"Purchase extra super avana 260 mg overnight delivery, treatment for erectile dysfunction before viagra".
M. Phil, M.A., Ph.D.
Co-Director, Boston University School of Medicine
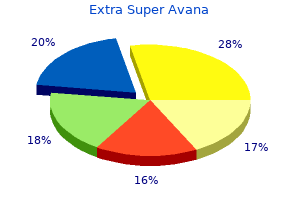
At the level of light microscopy, this boundary zone is seen as an undulating pattern of rete ridges (downward finger-like or ridgelike extensions of the epidermis) and dermal papillae (upward projections of the dermis into the epidermis) (see. Electron microscopic, immunoelectron microscopic, immunologic, biochemical, and genetic studies have elucidated the complexity of this region and are providing new insights into the pathogenesis of a variety of cutaneous diseases. Keratin filaments, hemidesmosomes, lamina lucida, lamina densa, anchoring filaments, and anchoring fibrils each function to maintain different levels of basement membrane adhesion. A variety of inherited mechanobullous diseases (epidermolysis bullosa) as well as autoimmune bullous diseases (pemphigoid, herpes gestationis, bullous systemic lupus erythematosus) involve separation and bullous formation at various levels of the dermoepidermal junction. Two to 3 million eccrine sweat glands distributed over all parts of the body surface participate in thermoregulation by producing hypotonic sweat that evaporates during heat or emotional stress (see. Each gland is a simple tubule with a coiled secretory segment deep in the dermis and a straight 2265 Figure 519-3 Structures and diseases of the dermoepidermal junction. Apocrine sweat glands in the axillae, circumanal and perineal areas, external auditory canals, and areolae of the breasts secrete viscid, milky material that accounts for axillary odor when bacteria degrade the secretion. Presumably, they are the vestigial remnants of lower species that communicate by cutaneous chemicals. Hair units, or pilosebaceous appendages, are found over the entire skin surface except on the palms, soles, and glans penis (see. Hair follicles consist of a shaft surrounded by an epithelial sheath continuous with the epidermis, the sebaceous gland, and the arrector pili smooth muscle. The bulb contains the proliferating pool of undifferentiated cells that gives rise to various layers comprising the hair and the follicle. The proliferating cells in the bulb differentiate into a hair consisting of keratinized, hard, imbricated, flattened cortex cells surrounding a central medullary space. The sebaceous glands are multilobular holocrine glands that connect into the pilosebaceous canal (hair canal) through the sebaceous duct. Germinative undifferentiated sebaceous cells at the periphery of each lobule of the gland generate daughter cells that move to the central areas of each acinus as they differentiate and form sebum (a complex oily substance composed of triglycerides and diglycerides, fatty acids, wax esters, squalene, and sterols). Most sebaceous glands adjoin a hair follicle, although some open directly on the skin surface. The sebaceous glands and certain hair follicles are androgen-dependent target organs. Follicles particularly responsive to androgen stimulation are found over the frontal and vertex areas of scalp, beard, chest, axillae, and upper and lower pubic triangles. Hair follicles are formed in early embryonic life, and no more develop after birth. Males and females have approximately the same number of hair follicles distributed over the body, but the degree of hairiness depends on two distinct features of hair growth-the hair cycle and the hair pattern. The resting hair lies high in the follicle, where it forms a stubby hair bulb that is easily shed. Growth begins with a burst of mitotic activity, and the follicle grows downward to reconstitute a new hair bulb. The hair bulb cells divide rapidly and keratinize to form a new hair shaft that dislodges the old resting club telogen hair. Regression provides a brief respite when mitosis ceases and the hair follicle pulls upward in the dermis as the hair shaft evolves into a resting club hair. In the adult scalp 85% of the hairs are in a growth state, 14% in a resting state, and 1% in regression. Considerable variation in timing of the hair cycle occurs from one region of the body to another, and the duration of growth determines the length of hairs. Hair cycles also vary with the second important feature of hair growth, namely, hair pattern or the type of hair growing in each follicle. Two types of hairs are seen: vellus hair (fine, soft, short, non-pigmented, and common on "non-hairy" areas of the body) and terminal hair (coarse, long, pigmented, and found on hairy areas of the body). The increased hairiness results from the conversion of vellus hair follicles to large terminal follicles. In the axillae and lower pubic triangle this conversion is mediated by testosterone and androstenedione.
The chronic form, adult type, accounting for about 90% of cases, occurs in older adults as an indolent illness, manifested by oropharyngeal and laryngeal mucous membrane ulcers; verrucous, ulcerative, or nodular skin lesions, often on the face or mucocutaneous borders; and enlarged or necrotic, draining lymph nodes, especially in the cervical region; pulmonary disease also occurs in the majority of patients. Other sites of less frequent involvement are the gastrointestinal tract, adrenal glands, testes, epididymis, and skeletal system. Paracoccidioidomycosis heals by fibrosis; consequently, residual fibrotic sequelae in the affected organs, despite therapy, may be incapacitating, especially in patients with pulmonary disease. Two serologic tests, immunodiffusion and complement fixation, are commonly utilized. Precipitin bands appear early in the course of active infection and may persist for years, even after successful therapy. Complement-fixing antibodies appear later and are more useful in evaluating response to treatment. In the past, oral sulfonamides were the mainstay of therapy, in large part owing to low cost; however, sulfonamides have two major drawbacks, namely, a high rate of relapse even after prolonged suppression therapy and a high frequency of adverse reactions, especially rashes. Intravenous amphotericin B is effective therapy and is usually used for more severe forms of paracoccidioidomycosis, such as pulmonary or disseminated multiorgan disease, and for more refractory cases. Oral antifungal azole drugs represent a significant advance in the treatment of this disease. Ketoconazole, an imidazole, is highly effective in both in vivo animal models and humans. Cure is usually achieved with dosages of 200 to 400 mg/day, given for at least 1 year. Itraconazole, a triazole, in a dose of 100 mg/day for 6 to 12 months, is as effective as ketoconazole and better tolerated; as a result, authorities now consider itraconazole the drug of choice for paracoccidioidomycosis. Experience in this disease with fluconazole, the other available oral triazole, has been limited. As a rule, the more common indolent forms of adult disease, usually associated with reactivation, are amenable to prolonged therapy, given over months to years. Unfortunately, clinically significant fibrotic sequelae often persist despite therapy. A comprehensive review of the disease, focusing on the causative agent, epidemiology, pathogenesis, diagnosis, and therapy, with 329 references. Itraconazole, 100 mg/day, given for a mean duration of 6 months, was highly effective, as measured by radiographic and cultural responses, falling serologic titers, and improvement in clinical severity scores. Characteristics used to distinguish the genus Cryptococcus from other yeasts include a lack of pseudohyphae, assimilation of carbohydrate and nitrate, and production of phenyloxidase, melanin, and urease. For example, strains of serotypes A and D, which include the majority of clinical isolates, can be mated to produce the perfect state (Filobasidiella neoformans var neoformans). Although humans and animals acquire infection after inhaling aerosolized spores, clusters of cases or mini-outbreaks of cryptococcosis rarely occur. Only two unusual cases of presumed person-to-person transmission of cryptococcosis have been observed. The association of cryptococcosis and organ transplantation probably relates in large part to immunosuppression with corticosteroids. However, recent data from New York City showing the annual prevalence to be between 6. After aerosolized spores are inhaled, most infections begin with an asymptomatic pulmonary focus. In individuals with normal host defense, cryptococci remain localized in the lungs and are eventually eliminated. By contrast, in immunocompromised individuals, there is hematogenous spread to extrapulmonary organs. Cryptococcal polysaccharide is a major virulence factor and may be immunosuppressive, inhibit phagocytosis, limit production of nitric oxide (an inhibitor of cryptococcal cells), and interfere with antigen presentation processes. Paradoxically, cryptococcal polysaccharide has also been shown to activate the alternative complement pathway. Other cryptococcal virulence factors include soluble constituents of the capsule (glucuronoxylomannan, galactoxylomannan, and mannoprotein), melanin, and mannitol. Although immunity in large part depends on functioning, sensitized T-cells, and an intact cell-mediated arm of host defense, anticryptococcal antibody and complement appear to be critical components of some of the cellular mechanisms. As a result, well-formed granulomas are generally absent in histopathologic sections of infected tissue. The characteristic lesion in cryptococcal meningoencephalitis consists of cystic clusters of fungi; the meninges, basal ganglia, and the cortical gray matter are the sites of heaviest involvement.
Coca. Extra Super Avana.
- Are there any interactions with medications?
- Stimulation of stomach function, asthma, colds, altitude sickness, and other conditions.
- Dosing considerations for Coca.
- Improving physical performance.
- What is Coca?
- How does Coca work?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96730
It is common in overcrowded settings and spreads rapidly in conditions in which person-to-person contact is frequent, such as in institutions for children. Embryonated eggs carried on the fingernails, bed clothing, or bedding are ingested and hatch in the upper small intestine. Female worms migrate nightly out of the rectum and deposit large numbers of ova (11,000 per worm) in the perianal and perineal areas. Larvae in the deposited eggs become infective within several hours of exposure to ambient oxygen. The vast majority of pinworm infections are asymptomatic or associated with perianal pruritus and consequent sleep deprivation. The diagnosis of pinworm infection is easily made by identifying ova on a piece of cellophane tape applied to the perirectal area in the morning. Treatment (Table 433-1) is mebendazole given to affected individuals as well as close associates, such as family members. Although personal cleanliness is recommended as a means of limiting transmission, there is no clear-cut demonstration that it prevents infection. Trichuriasis Trichuris trichiuria or whipworm infection is similar to pinworm infection in that it is limited to the gastrointestinal tract and does not have a tissue migratory phase. Ingested eggs hatch in the small bowel and subsequently develop in epithelial cells of the cecum and ascending colon into adult worms that are 40 mm in length. As is the case with most intestinal nematode infections, trichuriasis is most common in overcrowded areas with poor sanitation. The estimated prevalence worldwide is 800 million, with approximately 2 million cases in the southern United States. Children are more frequently infected than adults and also more likely to have higher worm burdens. In children with heavy infections (>10,000 eggs/g of feces), a syndrome of dysentery, growth retardation, and rectal prolapse has been described. The pathologic manifestations include infiltrates of eosinophils and neutrophils accompanied by epithelial denudation. Complicating diseases such as shigellosis and amebiasis may contribute to this condition in children. Whipworm infection is diagnosed by identification of football-shaped eggs in direct smears of fecal specimens. Mebendazole at the same dosage indicated for ascariasis listed in Table 433-1 is satisfactory treatment. Other Animal Nematodiases Humans may serve as paratenic hosts for several nematodes that ordinarily parasitize the intestine of other mammals. These helminths are incapable of completing their life cycle in humans and display aberrant migration patterns in both intestinal and non-intestinal tissues. Several species of the genus Trichostrongylus infect both humans and domestic ruminants. The adult worms live in the intestines and suck small amounts of blood; heavy infections result in anemia. Diagnosis is made by identifying ova, which resemble those of hookworm, in the stool. Most cases have been reported in Japan or Western Europe, particularly Scandinavia. The larvae invade the wall of the small intestine or stomach, causing pain and, rarely, intestinal obstruction or perforation. Gastric anisakiasis can be diagnosed endoscopically and treated by removal of the worms. Intestinal anisakiasis often resembles acute conditions that require surgery leading to laparotomy. Capillaria philippinensis infection has been reported from the Philippines and Thailand. This nematode is thought to parasitize birds, with fish and crustaceans serving as intermediate hosts. The ingested larvae mature and live in the crypts of the small intestine, where they reproduce. The result is often a heavy infection; up to 40,000 adult worms have been recovered at one autopsy. The clinical syndrome includes severe malabsorption and protein-losing enteropathy.
Lipid-associated amphotericin is theoretically attractive because the drug is delivered to macrophages, the sanctuary of leishmania. Recombinant interferon gamma with pentavalent antimony has proved effective in the treatment of patients with visceral leishmaniasis when antimony therapy alone failed. Unfortunately, some patients relapse after therapy with pentavalent antimony or other drugs, most within the first few months. Cutaneous lesions that are large or located in cosmetically important sites and those that are caused by L. Small, inconspicuous, or healing lesions caused by Leishmania species that are not associated with mucosal disease can be followed expectantly. Pentavalent antimonials, stibogluconate sodium and meglumine antimoniate, effectively treat cutaneous leishmaniasis in many situations, but, as described, they are frequently associated with toxicity and clinical failures occur. Full doses of 20 mg/kg body weight/day are recommended for 20 1963 days; lower doses may favor the development of antimony resistance. A topical formulation of paromomycin sulfate, methylbenzethonium chloride, and white paraffin has been used successfully against L. The injection of pentavalent antimony into cutaneous lesions is effective in some patients. Oral itraconazole or ketoconazole has been effective in some persons infected with L. Therapeutic failures and relapses are common among persons with diffuse cutaneous leishmaniasis or mucosal leishmaniasis who are treated with pentavalent antimony. Amphotericin B and pentamidine are effective, but toxic alternatives for those who experience failure or relapse. Recombinant interferon gamma administered with pentavalent antimony has been used effectively in a limited number of persons with diffuse cutaneous leishmaniasis. Large-scale control programs have been attempted in areas where dogs are the apparent reservoir, but their efficacy is debated. Residual insecticide spraying has been used successfully to limit disease where transmission is due to peridomestic sandflies, but it is seldom employed now because of emerging insect resistance and environmental concerns. Unfortunately, these measures are often not available for residents of endemic areas, and no vaccine is available. This is a summary of their exposures and the delay that frequently occurs in diagnosis. The epidemiologic characteristics, clinical manifestations, diagnosis, and treatment of leishmaniasis are reviewed. Visceral leishmaniasis is endemic in the Sudan, and a major epidemic has occurred there among refugees. Toxoplasma gondii is a protozoan parasite that is ubiquitous in nature and infects a variety of mammals and birds throughout the world. However, clinical and/or pathologic evidence of disease (toxoplasmosis) may occur, particularly in the immunocompromised patient, the congenitally infected fetus and child, and those in whom chorioretinitis develops during the acute acquired infection. Infection is characterized by two stages: acute (recently acquired) and chronic (latent). For information on congenital toxoplasmosis, the reader is referred to Remington and Klein (1995). There are three forms of the parasite: the tachyzoite, which is the asexual invasive form; the tissue cyst (containing bradyzoites), which persists in tissues of infected hosts during the chronic phase of the infection; and the oocyst (containing sporozoites), which is produced during the sexual cycle in the intestine of members of the cat family (the definitive host). After ingestion of tissue cysts or oocysts, bradyzoites or sporozoites, respectively, are released into the intestinal lumen, where they invade surrounding cells, become tachyzoites, and disseminate throughout the body via the blood. The tachyzoite has a crescent shape, measures approximately 3 by 7 mum, requires an intracellular habitat for survival, and can infect all mammalian cells. Continued multiplication ultimately results in destruction of the host cell and release of tachyzoites, which can then infect other cells. Tachyzoites are found in tissues during the acute stage of the infection or during reactivation of the chronic infection. Development of immunity is associated with disappearance of tachyzoites and formation of tissue cysts.