"Buy online maxolon, gastritis symptoms hemorrhage".
C. Sinikar, M.A.S., M.D.
Co-Director, Harvard Medical School
However, little is known about the signaling mechanism underlying this insulin action. The resultant enhancement in renal gluconeogenesis may at least partially contribute to hyperglycemia in these conditions. Kidney function and morphology were evaluated a week later by histological analyses. Using specific markers, we found significant reduction of cell death and enhanced proliferation in the tubules. Silenced Tie2 signaling following dysregulated expression of its ligands Angpt1 and 2 found in diabetic patients has been linked to increased mesangial expansion and glomerular scarring. Department of Nephrology, Peking Union Medical College Hospital, Chinese Academy of Medicine Sciences & Peking Union Medical College, Beijing, China. Background: Renal gluconeogenesis is substantially stimulated in patients with type 2 diabetes, but the mechanism remains unknown. After 12 weeks of treatment, blood, urine and kidney samples were collected for measurement. Conclusions: Our study demonstrated for the first time that renal gluconeogenesis is upregulated in db/db mice, and this was associated with renal inflammationmediated insulin resistance. This work shed light on the role of inflammation in enhanced renal gluconeogenesis and may yield a novel target for hyperglycemia. Furthermore, the effects of 18E1 mAb in glomerular endothelial cell and podocyte cell proliferation were also assessed in culture. Specifically targeting pNaKtide to the adipocytes with lenti-adipopNaKtide ameliorates this systemic effect. This new information is important in the development of new therapeutic targets for obesity. We have previously reported that telomerase deficiency may predispose to diabetic renal injury. Blood glucose, Creatinine clearance (Ccr) and urinary protein were measured at 0, 4, 8 weeks. It has been demonstrated that oxidative stress can exacerbate obesity development. Adipocyte dysfunction may be prevented by lentiviral mediated adipocyte-specific delivery of pNaKtide. Lentiviral constructs with pNaKtide driven by an adiponectin promoter were used to achieve pNaKtide expression specifically in adipose tissue. Glucose clearance was determined using an intraperitoneal glucose tolerance test before termination of the experiment. At sacrifice body weight, visceral and subcutaneous fat content of all mice were measured. Renal function was not significantly impacted; slight decreases in function are evident, suggesting a potential decrease in renal function with chronic obesity. We are also following up these patients to investigate the renal and cardiovascular outcomes of the different phenotypes. Methods: At the end of the study, participants were asked to join passive followup with electronic data abstraction through 9/30/14. Conclusions: Overall, there was not an apparent long-term benefit or harm for combination therapy. Methods: Prospective, randomized, double-blind, placebo-controlled multicentre clinical trial and observational study in normoalbuminuric type 2 diabetic patients. Patients in the high risk group are assigned to spironolactone 25 mg once daily or placebo, the low-risk group is followed on standard care. Baseline characteristics of the overall study cohort and by subgroup Body Fat Distribution Is More Predictive of All-Cause Mortality Than Overall Adiposity Sung Woo Lee,1 Nam ju Heo. Background: the relationship between directly measured body fat and all-cause mortality has been rarely studied. Of those, 32,593 participants with data regarding vital status as of May 2016 were included in the final analysis. This suggests that the location of fat deposits may be more important than the actual amount of body fat. Sensitivity analyses incrementally adjusted for broad categories of anti-diabetic medications (insulin, oral medications) as well as specific categories (biguanides, thiazolidinediones, alpha-glucosidase inhibitors, insulin, insulin secretors, other oral medications).
The greatest exposure can occur from eating food (eg fruits and vegetables) since its easily taken up by plants through the roots. Accidental ingestion may lead to vomiting, diarrhea, and leg pains followed by a severe and sometimes fatal sensorimotor polyneuropathy. Most thallium is excreted in the urine and can be found within an hour after exposure and be detected as long as two months after exposure. Useful For: Detecting toxic thallium exposure in 24-hour urine specimens Interpretation: Patients exposed to high doses of thallium (>1 g) present with alopecia, peripheral neuropathy, seizures, and renal failure. Reference Values: 0-17 years: not established > or =18 years: <2 mcg/24 hours Clinical References: 1. Agency for Toxic Substances and Disease Registry: Toxicological profile for thallium. Useful For: Detecting toxic thallium exposure in whole blood specimens Interpretation: Normal blood concentrations are less than 1 ng/mL. Significant exposure is associated with thallium concentrations in blood greater than 10 ng/mL, and as high as 50 ng/mL. Patients exposed to high doses of thallium (>1 g) present with alopecia (hair loss), peripheral neuropathy, seizures, and renal failure. Reference Values: 0-17 years: not established > or =18 years: <2 ng/mL Clinical References: 1. Pelcloval D, Urbanl, P, Ridsonl P, et al: Two-year follow-up of two patients after severe thallium intoxication. Useful For: Detecting toxic thallium exposure in random urine specimens Interpretation: Patients exposed to high doses of thallium (>1 g) present with alopecia, peripheral neuropathy, and seizures, and renal failure. Pelclova D, Urban P, Ridson P, et al: Two-year follow-up of two patients after severe thallium intoxication. Zhao G, Ding M, Zhang B, et al: Clinical manifestations and management of acute thallium poisoning. Campanella B, Colombaioni L, Benedetti E, et al: Toxicity of thallium at low doses: A review. Activated protein C downregulates further thrombin generation, suppressing clot formation. Despite its role in coagulation, it is unclear whether thrombomodulin gene alterations play a significant role in venous thromboembolism (5). A set of clinical guidelines from the British Society for Haematology on testing for heritable thrombophilia (1) is freely available. There is somewhat stronger evidence of an association between thrombomodulin gene polymorphisms and a moderately increased risk for arterial thrombosis, although more studies including a larger number of patients are needed to more firmly establish this risk (5). A systematic diagnosis through conventional coagulation testing is recommended prior to considering genetic testing for any suspected bleeding disorder. Evaluation and categorization of variants is performed using the most recent published American College of Medical Genetics and Genomics recommendations as a guideline. Ariceta G, Besbas N, Johnson S, et al: Guideline for the investigation and initial therapy of diarrhea-negative hemolytic uremic syndrome. Delvaeye M, Noris M, De Vriese A, et al: Thrombomodulin mutations in atypical hemolytic-uremic syndrome. Anastasiou G, Gialeraki A, Merkouri E, et al: Thrombomodulin as a regulator of the anticoagulant pathway: implication in the development of thrombosis. Theophylline is typically administered orally at a dose of 400 mg/day or 6 mg/kg, whichever is lower, or intravenously as aminophylline at 0. Theophylline has a half-life of approximately 4 hours in children and adult smokers, and 8. Coadministration of cimetidine and erythromycin will significantly inhibit theophylline clearance, requiring dosage reduction.
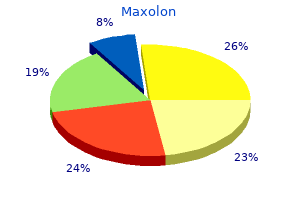
Forty percent had received organ transplants: 33% liver and 7% liver + kidney; 83% of transplant patients received tacrolimus for immunosuppression. Sixty-seven percent of patients received elbasvir/grazoprevir, 20% elbasvir/grazoprevir + ribavirin, and 13% ledipasvir/sofosbuvir. One patient received additional erythropoietin during dialysis and had a ribavirin dose reduction. With this high incidence we decided to run a prospective improvement trial to reduce the incidence Methods: We conducted a random survey for 60% of patients to determine daily practice. Based on the data, procedure check list created during monthly visits and re-training at same time. Regular home visit assessment and questionnaire taking for environmental evaluation and daily practice. Results: 110 Patients took part in the survey and after analysis of the data using pareto chart, 24% had poor hand hygiene, 22% not using mask, 20% had constipation, 14% had an unsuitable environment at home, 8% had poor personal hygiene, 7% traveled abroad and 5% did not have adequate time to undertake the procedure properly. The incidence of peritonitis in the 6 months of the trial has fallen from average 4% to 1. Although there is medical and economical benefit, there is some cost implication for the monthly retraining. More work is needed to establish what would be the most effective frequency of training Funding: Government Support - Non-U. Results: A total of 1814 samples were obtained, the more prevalent bacteria were Staphylococcus coagulasa negative (ConN) (23. The distribution of agents according to Gram stain between the years studied were no different (p=0. The prevalence of Vancomycin resistant Enterococcus was 18%, with no difference between acquisitions on community or nosocomial setting. Surprisingly there were no differences between the resistance and the ambulatory or hospital setting of the infection. Conclusions: the agents responsible of peritonitis during this 8 year study were primarily Gram positive coccus, with a high prevalence of methicillin resistance in both ambulatory and nosocomial setting. Services Associated with Increased Cost of Hospitalization for Peritonitis in Pediatric Patients Receiving Chronic Peritoneal Dialysis Allison C. Background: Peritonitis is a leading cause of hospitalization in children on chronic peritoneal dialysis. The objective of this analysis is to describe service-line utilization associated with high-cost hospitalizations for peritonitis. Linkage was performed on the basis of sex, birth month and year, and date of peritonitis episode and hospitalization. Detailed billing information was used to compare service-line utilization among the top 25 % of infection episodes by cost with bottom 75% and to compare fungal infection episodes to other types of infections. Detailed billing data was available for 246 hospitalizations and 238 peritonitis episodes. The proportions of hospitalization costs were similar between the top 25% of peritonitis episodes (N=66) and the lower 75% (N=180) for pharmacy (p=0. Compared with other types of infections (N=215), fungal peritonitis episodes (N=23) had elevated costs per episode (p<0. Conclusions: the increase costs attributed to the top 25% of peritonitis hospitalizations can be attributed to all service lines. Background: Guidelines that recommend specific antibiotics for empiric treatment of peritonitis are not specific to populations and time variable microbiology. The inclusion criteria were all adult living donor kidney transplants performed between 2004 and 2015. Data from pediatric recipients (<18 years) and donors with pre-existing renal pathology (n=404), with incomplete data (n=46) and those with early graft loss (graft loss within 1 week of implantation) (n=38) were excluded. Attention towards minimization of ischemia time in high-risk patients is recommended. Background: We tested a multi-platform approach for the noninvasive differential diagnosis of acute dysfunction of the kidney allograft. Methods: We studied 118 kidney transplant recipients with acute kidney allograft dysfunction. Using these three transcript levels, we derived our 3-gene molecular signature (Suthanthiran et al.
Efficacy of Steroid Therapy for IgA Nephropathy Yasuyuki Nagasawa,1 Ryohei Yamamoto,6 Maki Shinzawa,6 Tatsuya Shoji,4 Katsuyuki Nagatoya,5 Terumasa Hayashi,4 Yukiko Hasuike,1 Takahiro Kuragano,3 Atsushi Yamauchi,5 Toshiki Moriyama,7 Yoshitaka Isaka,6 Takeshi Nakanishi. Background: IgA Nephropathy is most common primary glomerular nephritis not only in Asian, but also in Caucasians. But, IgA nephropathy patients with low proteinuria and with normal kidney function were known to have good prognosis. There was favorable effect by steroid upon renal progression in the IgA patient whose proteinuria was more than 60mL/ min/1. Two independent factors of severe manifestation at the time of biopsy were high blood pressure and high score of tubulointerstitial involvement. Methods: Thirty adult patients with a sole diagnosis of IgA nephropathy were included in this study. Patients were excluded if they had received glucocorticoids or immunosuppressant therapy before renal biopsy. The histological classification was scored according to the Oxford classification. The available data came from few medical schools, which might not represent the entire Thai population. The clinical and renal pathology characteristics, treatment regimens at the time of renal biopsy were obtained via online data collection forms. All adverse events were mild with headache and sinus congestion considered possibly related by the investigator. Despite their relatively high prevalence, limited data exist describing their natural histories. Inclusion criteria were diagnosis before age 18 years, minimum 1-year of follow-up, and absence of pre-existing renal disease. At 1-year follow-up, there were no differences in clinical features or immunosuppressant use. Demographics and clinical features Long-Term Outcome of Pneumococcal Haemolytic Uraemic Syndrome Aoife Waters. Additional information pertaining to mortality and co-morbidties were also collected. Results: Long-term outcome data was available for 16 of 38 patients who were previously reported1. At time of follow up, none were on dialysis but three patients [18%] had received renal transplants without recurrence. Those with nephrotic-level proteinuria had crescents (73%), M1 (73%), E1 (86%), S1 (13%), and T1 (13%). Patients with M1 vs M0 were more likely to have higher urine p/c at follow-up (p=0. Of patients with >10% crescents, 92% received steroids and 79% received immunosuppression. Patients were stratified by treatment approach: targeted to detected clonal cell type or non-targeted. A paraprotein was detected in serum or urine in 8 patients and an underlying clone was detected in 7 patients (B cell n=2, plasma cell n=3, lymphoplasmacytic cell n=2); 5 of these patients received clonedirected therapy. Among those who responded, median time to any renal response was 98 days in bortezomib-treated patients vs. Future studies should explore more sensitive methods for detecting an underlying pathogenic clone to direct treatment. These data including the demographic data and laboratory data together with kidney biopsy pathological findings. Results: the 276 from 1,556 patients were recruited in this study; 123 cases were male (44. However, kidney biopsy is still the important means for the definite diagnosis of glomerular disease in diabetic patients.
You can also donate your own blood before the procedure, or have family members donate if you prefer. This surgery is done under general anesthesia, so patients meet with an anesthesiologist before the procedure and are asked questions about their medical history. This is an open surgery, which means the skull is cut and microsurgery is performed. Part of the preparation for this surgery may include shaving a section of the hair on your head. The neurosurgeon makes an incision behind the hairline or on the back of the head, depending on the location of the aneurysm. From there a section of bone, or bone plate, is removed (craniotomy) from the skull to expose the brain tissue. Under a microscope, the aneurysm is carefully separated from the normal blood vessels and the brain, so the neurosurgeon can see it and properly treat it. With the clip in place, the aneurysm is totally sealed off, and no more blood can enter it. Aneurysms that are quite large or involve a large section of the blood vessel may require special procedures, such as putting clips on either side of the aneurysm or making a bypass around the aneurysm. After the surgery, you will wake up somewhat cold and slightly dizzy, and amazed that it is all over. What will surprise you is how little you remember of the day of the operation, and how well you feel the next day. Patients treated for an unruptured aneurysm will leave the hospital within a few days, while patients treated for a ruptured aneurysm will usually leave the hospital within two weeks. Instead of open surgery, the aneurysm is accessed via a catheter inserted in an artery (usually in the groin) and treated by inserting various devices (coils, stents, balloons, flow diversion devices) or liquid agents that prevent blood from flowing into the aneurysm. The goal of endovascular therapy is the same as surgical treatment: to prevent rupture by safely sealing off the aneurysm from its parent artery. Available since about 1990, endovascular treatment was initially used to treat aneurysms that could not be treated with surgery. The field has developed rapidly so that now endovascular treatment is used as the primary treatment method at many medical centers. Your doctor will discuss the risks and benefits of endovascular treatment with you and your family and answer any questions you may have. Coiling Procedure Endovascular treatment of aneurysms is most often performed in an angiography suite by a specialized team of doctors, nurses, and technologists. An interventional neuroradiologist or neurosurgeon trained in interventional neuroradiology is the primary doctor during the procedure. At the time of the procedure, your groin is scrubbed and shaved, usually on both sides. Sterile drapes and cloths are placed over your body, leaving the groin area exposed. A small skin incision, measuring approximately 6 mm (a dime is 18 mm), is made over the artery and a needle is used to puncture the blood vessel. Using X-ray visualization and high-speed filming techniques that provide a continuous view of the normal blood vessels and aneurysm, the doctor inserts a catheter, led by a guide wire, and advances it to the site of the aneurysm. Through the catheter, a smaller microcatheter is advanced into the aneurysm opening and the coil system is introduced. The coil system consists of different materials, most commonly platinum and sometimes other gel-like and suture-like materials. The coils are soft and pliable, and are available in several sizes and shapes to fit correctly inside an aneurysm. While inside the catheter, the coil is straight, but when the coil exits the catheter, it takes on a spiral shape, conforming to the shape of the aneurysm. The coil (or coils, as sometimes more than one is needed) prevents blood from flowing into the aneurysm. Coil Used with the permission of Mayo Foundation for Medical Education and Research.