"Cheap 250mg divalproex amex, treatment quad strain".
M. Ugrasal, M.A., Ph.D.
Assistant Professor, University of Missouri–Kansas City School of Medicine
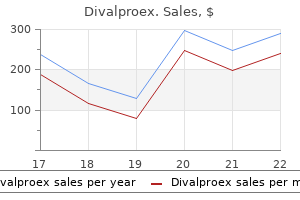
Previous studies have demonstrated an 18% recidivism47 rate within one year, which may account for our numbers; however, we would expect to see this reflected across all the years, which would not account for the overall upward trend. The author postulates that determinants present at a younger age, such as lifestyle or poor nutrition in the southern region, are driving this overall risk. There is evidence to suggest that poorer socioeconomic status is associated with a higher risk of falls in part due to poor housing, roads and sidewalks and surrounding environments. Census data the South has had the highest percentage of poverty as compared to the rest of the country since 1950,42 which may be contributing to the increasing rate of falls in this area; however, further research is needed to assess this association and understand if other factors are mediating this effect. Interestingly, it appears that there is an increasing rate of falls despite national falls-prevention initiatives. Many of these initiatives involve linking to community falls programs and incorporating screening algorithms into office-based practice. Such initiatives are challenging to implement due to their cost, time requirements, need for adaptation and limited use by the community. Despite the potential effectiveness of fall-prevention programs, participation ranges from 15% to 50% with women having higher enrollment and completion rates than men. Census Bureau as the field data collection agent, which can introduce error into the dataset. Deaths from unintentional injury among adults aged 65 and over: United States, 2000-2013. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. Trends in Caregiving Assistance for Home-Dwelling, Functionally Impaired Older Adults in the United States, 1998-2012. Fatalities and injuries from falls among older adults-United States, 1993-2003 and 2001-2005. Racial/Ethnic predictors of falls among older adults: the health and retirement study. Self-reported falls and fall-related injuries among persons aged>or=65 years-United States, Western Journal of Emergency Medicine 792 Volume 18, no. Do rates of hospital admission for falls and hip fracture in elderly people vary by socio-economic status Effectiveness of falls clinics: an evaluation of outcomes and client adherence to recommended interventions. Factors influencing the implementation of fall-prevention programmes: a systematic review and synthesis of qualitative studies. Implementing the evidence for preventing falls among community-dwelling older people: a systematic review. A randomized controlled trial of a multifactorial falls prevention intervention for older fallers presenting to emergency departments. Falls among adults: the association of cardiorespiratory fitness and physical activity with walking-related falls. Circumstances and consequences of falls in independent community-dwelling older adults. Unexpected geographic variation in rates of hospitalization for patients who have fracture of the hip. The geographic incidence and treatment variation of common fractures of elderly patients. Is geographic variation in hip fracture rates related to current or former region of residence Langdorf Submission history: Submitted November 16, 2017; Revision received May 10, 2017; Accepted May 8, 2017 Electronically published July 14, 2017 Full text available through open access at escholarship.
However, the formulation of diltiazem given was not stated and the effects of multiple dosing, or of larger doses of diltiazem, is unknown. Bear in mind the potential for an interaction should a patient taking guggul have a reduced response to diltiazem. Guggul + Statins An isolated case suggests that guggul alone can cause rhabdomyolysis. Clinical evidence A case of rhabdomyolysis has been reported in a patient, 2 weeks after an extract of guggul 300 mg three times daily was started. The patient was not reported to be taking any other medication known to cause rhabdomyolysis and simvastatin had been stopped one year previously because of an increase in creatine kinase. The herbal product used was prepared by a local chemist using a standardised drug extract of the oleo gum resin without excipients. Importance and management this appears to be the only case report of rhabdomyolysis occurring with a guggul-containing preparation. Guggul is widely used for cholesterol lowering, and the most commonly used conventional drugs for this condition are the statins, which are well recognised, rarely, to cause rhabdomyolysis. It is quite likely that guggul and statins are being used together, and the concern generated by this case report is that, if guggul alone can cause rhabdomyolysis, then combined use might increase the risk of rhabdomyolysis. However, this is only one case, and the mechanism (which could include adulteration) is uncertain. Bear the possibility of an additive effect in mind if myositis occurs with concurrent use. All patients taking statins should be warned about the symptoms of myopathy and told to report muscle pain or weakness. It would be prudent to reinforce this advice if they are known to be taking guggul. Guggul + Propranolol Limited evidence suggests that guggul modestly reduces the absorption of single-dose propranolol. This single dose of propranolol did not have any effect on blood pressure or heart rate in these particular subjects,1 so it was not possible to assess the effect of the reduction in levels of Hawthorn Crataegus laevigata (Poir. For information on the pharmacokinetics of individual flavonoids present in hawthorn, see under flavonoids, page 186. Other studies do not appear to have identified any clinically significant drug interactions. For information on the interactions of individual flavonoids present in hawthorn, see under flavonoids, page 186. Constituents the leaves and flowers of hawthorn are usually standardised to their flavonoid content, and the berries may be standardised to their procyanidin content. Other flavonoids present include quercetin, isoquercetin and their glycosides, and rutin. Other constituents include catechins and epicatechin dimers, polyphenolic acid derivatives including chlorogenic and caffeic acids, phenethylamine, dopamine, and ursolic and oleanolic acid triterpenenoid derivatives. Use and indications Hawthorn extracts are used as a cardiotonic, mild antihypertensive and antisclerotic. H 247 248 Hawthorn patients, many of whom were taking antihypertensives, the effect was small. As such, it is unlikely that clinically important hypotension would occur if hawthorn is added to existing antihypertensive treatment. Hawthorn + Antidiabetics Hawthorn does not appear to affect the glycaemic control in patients taking conventional antidiabetic drugs. Clinical evidence In a randomised study, 80 patients with type 2 diabetes taking antidiabetics (including metformin, gliclazide and/or low-dose insulin) with or without antihypertensives were given hawthorn extract 600 mg twice daily, or placebo, for 16 weeks. There was no difference between the two groups in measures of glycaemic control (fasting glucose, glycosylated haemoglobin and fructosamine) at 16 weeks. However, as no alteration in glycaemic control was reported, no interventions are deemed necessary in patients taking antidiabetics and hawthorn extract. Hypotensive effects of hawthorn for patients with diabetes taking prescription drugs: a randomised controlled trial. Clinical evidence In a randomised, crossover study, 8 healthy subjects were given hawthorn extract 450 mg twice daily with digoxin 250 micrograms daily for 21 days, or digoxin 250 micrograms alone daily for 10 days. While digoxin levels tended to be lower when hawthorn was given (the biggest difference being a 23% reduction in the trough level), these reductions were not statistically significant.
Onset, which is usually in later life, can be abrupt, following one particular ischaemic episode, or there may be more gradual emergence. The dementia is usually the result of infarction of the brain due to vascular diseases, including hypertensive cerebrovascular disease. Diagnostic guidelines the diagnosis presupposes the presence of a dementia as described above. Impairment of cognitive function is commonly uneven, so that there may be memory loss, intellectual impairment, and focal neurological signs. An abrupt onset or a stepwise deterioration, as well as the presence of focal neurological signs and symptoms, increases the probability of the diagnosis; in some cases, confirmation can be provided only by computerized axial tomography or, ultimately, neuropathological examination. Associated features are: hypertension, carotid bruit, emotional lability with transient depressive mood, weeping or explosive laughter, and transient episodes of clouded consciousness or delirium, often provoked by further infarction. Personality is believed to be relatively well preserved, but personality changes may be evident in a proportion of cases with apathy, disinhibition, or accentuation of previous traits such as egocentricity, paranoid attitudes, or irritability. Diagnostic guidelines Presence of a dementia as described above; presence of features characteristic of one of the specified syndromes, as set out in the following categories. The neuropathological picture is one of selective atrophy of the frontal and temporal lobes, but without the occurrence of neuritic plaques and neurofibrillary tangles in excess of that seen in normal aging. Diagnostic guidelines the following features are required for a definite diagnosis: - 51 - (a) a progressive dementia; (b)a predominance of frontal lobe features with euphoria, emotional blunting, and coarsening of social behaviour, disinhibition, and either apathy or restlessness; (c)behavioural manifestations, which commonly precede frank memory impairment. Onset is usually in middle or later life, typically in the fifth decade, but may be at any adult age. Diagnostic guidelines Creutzfeldt-Jakob disease should be suspected in all cases of a dementia that progresses fairly rapidly over months to 1 or 2 years and that is accompanied or followed by multiple neurological symptoms. In some cases, such as the so-called amyotrophic form, the neurological signs may precede the onset of the dementia. There is usually a progressive spastic paralysis of the limbs, accompanied by extrapyramidal signs with tremor, rigidity, and choreoathetoid movements. Other variants may include ataxia, visual failure, or muscle fibrillation and atrophy of the upper motor neuron type. The triad consisting of - rapidly progressing, devastating dementia, - pyramidal and extrapyramidal disease with myoclonus, and - a characteristic (triphasic) electroencephalogram is thought to be highly suggestive of this disease. The rapid course and early motor involvement should suggest Creutzfeldt-Jakob disease. Symptoms typically emerge in the third and fourth decade, and the sex incidence is probably equal. In a proportion of cases, the earliest symptoms may be depression, anxiety, or frank paranoid illness, accompanied by a personality change. Involuntary choreiform movements, typically of the face, hands, and shoulders, or in the gait, are early manifestations. They usually precede the dementia and only rarely remain absent until the dementia is very advanced. Other motor phenomena may predominate when the onset is at an unusually young age. The dementia is characterized by the predominant involvement of frontal lobe functions in the early stage, with relative preservation of memory until later. Includes: dementia in paralysis agitans dementia in parkinsonism Differential diagnosis. Apathy, reduced spontaneity, and social withdrawal are common, and in a significant minority of - 53 - affected individuals the illness may present atypically as an affective disorder, psychosis, or seizures. Physical examination often reveals tremor, impaired rapid repetitive movements, imbalance, ataxia, hypertonia, generalized hyperreflexia, positive frontal release signs, and impaired pursuit and saccadic eye movements. The neurological involvement most often occurs in the absence of opportunistic infections and neoplasms, which is not the case for adults. Parkinsonism-dementia complex of Guam should also be coded here (identified by a fifth character, if necessary). It is a rapidly progressing dementia followed by extrapyramidal dysfunction and, in some cases, amyotrophic lateral sclerosis. The disease was originally described on the island of Guam where it occurs with high frequency in the indigenous population, affecting twice as many males as females; it is now known to occur also in Papua New Guinea and Japan. While immediate recall is preserved, the ability to learn new material is markedly reduced and this results in anterograde amnesia and disorientation in time.
Even with careful assessments of suicide risk, the ability to predict suicidal behavior is poor, with many false positives. The assessment of suicide risk is complicated by the fact that suicidal individuals often conceal their thoughts and plans or act impulsively on short-lived suicidal thoughts, making their response to direct questions an unreliable predictor of dangerousness to self. For this reason, in addition to using direct questioning, the psychiatrist should also obtain information through observation and collateral history whenever possible (22, 25). The risk of suicide should also be monitored as treatment proceeds, since variations in depressive symptoms may be associated with fluctuations in suicide risk. In youth and young adults, increases in suicidal thoughts and attempts have been reported early in the course of treatment with antidepressants, although no increases in mortality rates were seen in clinical trials (26). Family members can provide information that increases the likelihood of early detection of harmful behaviors. It is also useful to convey the expectation that family members will call the psychiatrist if concerns for safety emerge (27). Psychiatrists accordingly should assess not only suicidal risk but also history of violence, homicidal ideation, and plans of violence toward others. Whenever suicidal or violent ideas are expressed or suspected, careful documentation of the decision-making process is essential. In addition, patients who exhibit suicidal or violent ideas or intent require close monitoring. Patients with suicidal or homicidal ideation, intention, or plans require close monitoring. For those at significant risk, measures such as hospitalization should be considered; hospitalization is usually indicated for patients who are considered to pose a serious threat of harm to themselves or others. Patients who refuse can be hospitalized involuntarily if their condition meets the criteria of the local jurisdiction for involuntary admission. Severely ill patients who lack or reject adequate social support outside of a hospital setting should be considered for admission to a hospital or intensive day program, if available. In addition, patients who also have complicating psychiatric or general medical conditions or who have not responded adequately to outpatient treatment may need to be hospitalized. Unfortunately, the spectrum of treatment settings available to patients is often limited by lack of availability of options in the geographic setting, lack of ability to pay for care, and/or limitations imposed by third party payers. Evaluate functional impairment and quality of life the assessment of a patient with major depressive disorder includes a determination of the severity and chronicity of symptoms. Even mild depression can impair function and threaten life and the quality of life. In the extreme, depressed people may be totally unable to function socially or occupationally or even to feed and clothe themselves and maintain minimal personal hygiene. Severely depressed patients may be immobilized to the point of being bedridden, with associated medical complications. The psychiatrist should address impairments in functioning and help the patient to set specific goals appropriate to his or her functional impairments and symptom severity. This will likely involve helping the patient to establish intermediate, pragmatic steps in the course of recovery. For example, the psychiatrist may help patients who are having difficulty meeting commitments to develop a reasonable plan to fulfill their obligations. The psychiatrist may advise other patients not to make major life changes while in the midst of a major depressive episode. Establish the appropriate setting for treatment Treatment settings for patients with major depressive disorder include a continuum of possible levels of care, from involuntary hospitalizations to partial hospital programs, skilled nursing homes, and in-home care. In general, patients should be treated in the least restrictive setting that is most likely to prove safe and effective. Practice Guideline for the Treatment of Patients With Major Depressive Disorder, Third Edition tients what bothers them the most about their depression and determining how their current activities and enjoyment of life have been altered by their depressive symptoms. The overall goals of treatment of major depressive disorder should focus on alleviating functional impairments and improving quality of life in addition to achieving symptom resolution and episode remission. He or she may initiate the medical evaluations or coordinate care with other appropriate clinicians.