"Order etoricoxib now, arthritis in dogs pictures".
G. Berek, M.B.A., M.D.
Medical Instructor, Medical College of Georgia at Augusta University
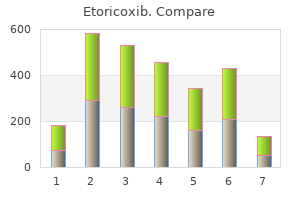
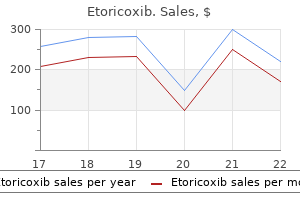
Process Solution Time Retort a) Conventional, room temperature processing schedule, 3mm biopsy. Fixation Fixation Fixation Formalin, 10% Alcoholic formalin Alcoholic formalin Alcohol, 95% Alcohol, 95% Alcohol, absolute Alcohol, absolute Xylene Xylene Paraffin Paraffin Paraffin 120 min 60 min 60 min 60 min 45 min 45 min 60 min 60 min 60 min 30 min 60 min 90 min -vacuum -vacuum -vacuum -vacuum Tissue Processing inordertoprepareatissueforembedding,itmustbeinfiltrated with paraffin. Because water and paraffin are not miscible, the specimensmustbegraduallydehydratedtoachievereplacement ofwaterwithalcoholbeforetheclearingagentisintroduced. Dehydrate Dehydrate Dehydrate Dehydrate Clearing agent Clearing agent Infiltrate Infiltrate Infiltrate 148 pecialstainsandH&e s specialstainsandH&e 149 Fixation and Tissue Processing Fixation and Tissue Processing Table 2. Embedding and Microtomy Oncethetissuehasbeenprocesseditisreadytobeorientated Solution Time Retort after sectioning, the tissue slide is drained and may be gently heatedtoevaporatethelayerofwaterbetweenthesectionsandthe glass. Dehydrate Dehydrate Dehydrate Dehydrate Dehydrate Clearing agent Clearing agent Infiltrate Infiltrate Infiltrate Alcohol, 65% Alcohol, 95% Alcohol, 95% Alcohol, absolute Alcohol, absolute Xylene Xylene Paraffin Paraffin Paraffin 15 min 15 min 15 min 15 min 15 min 15 min 15 min 15 min 15 min 15 min c) Microwave processing schedule, 1mm biopsy. Horobin, PhD Technical Considerations there are some technical tips that can apply to all preparative proceduresinmicrotechnique. Update on the immunocytochemical identification of lymphocytes in tissue sections. Blue blobs indicate the more hydrophilic structural fragments, pink blobs the more lipophilic. Structures of Oil Red O, a non-ionic, and gallocyanine chrome alum, a metal-complex ("mordant") dye, used in special stains. Unbiased samples of "normal", elastin and amyloid staining "acid" (anionic) dyes were obtained from Lillie & Fullmer (1976: being the first 10 dyes listed on page 138, and relevant dyes from page 666 and page 707 respectively). Influence of the lipophilicity (modeled by log P) of dyes on staining of fat and lipid droplets. Onecomplicationis"reactivestaining", involving making or breaking of covalent bonds, or significant oxidation-reduction changes, or formation of insoluble salts or complexes. By their pathological character Amyloid Microorganisms Viral inclusion bodies Congo red Carbol fuchsine, Giemsa and Gram stains Feulgen nucleal stain 158 pecialstainsandH&e s specialstainsandH&e 159 How Do Dyes Impart Color to Different Components of the Tissues The mobile ions are shown as nominal chloride and sodium ions, although the actual ionic species present will depend on the composition of the staining solution. Cl Na+ Basic dye Type of Component Acidophilic components How Are Targets Colored, Whilst Backgrounds Are Not Cytoplasmic protein Most permeable Collagen fibers Smooth muscle and other cytoplasms Red blood cells Basophilic components Most permeable Goblet cell mucin Chromatin Nissl substance Elastic fibres Least permeable Least permeable Case Examples Illustrating the Bases of Affinity and Selectivity asentropyeffectscontributetoaffinityinallstainingprocedures,they arenotalwaysmentioned. Acid Dyes Giving General Oversight Staining of Cells and Tissues suchdyesareanionic,varyfromsmall(picricacid,seeFigure1for structure)tomoderate. Sources of selectivity -suchdyesbindtomostproteins,and the near-universal distribution of these biopolymers results in non-selectivebackgroundcoloration. Sources of affinity - VanderWaalsattractionsbetweentBand polyanionscontributetoaffinitywhenbindingtodnaandRna,asdoes hydrophobicbonding. Sources of selectivity for mast cell granules -tBistypically appliedfromweaklyacidicaqueoussolutions. Sources of selectivity for amyloid -thestainingsolution(and/ orpre-stainingwashandpost-stainingdifferentiator,dependenton variant)istypicallyofhighpH. Sources of selectivity for calcium deposits - Backgroundacid dyeingofproteinsisreducedbythesmallconjugatedsystemsizeand hydrophiliccharacterofaRsminimisingvanderWaalsattractions andhydrophobicbonding. Sensitivity for calcium deposits - increasingpHsandstaining timesincreasesstainingintensity,sincethesemaximisethenumber ofdyephenolategroupsandaccommodatetheslowstainingreaction raterespectively. Source of selectivity for lipid - thenon-lipidcomponentsof tissues,beinglargelycomprisedofpolysaccharides,proteinsand nucleicacids,aresignificantlyhydrated. Sensitivity for lipids - triglyceridedepositsneartheirmelting pointarefluidandpermeable,andstainreadily;whereascrystalline depositssuchascholesterolremainunstainedinroutineprocedures. Bothcationicandanioniccomplexescouldbepresent; forexperimentaldataandsummaryofpriorworkseeBettinger & Zimmermann (1991) and puchtler et al (1986). Routine basic dyes readily wash out of sections if over-enthusiastically dehydratedbyalcohol,but"hematoxylin"doesnot. Raising the pH or reducing the concentration of sulfurous acid increases the sensitivity of the reagentfordetectingaldehydesbutalsoleadstoregenerationofthe originaldye.
The application of in vitro cytotoxic reactions to clinical diagnosis of food allergy. A study of the reactions of human polymorphonuclear leukocytes to various allergens. The leukocytic food allergy test: a study of its reliability and reproducibility: effect of diet and sublingual food drops on this test. Secretory otitis media and allergy: with special reference to the cytotoxic leucocyte test. An unproven technique with potentially fatal outcome: provocation/neutralization in a patient with systemic mastocytosis. A double blind, randomized, controlled investigation of electrodermal testing in the diagnosis of allergies. Is electrodermal testing as effective as skin prick tests for diagnosing allergies A double-blind, placebocontrolled study on the diagnostic accuracy of an electrodermal test in allergic subjects. An investigation of the relationship between anatomical features in the iris and systemic disease, with reference to iridology. Unreliability of Ige/IgG4 antibody testing as a diagnostic tool in food intolerance. Basidiomycete mycelia and spore-allergen extracts: skin test reactivity in adults with symptoms of respiratory allergy. Comparative studies of allergens from mycelia and culture media of four new strains of Alternaria tenuis. A major antigen of Alternaria alternata with potential for safe and effective immunotherapy of allergic patients [editorial]. Vespula vulgaris venom: role of kinins and release of 5-hydroxytryptamine from skin mast cells. Characterization and biochemical analyses of venom from the ectoparasitic wasp Nasonia vitripennis (Walker) (Hymenoptera:Pteromalidae). Allergen-specific IgE measured by a continuous random-access immunoanalyzer: interassay comparison and agreement with skin testing. Hypersensitivity to chrionomids (non-biting midges): localization of the antigenic determinants within certain polypeptide sequences of hemoglobins (erythrocruorins) of Chironomus thummi thummi (Diptera). Multicolored Asian lady beetle hypersensitivity: a case series and allergist survey. Inner City Asthma Study: relationships among sensitivity, allergen exposure, and asthma morbidity. The house dust mite (Dermatophagoides pteronyssinus) and the allergens it produces; identity with the house dust allergen. The prevalence of house dust associated environmental conditions in homes in Ohio. Antigens and allergens from the common house dust mite Dermatophagoides pteronyssinus. Detection of human IgE to sulfamethoxazole by skin testing with sulfamethoxazoyl-poly-L-tyrosine. Antigenicity of sulfanilamide and its metabolites using fluorescent-labelled compounds. Desensitization to trimethoprim sulfamethoxazole in patients with acquired immune deficiency syndrome and Pneumocystis carinii pneumonia. Diagnostic performance of Food and Drug Administration-cleared serologic assays for natural rubber latex-specific IgE antibody. Receiver operating characteristics analyses of Food and Drug Administration-cleared serological assays for natural rubber latex-specific immunoglobulin E antibody. In vivo sensitization to purified Hevea brasiliensis proteins in health care workers sensitized to natural rubber latex. Conifer pollen allergy: Studies of immunogenicity and cross antigenicity of conifer pollens in rabbit and man. An investigation of pollen extracts from different deciduous trees in patients with springtime allergy in Sweden. Detection of cross-reactive allergens in Kentucky bluegrass and six other grasses by crossed radioimmunoelectrophoresis. Study of the epitope structure of purified Dac g I and Lol p I, the major allergens of Dactylis glomerata and Lolium perenne pollens, using monoclonal antibodies.
Both of these assays suffer from the occurrence of falsenegative results, that is, patients who are clinically sensitive but exhibit negative findings to these tests. The advantages of histamine assays are that they require smaller amounts of allergen, unlike skin testing they do not involve injection of allergen into the subject, and they are not dependent on coupling antigens to immobilized support systems with the inherent problems of antigen modification or unavailability of binding sites. By contrast, using washed leukocyte experi- ments, there is no competition between IgG and IgE for antigenic binding sites, and, therefore, IgG cannot interfere in the release assays as sometimes is the case with IgE antibody serology. Histamine and its metabolite, N-methyl histamine, may be measured in urine samples (usually 24-hour collection) after a suspected anaphylactic episode or evaluation of suspected mastocytosis. Tryptase (molecular weight, 134,000 kDa) is a neutral serine esterase with trypsin-like substrate specificity that is found in relatively large quantities in mast cells (approximately 10 pg per lung mast cell and up to 135 pg per skin mast cell). It is stored in the secretory granules as an active enzyme complexed to and stabilized by heparin. Since modest amounts are found in basophils (less than 1% than found in tissue mast cells), tryptase is considered to be a good clinical marker of mast cell activation. Elevated levels of tryptase (10 g/L as measured by immunoassay) can be detected in serum from 1 to 4 hours after the onset of systemic anaphylaxis with hypotension. Recommended serum collection times for a serum tryptase are 30 minutes to 4 hours after the onset of an acute event. Although postmortem specimens are difficult to analyze for tryptase due to gross lysis of cells, levels of approximately 10 g/L in these specimens have been considered abnormal. Elevated tryptase can be detected usually within 15 to 30 minutes after an allergen challenge, and it declines with an approximate half-life of 2 hours. This is in contrast to histamine, which peaks more quickly within 5 to 10 minutes after an event and may return to baseline levels in less than 1 hour. Human Cytokine Families and Subfamilies of Special Interest to Allergy/Clinical Immunology Family I. However, since -tryptase is spontaneously secreted from mast cells and often elevated in mastocytosis patients during mast cell burden or activation, quantifying serum ratios of and provide the best indication of mast cell activation by a specific allergen. Eosinophilic cationic protein is a basic protein that can be detected in the granules of the eosinophil in different forms, with molecular weights ranging from 18. Human Chemokine Receptor and Ligand Families of Special Interest to Allergy/Clinical Immunology Family receptor I. Lymphocyte proliferative responses may be evaluated by either nonspecific mitogens (eg, phytohemagglutinin, concanavalin A, or pokeweed) or specific soluble and cell-bound antigens. Cytokine and chemokine profiles play essential roles in allergic inflammation and are being increasingly evaluated as phenotypic markers and in the differential diagnosis of human hypersensitivity disorders. Tests that quantify lymphocyte function detect the ability of lymphocytes to (1) proliferate, (2) produce inflammatory mediators and cytokines, (3) mount cytotoxic responses, and (4) regulate immune responses. Lymphocyte proliferative responses can be evaluated by the use of nonspecific mitogenic stimulants such as phytohemagglutinin, concanavalin A, or pokeweed mitogen and by specific stimuli such as soluble and cell bound antigens. The nonspecific activation of lymphocytes measures both T (ie, phytohemagglutinin, concanavalin A) and B (ie, pokeweed mitogen) cell function, although the kinetics of these responses differ. In contrast, specific antigenic challenge appears to measure only T-cell function. Cytokines and growth factors are glycoproteins produced by a variety of cells that are capable of altering activities of other cells through interaction with specific surface receptors. They have significant growth differentiation and activation functions on contiguous or distant cells and tissues. Historically, cytokines have been called lymphokines if they were produced by lymphocytes or monokines if they were produced by monocytes or macrophages. Many cytokines produced by lymphocytes have also been termed interleukins even though most of their functions are not restricted to between cells. Both immune and nonimmune cells produce chemokines and smaller proinflammatory proteins (Table 7). The elaboration of cytokines or chemokines by lymphocytes and monocytes indicates that these cells are capable of producing factors that are involved in both afferent and efferent limbs of the cellular hypersensitivity response. T-cell regulation of immunoglobulin synthesis or antibody production, as well as lymphocyte proliferation, also has clinical application. Excessive or diminished regulation of these immune responses can result in disorders associated with humoral immunity, cellmediated immunity, or both. In 1960, Nowell described that phytohemagglutinin, a lectin extracted from kidney beans, nonspecifically transformed small lymphocytes into proliferating lymphoblasts in vitro.
These patients should be immobilized in a position of comfort using towel rolls or sand bags Patient Safety Considerations 1. Be aware of potential airway compromise or aspiration in immobilized patient with nausea/vomiting, or with facial/oral bleeding 2. Excessively tight immobilization straps can limit chest excursion and cause hypoventilation 3. Prolonged immobilization on spine board can lead to ischemic pressure injuries to skin 4. Children are abdominal breathers, so immobilization straps should go across chest and pelvis and not across the abdomen, when possible 6. When securing pediatric patients to a spine board, the board should have a recess for the head, or the body should be elevated approximately 1-2 cm to accommodate the larger head size and avoid neck flexion when immobilized 7. In an uncooperative patient, avoid interventions that may promote increased spinal movement 8. There are three circumstances under which raising the head of the bed to 30 degrees should be considered: a. Promotion of patient compliance Updated November 23, 2020 212 Notes/Educational Pearls Key Considerations 1. Evidence is lacking to support or refute the use of manual stabilization prior to spinal assessment in the setting of a possible traumatic injury, when the patient is alert with spontaneous head/neck movement Providers should not manually stabilize these alert and spontaneously moving patients, since patients with pain will self-limit movement, and forcing immobilization in this scenario may unnecessarily increase discomfort and anxiety 2. Certain populations with musculoskeletal instability may be predisposed to cervical spine injury. However, evidence does not support or refute that these patients should be treated differently than those who do not have these conditions. These patients should be treated according to the Spinal Care guideline like other patients without these conditions 3. Communication barriers with infants/toddlers or elderly patients with dementia may prevent the provider from accurately assessing the patient 4. Patients who are likely to benefit from immobilization should undergo this treatment 6. Patients who are not likely to benefit from immobilization, who have a low likelihood of spinal injury, should not be immobilized 7. Ambulatory patients may be safely immobilized on gurney with cervical collar and straps and will not generally require a spine board 8. Reserve long spine board use for the movement of patients whose injuries limit ambulation and who meet criteria for the use of spinal precautions. Remove from the long board as soon as is practical Pertinent Assessment Findings 1. Comparison of outcomes for children with cervical spine injury based on destination hospital from scene of injury. Prehospital clearance of the cervical spine: does it need to be a pain in the neck Prehospital stabilization of the cervical spine for penetrating injuries of the neck - is it necessary Extrication collars can result in abnormal separation between vertebrae in the presence of a dissociative injury. Prehospital spinal immobilization does not appear to be beneficial and may complicate care following gunshot injury to the torso. A statewide, prehospital emergency medical service selective patient spine immobilization protocol. Maintaining neutral sagittal cervical alignment after football helmet removal during emergency spine injury management. The effectiveness of extrication collars tested during the execution of spine-board transfer techniques. The 6-plusperson lift transfer technique compared with other methods of spine boarding. Transferring patients with thoracolumbar spinal instability: Are there alternatives to the log roll maneuver
V infusion) 3 litres/day with 2g (26mmol) potassium chloride added to every litre bag (if renal function is satisfatory). Check for any infection and treat immediately If signs of bleeding are present give D: Vitamin K (I. V) 10mg Plus S: Fresh Frozen Plasma initially Add Platelets if count <20 x 10g/l and patient is still bleeding If ethanol etiology is suspected give: C: Thiamine (I. Note: Hepatic encephalopathy is a medical emergency and requires referral to specialized and equipped centers for proper evaluation and management. Pneumonia can either be primary (to the causing organism) or secondary to pathological damage in the respiratory system. The common causative organisms for pneumonia are bacterial (for example Streptococcus pneumoniae, Hemophilus influenza, and Staphylococcus aureus, and Mycoplasma pneumoiae, viral or parasitic. The important clinical features are high fever 39C, dry or productive cough, central cyanosis, respiratory distress, chest pain and tachypnea. Classification of pneumonia in children is based on respiratory rate whichis fast breathing and chest in-drawing. Fast breathing is defined as Respiratory rate>60 age less than 3 months Respiratory rate > 50 age between 3 months and 5 years Chest indrawing is when the lower part of the chest moves in when the child breaths in. Table 1: Important clinical features of pneumonia in underfives Age Signs Severe chest in-drawing Or 60 breaths per minute or more No severe chest in-drawing Less than 60 breaths per-minute Chest in-drawing No chest in-drawing 50 breaths per minute or more No chest in-drawing Less than 50 breaths per minute Chest in-drawing Classification Severe pneumonia (all young infants with pneumonia are classified as severe) No pneumonia: Cough or cold Severe pneumonia Pneumonia No pneumonia Cough or cold Severe pneumonia Infants less than 2 months Children from months to 1 year 2 Children from 1 year to 71 P a g e 5 year No chest in-drawing 40 breaths per minute or more No chest in-drawing Less than 40 breaths per minute Pneumonia No pneumonia Cough or cold General management Oxygen therapy if available Supportive care - Lower the temperature if 38. M once a day) for 5 days; If child responds well, complete treatment at home or in hospital with A: Amoxicillin (15 mg/kg three times a day) Plus A: Gentamicin 7. If the child does not improve within 48 hours, or deteriorates, look for complications and treat accordingly. If there are no apparent complications, switch to 72 P a g e B: Chloramphenical (25 mg/kg every 6 hours I. Non-severe pneumonia A: Amoxicillin 25 mg/kg 12 hourly for 5 days Give the first dose at the clinic and teach the mother how to give the other doses at home. The symptoms are caused by constriction of bronchial smooth muscle (bronchospasm), oedema of bronchial mucous membrane and blockage of the smaller bronchi with plug of mucus. Infants under 18 months, however, may not respond well to bronchodilator Asthma attack/ acute asthma Acute asthma is a substantial worsening of asthma symptoms. If conventional spacer not available, take a 500ml plastic bottle, insert the mouth piece of the inhaler into a hole on the bottom of the bottle (the seal should be as tight as possible). The child breathes from the mouth of the bottle in the same way as he would with a spacer 76 P a g e Silent chest Paradoxical thoracoabdominal movement Cyanosis Collapse Bradycardia arrhythmia/ adults in children hypotension or in Salbutamol nebulizer 2. O2 saturation<92% Nocturnal Asthma Patients who get night attacks should be advised to take their medication on going to bed. Chronic Asthma in Adults the assessment of the frequency of daytime and nighttime symptoms and limitation of physical activity determines whether asthma is intermittent or persistent. Therapy is step-wise (Step 1-4) based on the category of asthma and consists of: Preventing the inflammation leading to bronchospasm (controllers) Relieving bronchospasm (relievers) Controller medicines in asthma Inhaled corticosteroids. Acute bronchitis is one of the most common conditions associated with antibiotic misuse. Pertussis is the only indication for antibacterial agents in the treatment of acute bronchitis. Diagnosis Patients with acute bronchitis present with a cough lasting more than five days (typically one to three weeks), which may be associated with sputum production. Patients may get secondary bacterial infection with development of fever and production of thick smelly sputum. Non Pharmaceutical Treatment Stop smoking and/or remove from hazardous environment Prompt treatment of infective exacerbations 78 P a g e Controlled oxygen therapy Physiotherapy Bronchodilator may give some benefit Pharmaceutical Treatment Give -agonist. Chronic cough and sputum production often precede the development of airflow limitation by many years. Is confirmed by a simple test called spirometry, which measures how deeply a person can breathe and how fast air can move into and out of the lungs. Additionally, a generalized sub classification of exacerbations based on health-care utilization is proposed. Mild: patient has an increased need for medication, which he/she can manage in his/her own normal environment. Moderate: patient has an increased need for medication, and he/she feels the need to seek additional medical assistance.