"Discount 200 mg zovirax fast delivery, hiv infection unaids".
D. Chenor, M.A., M.D., Ph.D.
Co-Director, Keck School of Medicine of University of Southern California
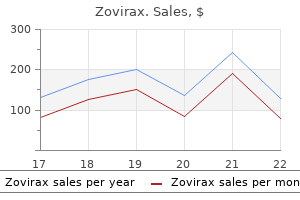
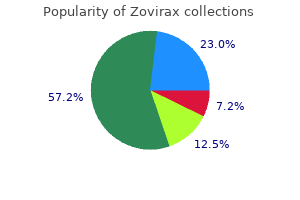
Thus, a steady-state is achieved in which the plasma concentration of drug remains constant. First, what is the relationship between the rate of drug infusion and the plasma concentration of drug achieved at the plateau, or steady state? Second, what length of time is required to reach the steady state drug concentration? Influence of the rate of drug infusion on the steady state: A steady-state plasma concentration of a drug occurs when the rate of drug elimination is equal to the rate of administration (Figure 1. For example, if the infusion rate is doubled, the plasma concentration ultimately achieved at the steady state is doubled (Figure 1. Thus, any factor that decreases clearance, such as liver or kidney disease, increases the steady-state concentration of an infused drug (assuming Vd remains constant). Factors that increase clearance of a drug, such as increased metabolism, decrease the steady-state concentrations of an infused drug. Time required to reach the steady-state drug concentration: the concentration of drug rises from zero at the start of the infusion to its ultimate steady-state level, Css (Figure 1. The fractional rate of approach to a steady state is achieved by a first-order process. Exponential approach to steady state: the rate constant for attainment of steady state is the rate constant for total body elimination of the drug, ke. Thus, fifty percent of the final steady-state concentration of drug is observed after the time elapsed since the infusion, t, is equal to t1/2, where t1/2 (or half-life) is the time required for the drug concentration to change by fifty percent. Waiting another half-life allows the drug concentration to approach 75 percent of Css (see Figure 1. The drug concentration is ninety percent of the final steady-state concentration in 3. For convenience, therefore, one can assume that a drug will reach steady-state in about four half-lives. The time required to reach a specific fraction of the steady-state is described by where f = the fractional shift (for example, 0. Effect of the rate of drug infusion: the sole determinant of the rate that a drug approaches steady state is the t1/2 or ke, and this rate is influenced only by the factors that affect the half-life. The rate of approach to steady state is not affected by the rate of drug infusion. Although increasing the rate of infusion of a drug increases the rate at which any given concentration of drug in the plasma is achieved, it does not influence the time required P. This is because the steady-state concentration of drug rises directly with the infusion rate (see Figure 1. Rate of drug decline when the infusion is stopped: When the infusion is stopped, the plasma concentration of a drug declines (washes out) to zero with the same time course observed in approaching the steady state (see Figure 1. This relationship is expressed as where Ct i = the plasma concentration at any time, C0 = the starting plasma concentration, ke = the first-order elimination rate constant, and t = the time elapsed. Loading dose: A delay in achieving the desired plasma levels of drug may be clinically unacceptable. Therefore, a вoeloading doseв of drug can be injected as a single dose to achieve the desired plasma level rapidly, followed by an infusion to maintain the steady state (maintenance dose). Kinetics of fixed-dose/fixed-time-interval regimens Administration of a drug by fixed doses rather than by continuous infusion is often more convenient. However, fixed doses, given at fixed-time intervals, result in time-dependent fluctuations in the circulating level of drug. Because the rate of elimination is usually first order in regard to drug concentration, the circulating level of drug decreases exponentially with time (Figure 1. Because most drugs are given at intervals shorter than five half-lives and are eliminated exponentially with time, some drug from the first dose remains in the body at the time that the second dose is administered, and some from the second dose remains at the time that the third dose is given, and so forth. Therefore, the drug accumulates until, within the dosing interval, the rate of drug loss (driven by an elevated plasma concentration) exactly balances the rate of drug administrationв"that is, until a steady state is achieved. Model assumes rapid mixing in a single body compartment and a half-life of twelve hours. Effect of dosing frequency: the plasma concentration of a drug oscillates about a mean. Using smaller doses at shorter intervals reduces the amplitude of the swings in drug concentration. However, the steady-state concentration of the drug, and the rate at which the steady-state is approached, are not affected by the frequency of dosing.
The eighth (vestibule-cochlear) nerve: - it mediates the sense of hearing and also important for rotational perception and keeping balance. In conduction problems sound lateralizes to the abnormal ear and in neural deafness to the normal ear. Vestibular portion of the eighth nerve is evaluated during testing of the extra ocular movements, the examiner observes for nystagmus. The ninth cranial (glosso pharyngeal) nerve mediates · · Taste sensation from the posterior 1/3 of the tongue Motor supplies to muscles of the pharynx Examination includes -Checking for taste over the posterior third of the tongue. The tenth cranial (vagus) nerve mediates · · Sensory and motor supply to the pharynx, larynx together with the ninth Autonomic (parasympathetic) supply to thoracic and abdomen al viscera - watching movement of the uvula, which normally rises to the midline during phonation ("ah" reflex). The eleventh cranial (accessory) nerve: - Originates from the upper spinal ganglia and innervates sternocleidomastoid and trapizius muscles. This nerve is evaluated by observing neck motion and by testing the trapezius and sternocleidomastoid muscles. The patient is asked to keep his shoulders shrugged while the examiner attempts to push them down. Weakness that is secondary to hypoglossal nerve involvement on one side is manifested by deviation of the tongue toward the side of the lesion. Inspection the muscles of the limbs are specifically observed for Resting position of the limbs Size Symmetry Presence of atrophy Fasciculations (fine twitching movements) and Involuntary movements such as a tremor. Testing for muscle tone this can be accomplished by movement of the limbs passively at every joint while the patient is completely relaxed. Clasp knife rigidity which may be found an upper motor lesions Cog- Wheel rigidity which is found in Parkinsonism. Muscle power Screening tests for muscle strength In the Upper limbs Hand Grip: - is assessed by testing and comparing bilateral hand grips. The patient is asked to grip objects or while the examiner tries remove object from his hand. Tell the patient to extend his hands, palms up, straight at shoulder level and to close his eyes. Then proceed to examine power of each muscle group at every joint by pulling or pushing in the direction opposite to its action. Triceps reflex Support arm and let forearm hang freely If patient is sitting strike the triceps tendon above the elbow with the broadside of the hammer If patient is lying flex the arm at the elbow and hold close to the chest. Note contraction of the quadriceps and extension of the knee Ankle reflex Dorsiflexion of the foot at the ankle Strike the Achilles tendon Watch and feel for plantar flexion at the ankle. The superficial abdominal reflex: - is tested by lightly stroking the skin of the abdomen from above downward and laterally to medially. The cremasteric reflex: - is tested by pinching or stocking the skin of the medical aspect of the thigh. Contraction of the cremasteric muscle occurs, resulting in elevation of the testis on the same side. Sucking reflex - when the centre of the lip is touched with a tongue blade there is a sucking movement of lips. Rooting reflex- when the corner of the lips are touched with the tongue blade the lips move towards the blade. Grasp reflex- touching of the palm between the index finger and the thumb will stimulate forced grasp. Palmomental reflex- scratching of the palm diagonally results in the contraction of ipsilateral mentalis muscle. If the reaction is positive, a pursing movement of the lips occurs after each tap. Touch and pressure sensation test Light-tough sensation examined with tipped cotton applicators. The examiner touches the applicator with a light brushing motion to similar areas on two sides of the body simultaneously or just one side and ask the patient to describe the sensation perceived as left, right, or both sides. In lesions of the cortex the peripheral sensations like pain, temperature, pressure, touch, and vibration are not affected.
Treatment of this distortion of fluid-electrolyte balance is difficult: withhold diuretics, restrict water intake and give glucocorticoid which enhances excretion of water load. Diuretics should be avoided in toxaemia of pregnancy in which blood volume is low despite edema. Diuretics may further compromise placental circulation increasing the risk of miscarriage, foetal death. High ceiling diuretics and aminoglycoside antibiotics are both ototoxic and nephrotoxic; produce additive toxicity; should be used together cautiously. Cotrimoxazole given with diuretics has caused higher incidence of thrombocytopenia. Probenecid competitively inhibits tubular secretion of furosemide and thiazides: decreases their action by lowering concentration in the tubular fluid, while diuretics diminish uricosuric action of probenecid. Resistance to high ceiling diuretics Refractoriness (progressive edema despite escalating diuretic therapy) is more common with thiazides, but occurs under certain circumstances with high ceiling diuretics as well. Renal insufficiency (including advanced age) Mechanism Decreased access of diuretic to its site of action due to low g. Addition of metolazone, or to some extent a thiazide, which act on distal tubule overcome the refractoriness in many cases. Fractionation of daily dose may prevent operation of compensatory mechanisms and restart diuresis. Pharmacokinetics Acetazolamide is well absorbed orally and excreted unchanged in urine. Uses Because of self-limiting action, production of acidosis and hypokalaemia, acetazolamide is not used as diuretic. To alkalinise urine: for urinary tract infection or to promote excretion of certain acidic drugs. Epilepsy: as adjuvant in absence seizures when primary drugs are not fully effective. Aldosterone antagonist Spironolactone It is a steroid, chemically related to the mineralocorticoid aldosterone. It has no effect on Na+ and K+ transport in the absence of aldosterone, while under normal circumstances, it increases Na+ and decreases K+ excretion. Amiloride approaches the Na+ channel from the luminal side and blocks it-reducing the lumen negative transepithelial potential difference which governs K+ and H+ secretion Spironolactone is a mild saluretic because majority of Na+ has already been reabsorbed proximal to its site of action. However, it antagonises K+ loss induced by other diuretics and slightly adds to their natriuretic effect/reverses resistance to them due to secondary hyperaldosteronism. Pharmacokinetics the oral bioavailability of spironolactone from microfine powder tablet is 75%. It is highly bound to plasma proteins and completely metabolized in liver; converted to active metabolites, the most important of which is Canrenone that is responsible for 1/22/3 of its action in vivo. Use Spironolactone is a weak diuretic in its own right and is used only in combination with other more efficacious diuretics. Edema: It is more useful in cirrhotic and nephrotic edema in which aldosterone levels are generally high. Spironolactone is frequently added to a thiazide/loop diuretic in the treatment of ascitis due to cirrhosis of liver. It breaks the resistance to thiazide diuretics that develops due to secondary hyperaldosteronism and reestablishes the response. Hypertension: Used as adjuvant to thiazide to prevent hypokalaemia, it may slightly add to their antihypertensive action. More importantly, it may have the potential to attenuate hypertension related renal fibrosis and ventricular/vascular hypertrophy (see p. Aspirin blocks spironolactone action by inhibiting tubular secretion of its active metabolite canrenone. Adverse effects the side effects are drowsiness, ataxia, mental confusion, epigastric distress and loose motions.
With all forms of asbestos-induced treatment, disease is largely symptomatic and supportive. Antidotes Specific chemical antidotes for poisonings exist for only a small number of chemicals or classes of chemicals (Figure 43. The following are examples of strategies that form the basis for the use of specific chemical antidotes, with an example of how each can be applied. Pharmacologically antagonize toxic action Atropine is a muscarinic-receptor antagonist that is used as an antidote for intoxication by the anticholinesterases (see p. Accelerate detoxification of toxic agent Acetaminophen at very high doses will produce liver necrosis as a result of its metabolic activation by cytochromes P450. Administration of N-acetylcysteine will serve as a substitute for glutathione by binding to and inactivating the reactive metabolites produced from acetaminophen. To be effective, N-acetylcysteine must be given as early as possible (within 8в"10 hours of ingestion of acetaminophen). Sodium nitrite is administered to induce the oxidation of hemoglobin to methemoglobin, which has a high binding affinity for cyanide to produce cyanmethemoglobin. The second step in the antidotal treatment of cyanide intoxication is to accelerate its detoxification. Administration of sodium thiosulfate will accelerate the production of thiocyanate, which is much less toxic than cyanide and is also quickly excreted in the urine. In patients with smoke inhalation and cyanide toxicity, the induction of methemoglobin should be avoided unless the carboxyhemoglobin concentration is less than 10 percent. Reduce metabolic activation the toxicity of methanol is thought to be mediated by formic acid, which is produced by the metabolism of methanol by alcohol dehydrogenase. Fomepizole is considered an antidote to methanol, because it inhibits alcohol dehydrogenase (see Figure 43. Slowing the rate of methanol metabolism reduces the rate of rate formic acid production, thereby protecting the patient from the toxic effects of formic acid. Restore altered target Acetylcholinesterase that has been inhibited as a result of phosphorylation by organophosphorus compounds often can be reactivated by the antidote pralidoxime (see p. The chelator-metal complex is then excreted in the urine, thereby greatly facilitating the excretion of the heavy metal. Unfortunately, chelators are not specific to heavy metals, and essential metals, such as zinc, often can also be chelated. Additionally, some chelators have potentially serious adverse effects themselves, and their use in treatment of heavy metal intoxication is undertaken only when the benefits of chelation therapy outweigh the associated risks. Dimercaprol is used by itself to chelate mercury and arsenic and in combination with edetate calcium disodium to treat lead intoxication. It is not effective after oral administration and is usually given intramuscularly. Use of dimercaprol is often limited by its capacity to increase blood pressure and heart rate. Succimer: Succimer (dimercaptosuccinic acid) is a derivative of dimercaprol that is effective upon oral administration. A second advantage of succimer over dimercaprol is the lack of increased blood pressure and heart rate during treatment. Some elevation of serum levels of hepatic enzymes can be observed with succimer treatment. Succimer is currently approved for treatment of lead intoxication, but may be effective in chelation of other metals as well. Edetate calcium disodium: Edetate calcium disodium is used primarily for treatment of lead intoxication, but it can also be used for P. It is not effective after oral administration and is usually given intravenously or intramuscularly. Edetate calcium disodium can cause renal damage that is reversible upon cessation of the drug.