occupational Safety and Health immediately dangerous to life or health value ј 500 ppm. Ecotoxicology Toxicity thresholds for protozoa, bacteria, and green algae have been measured to range from 520 mg l А 1 for Microcystis aeruginosa (algae) to 7300 mg l А 1 for Scenedesmus quadricauda (green algae). Acetylaminofluorene 31 Acetylaminofluorene Sanjay Chanda and Harihara M Mehendale & 2005 Elsevier Inc. Ring hydroxylation, however, leads to the formation and excretion of water-soluble conjugates. Acute and Short-Term Toxicity (or Exposure) Animal Uses Acetylaminoflourene is found as a contaminant in coal gasification processes. Background Information 2-Acetylaminofluorene is used frequently by biochemists and technicians. The occupations at greatest risk to acetylaminofluorene exposure are organic chemists, chemical stockroom workers, and biomedical researchers. Exposure Routes and Pathways Skin contact is the most common accidental exposure pathway. Acetylaminoflourene emits toxic fumes of nitrous oxides when heated to decompose and can be toxic when inhaled. Rats treated for three cycles showed high incidence of liver, testis, and zymbal gland tumors. The same treatment when continued for 10 months produces conspicuous morphological alterations in pancreatic granular endoplasmic reticulum together with mitochondrial damage and focal cytoplasmic degradation. Guinea pigs and 32 Acetylaminofluorene monkeys fail to develop tumors after treatment. Liver tumors (but not bladder tumors) have been induced in chickens, fish, cats, and hamsters. Chemical hydrolysis, oxidation, volatilization, and bioaccumulation are not expected to be significant. If released to the atmosphere, 2-acetylaminofluorene may undergo vapor phase adsorption to airborne particulate matter, it may react with photochemically generated hydroxyl radicals (estimated vapor phase half-life ј 5. Other Hazards Acetylaminofluorene can be easily ignited by heat, sparks, or flames. They can spread along ground and collect in low or confined areas (sewers, basements, tanks). Identified as an occupational carcinogen without establishing a permissible exposure limit. Clinical Management In case of contact with the eyes, the eyes should be immediately flushed with running water for at least 15 min. If vapor is inhaled, the victim should be moved to fresh air and emergency medical care provided. If the victim is not breathing, artificial respiration should be provided; if breathing is difficult, oxygen should be administered. Environmental Fate Release of 2-acetylaminofluorene to the environment from artificial sources is probably not significant since less than 20 lb year А 1 of this compound are consumed in the United States. Chemical hydrolysis, oxidation, and volatilization are not expected to be significant. Acetylcholine 33 Acetylcholine Sanjay Chanda and Harihara M Mehendale & 2005 Elsevier Inc. If the enzyme is depleted or inhibited, then excessive acetylcholine accumulation in the body can cause toxicity. Symptoms are salivation, lacrimation, urination, diarrhea, muscle tremor, and fasciculation. Mechanism of Toxicity Cholinergic agents can increase the acetylcholine level at the synaptic junction and cause rapid firing of the postsynaptic membrane.
Memory, executive, and multidomain subtle cognitive impairment: clinical and biomarker findings. Neuropsychological criteria for mild cognitive impairment improves diagnostic precision, biomarker associations, and progression rates. Susceptibility of the conventional criteria for mild cognitive impairment to false-positive diagnostic errors. Subjective cognitive complaints contribute to misdiagnosis of mild cognitive impairment. Subjective memory complaint only relates to verbal episodic memory performance in mild cognitive impairment. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. Vascular disease and risk factors are associated with cognitive decline in the alzheimer disease spectrum. Complex brain networks: graph theoretical analysis of structural and functional systems. Destruction of white matter integrity in patients with mild cognitive impairment and Alzheimer disease. The Alzheimer structural connectome: changes in cortical network topology with increased amyloid plaque burden. Connectivity network measures predict volumetric atrophy in mild cognitive impairment. Epidemic spreading model to characterize misfolded proteins propagation in aging and associated neurodegenerative disorders. Extension and refinement of the predictive value of different classes of markers e82 M. Everyday cognition scale items that best discriminate between and predict progression from clinically normal to mild cognitive impairment. Gray & white matter tissue contrast differentiates Mild Cognitive Impairment converters from non-converters. Individualized Gaussian process-based prediction and detection of local and global gray matter abnormalities in elderly subjects. Spatially Weighted Principal Component Regression for High-Dimensional Prediction. Multiple kernel learning with random effects for predicting longitudinal outcomes and data integration. Sotolongo-Grau O, Pesini P, Valero S, Lafuente A, Buendia M, PerezGrijalba V, et al. Association between cell-bound blood amyloidbeta(1-40) levels and hippocampus volume. Lehallier B, Essioux L, Gayan J, Alexandridis R, Nikolcheva T, Wyss-Coray T, et al. Combined Plasma and Cerebrospinal Fluid Signature for the Prediction of Midterm Progression From Mild Cognitive Impairment to Alzheimer Disease. Development of a diagnostic test based on multiple continuous biomarkers with an imperfect reference test. Neurodegenerative disease diagnosis using incomplete multi-modality data via matrix shrinkage and completion. Biomarker progressions explain higher variability in stage-specific cognitive decline than baseline values in Alzheimer disease. Comparison of Visual and Quantitative Florbetapir F 18 Positron Emission Tomography Analysis in Predicting Mild Cognitive Impairment Outcomes. Proposal of a new tractographic feature for analysis of white matter in Alzheimer diffusion mr images. Cortical surface biomarkers for predicting cognitive outcomes using group l2,1 norm.
Similarly, meaningful neural connections in the brain are whittled from a mass of cells. Apoptosis research, with roots in developmental and cell biology, genetics, and immunology, embraces this long-ignored natural law. Apoptotic cells, upon completion of their mission, execute a suicidal program and form apoptotic bodies which are rapidly removed by a variety of resident and nonresident scavenger cells. Unlike necrosis, apoptotic cells do not release any enzyme; however, activation of a tissue enzyme transglutaminase has been reported in several systems. Massive cellular demise by apoptosis generally does not lead to organ dysfunction as opposed to necrotic cell death. In contrast, necrosis typically affects groups of contiguous cells, and an inflammatory reaction usually develops in the adjacent viable tissue in response to the released cellar debris. Stages of Apoptosis the cellular machinery of apoptotic death turns out to be as intrinsic to the cell as mitosis. Apoptotic process is executed in an organized fashion and usually solicits participation of all the intracellular organelles. The time to onset of apoptosis after a lethal stimulus is variable (minutes to hours) but the changes are extremely rapid. In apoptosis, coordinated changes occur in the nucleus, the cytoplasm, and at the cell surface. In vivo, apoptosis usually affects single cells or small groups of cells in an asynchronous fashion and the entire process can be primarily divided into four distinct stages: (1) cell shrinkage, (2) nuclear condensation and fragmentation, (3) cellular fragmentation and formation of apoptotic bodies, and (4) apoptotic body or debris clearance by phagocytosis. The major sequence of events that are associated with apoptosis and necrosis are presented in Table 1. Step I: Cellular Shrinkage the earliest changes observed include the loss of cell junctions and other specialized plasma membrane Table 1 Sequence of cellular events associated with apoptosis contrasted with those associated with necrosis Characteristic Distribution Adhesion between cells and to basement membrane Cellular morphology Apoptosis Affects individual cells scattered throughout the tissue Lost early Necrosis Affects massive and contiguous cells Lost but late (a) Chromatin condensation (karyorrhexis) followed by margination as large crescents to the periphery of the nuclear membrane; fragmentation in large masses (convolution). See Figure 1b (b) Loss of cell volume (cytoplasmic compaction) Damage to organelles. See Figure 1c (b) Very early swelling of cell, ballooning occurs frequently Very early swelling of organelles; cells disintegrate and lyse, appear chaotic, form blebs early (organelles are not found in blebs) Random or irregular damage (appears as a smear on gel) Present Hours to days Forms apoptotic bodies, occasionally containing intact organelles Usually phagocytosis by all types of resident and nonresident cells Absent Strictly energy-dependent, very tightly regulated, signaling-dependent, can easily be delayed but can be inhibited with difficulty Strictly dependent Absent Intact Swelling, disintegration, dissolution Usually cells are not removed Present Energy and signaling-independent, occasionally energy-dependent, can be blocked prior to irreversible changes. Typically, the cytoplasm begins to shrink following the cleavage of lamins and actin filaments, and in some instances cytoplasm becomes hypertrophied. Under an electron microscope, these fragments appear very dense and dark in the neartotal absence or loss of volume regulation of other organelles such as the mitochondria. The contraction of cytoplasmic volume is apparently associated with loss of intracellular fluid and ions. Photomicrographs of normal (panel a), apoptotic (panel b), and necrotic (panel c) liver cells are presented in Figure 1ac. Liver injury and apoptosis was induced by a single hepatotoxic dose of acetaminophen (500 mg kg А 1, i. The cell transiently adopts a deeply convoluted outline and shows extensive surface blebbing. In order to promote their phagocytosis by macrophages, apoptotic cells often elicit biochemical changes on the plasma membrane surface that appeal to the macrophage response. Lysophosphatidylcholine generated as a result of caspase-3-mediated activation of the Ca2 ю -independent phospholipase-A2 renders cells vulnerable to phagocytosis. Membrane changes can often be observed morphologically through the appearance of membrane blebs or blisters which often appear toward the end of the apoptotic process. Under the microscope, appearance of apoptotic bodies is a common feature used by trained pathologists to identify apoptosis in any tissue. These phagocytic cells are responsible for removing apoptotic cells from tissues in a clean and tidy fashion that avoids many of the problems associated with necrotic cell death. Although professionally trained engulfing cells are typically members of the reticuloendothelial system (mononuclear phagocytes such as macrophages, phagocytes, etc. The endocytosed apoptotic debris is rapidly degraded by a series of enzymes within lysosomes, and the adjacent cells move around or if necessary, proliferate to replace the gap created by the just-deleted apoptotic cell. However, the overall process appears to go through three distinct phases at the molecular level: an induction phase, an effecter phase, and a degradation phase.
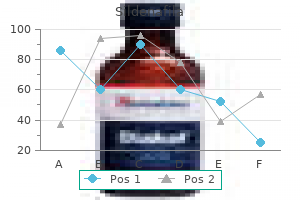
In two-stage implant surgery the implant must be surgically exposed following an undisturbed healing period. Other systems require a healing abutment to be attached to the implant so that it can be used in a one-stage approach8(76-4, B). The advantages of the one-stage surgical approach include easier mucogingival management around the implant in many cases. Patient management is simplified because a second-stage exposure surgery is not necessary. The two-stage, submerged approach is advantageous for situations that require simultaneous bone augmentation procedures at the time of implant placement. This approach also prevents movement of the implant by the patient, who may inadvertently chew on it during the healing period. Fundamental differences in flap management for these two surgical techniques are described separately. In the mandible the implants are left undisturbed for 2 to 4 months, whereas in the maxilla they are allowed to heal for 4 to 6 months. Over time, osteoblasts migrate to the surface and form bone adjacent to the implant (osseointegration)5(see Chapter 73). Shorter healing periods are indicated for implants placed in good quality (dense) bone and for implants with an altered surface microtopography. In the second-stage (exposure) surgery, the implant is uncovered and a healing abutment is connected to allow emergence of the implant/abutment through the soft tissues, thus facilitating access to the implant from the oral cavity. The restorative dentist then proceeds with the prosthodontic aspects of the implant therapy (impressions and fabrication of prosthesis). The following paragraphs describe the steps for the first-stage implant placement surgery (Figures 765, 76-6, and 76-7). FlapDesign,Incisions,andElevation Flap management for implant surgery will vary slightly depending on the location and objective of the planned surgery. A periosteal elevator is then used to reflect a mucoperiosteal (full-thickness) flap. For the crestal design of flap, the incision is made along the crest of the ridge, bisecting the existing zone of keratinized mucosa (see Figures76-5, A, and 76-7, B). When extensive bone augmentation is planned, a remote incision with layer suturing technique is used to minimize the incidence of bone graft exposure. The crestal incision, however, is preferred in most cases because it is easier to manage and results in less bleeding, less edema, and faster healing. A full-thickness flap is raised buccally and lingually to the level of the mucogingival junction, exposing the alveolar ridge of the implant surgical sites (Figures 76-5, B, and 76-7, C). Elevated flaps may be sutured to the buccal mucosa or the opposing teeth to keep the surgical site open during the surgery. The bone at the implant site(s) must be thoroughly debrided of all granulation tissue. Figure765 A, Crestal incision made along the crest of the ridge, bisecting the existing zone of keratinized mucosa. B, Full-thickness flap is raised buccally and lingually to the level of the mucogingival junction. A sharp ridge can be surgically contoured to provide a reasonably flat bed for the implant. For a "knife-edge" alveolar process with sufficient alveolar height and distance from vital structures. However, if a site has less than 10 mm of remaining alveolar bone, the knife-edge alveolar bone should be preserved. Bone augmentation procedures can be used to increase the ridge width (see Chapter 77). A series of drills are used to prepare the osteotomy site precisely and incrementally for an implant (Figure 76-8).