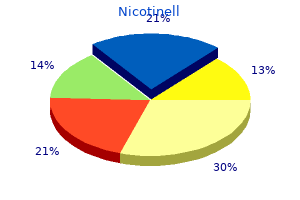
"52.5mg nicotinell for sale, quit smoking body effects".
R. Ernesto, M.S., Ph.D.
Co-Director, Indiana University School of Medicine
Delayed onset is most often seen with premature infants and occurs within the first 3 months of age. Sequelae or relapse in infancy through adolescence of a previously undiagnosed infection occurs in 24% to 85% of infected patients. The peak presentation of chorioretinitis from congenital infection occurs between the ages of 15 to 20 years. Hydrocephalus, chorioretinitis, and intracranial calcifications are the classic triad, but disease is usually a clinical spectrum. The neonate may have evidence of endocrine dysfunction or difficulties with temperature regulation depending on the areas of the brain that are affected. Active encephalitis and obstructive hydrocephalus from edema and inflammation may respond well to treatment. Toxoplasmosis is one of the most common causes of chorioretinitis and can lead to visual impairment. Other manifestations include phthisis (destruction of the globe), retinal detachment, optic atrophy, iritis, scleritis, uveitis, and vitreitis. Other common symptoms include hepatosplenomegaly, persistent conjugated hyperbilirubinemia (from liver damage or hemolysis), and thrombocytopenia. Rare presentations include erythroblastosis and hydrops fetalis, myocarditis, pneumonitis, and nephritic syndrome. Monozygotic twins often have similar patterns of infection in contrast to dizygotic twins. Other disorders to be considered include hepatitis B, varicella, bacterial sepsis, hemolytic diseases, metabolic disorders, immune thrombocytopenia, histiocytosis, and congenital leukemia. IgG appears within 1 to 2 weeks, peaks at 1 to 2 months, and persists throughout life. For patients with seroconversion or a fourfold rise in IgG antibody titer, perform IgM testing. Because IgM and IgA do not cross the placenta, they are useful in determining congenital infection. If maternal blood contamination is possible, repeat the IgM, IgA, and IgE testing in a few days. In infants who are IgM and IgA negative, the traditional means of diagnosis is to wait for clearance of transplacental IgG at about 12 months of age. IgA rises rapidly, and it usually disappears by 7 months (uncommonly, more than 1 year). In congenital toxoplasmosis, antibody production varies significantly and is affected by treatment. The Sabin-Feldman dye test (IgG) uses the uptake of methylene blue by Toxoplasma tachyzoites (organisms appear swollen and blue). The tachyzoite membranes lyse in the presence of complement and IgG-specific antibody (organisms appear thin and unstained). There is extensive experience with this test, particularly as an antenatal screen for maternal seroconversion in pregnancy. Persistence of Toxoplasma-specific immunoglobulin (IgM) may indicate active infection. Toxoplasma-specific IgG has been seen, and quantitative IgG levels should be determined as a baseline. They may be single or multiple and are usually limited to intracranial structures. Common locations include periventricular, scattered in the white matter, and the basal ganglia (often caudate). Histology may demonstrate tachyzoites (acute toxoplasmosis) or cysts (acute or chronic toxoplasmosis) in the placenta, tissue, or body fluids. Tissue or mouse culture can be performed to isolate the parasite from peripheral blood buffy coat or the placenta, but may require 1 or 6 weeks, respectively, for results. Congenital infection is frequently subclinical, has symptoms similar to other infections and diseases, and serologic diagnosis may be difficult.
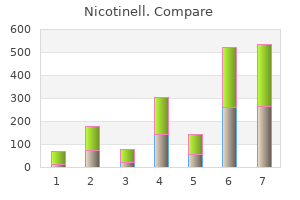
A dichorionic diamniotic placenta results when early splitting occurs at day 0 to 3 before chorion formation (which usually occurs about day 3) and before implantation. A monochorionic diamniotic placenta results when splitting occurs about day 4 to 7, at which time the blastocyst cavity has developed and the chorion has formed. Amnion formation occurs at day 6 to 8, and splitting of the egg after this time (day 4 to 7) results in a monochorionic monoamniotic placenta. At day 14 and thereafter, the primitive streak begins to form, and late splitting of the embryo at this time results in conjoined twins. Multiple gestational sacs can be detected by ultrasonography as early as 5 weeks and cardiac activity can be detected from more than one fetus at 6 weeks. First-trimester ultrasonography can best determine the chorionicity of a multiple gestation; chorionicity is more difficult to determine in the second trimester. From weeks 10 to 14, a fused dichorionic placenta may often be distinguished from a true monochorionic placenta by the presence of an internal dividing membrane or ridge at the placental surface (lambda sign). The dividing septum of a dichorionic placenta appears thicker and includes two amnions and two chorionic layers. In contrast, the dividing septum of a monochorionic placenta consists of two thin amnions. One placenta, same-sex fetuses, and absence of a dividing septum suggest monoamniotic twins, but absence of a dividing septum may also be due to septal disruption. Pathologic examination of the placenta(s) at birth is important in establishing and verifying chorionicity. Zygosity determines the degree of risk of chromosomal abnormalities in each fetus of a multiple gestation. Second-trimester maternal serum screening for women with multiples is limited because each fetus contributes variable levels of these serum markers. First-trimester ultrasonography to assess for nuchal translucency is a more sensitive and specific test to screen for chromosomal abnormalities. A secondtrimester ultrasonography exam is important in surveying each fetus for anatomic defects. Gestational diabetes has been shown in some studies to be more common in twin pregnancies. Spontaneous abortion occurs in 8% to 36% of multiple pregnancies with reduction to a singleton pregnancy by the end of the first trimester ("vanishing twin"). Possible causes include abnormal implantation, early cardiovascular developmental defects, and chromosomal abnormalities. Before fetal viability, the management of the surviving co-twin in a dichorionic pregnancy includes expectant management until term or close to term, in addition to close surveillance for preterm labor, fetal well-being, and fetal growth. The management of a single fetal demise in a monochorionic twin pregnancy is more complicated. The surviving co-twin is at high risk for ischemic multiorgan and neurologic injury that is thought to be secondary to hypotension or thromboembolic events. Termination of pregnancy may be offered as an option when single fetal demise occurs in a previable monochorionic twin pregnancy. In a large retrospective cohort study, the incidence of placental abruption was 6. Preterm premature rupture of membranes complicates 7% to 10% of twin pregnancies compared with 2% to 4% of singleton pregnancies. Preterm labor and birth occur in approximately 57% of twin pregnancies and in 76% to 90% of higher order multiple gestations. Approximately 66% of patients with twins and 91% of patients with triplets have cesarean delivery. Breech position of one or more fetuses, cord prolapse, and placental abruption are factors that account for the increased frequency of cesarean deliveries for multiple gestations. The average duration of gestation is shorter in multifetal pregnancies and further shortens as the number of fetuses increases. The mean gestational age at birth is 36, 33, and 29 and one-half weeks, respectively, for twins, triplets, and quadruplets. The likelihood of a birth weight 1,500 g is 8 and 33 times greater in twins and triplets or higher order multiples, respectively, compared with singletons. In two multicenter surveys, multiples occurred in 21% to 24% of births 1,500 g and in 30% of births 1,000 g. The mechanisms are likely uterine crowding, limitation of placental perfusion, anomalous umbilical cord insertion, infection, fetal anomalies, maternal complications.
If severe or prolonged, an episode of peritonitis may prompt removal of the peritoneal catheter or even discontinuation of the modality. Results are best with living-related transplantation, in part because of optimized tissue matching and in part because waiting time can be minimized. Rejection Immunologic rejection is the major hazard to the short-term success of renal transplantation. Rejection is characterized by a rise in serum creatinine, hypertension, fever, reduced urine output, and occasionally graft tenderness. Immunosuppression Maintenance immunosuppressive therapy usually consists of a three-drug regimen, with each drug targeted at a different stage in the immune response. Side effects of cyclosporine include hypertension, hyperkalemia, resting tremor, hirsutism, gingival hypertrophy, hyperlipidemia, hyperuricemia, and a slowly progressive loss of renal function with characteristic histopathologic patterns (also seen in exposed recipients of heart and liver transplants). While the side effect profile of tacrolimus is generally similar to cyclosporine, there is a higher risk of hyperglycemia, a lower risk of hypertension, and occasional hair loss rather than hirsutism. The major side effects of mycophenolate mofetil are gastrointestinal (diarrhea is most common), and leukopenia (and thrombocytopenia to a lesser extent) develops in a fraction of patients. Sirolimus is a newer immunosuppressive agent often used in combination with other drugs, particularly when calcineurin inhibitors are reduced or eliminated. Other Complications Infection and neoplasia are important complications of renal transplantation. Bacterial: infective endocarditis, "shunt nephritis," sepsis, pneumococcal pneumonia, typhoid fever, secondary syphilis, meningococcemia 2. Dx depends on a positive pharyngeal or skin culture, rising antibody titers, and hypocomplementemia. In most cases the disease is self-limited, although the prognosis is less favorable and urinary abnormalities are more likely to persist in adults. Examples are bacterial endocarditis, sepsis, hepatitis B, and pneumococcal pneumonia. Similar features plus palpable purpura and asthma are common in hypersensitivity angiitis. Combinations of glucocorticoids in pulsed doses, cyclophosphamide, and intensive plasma exchange may be useful, although few prospective clinical trial data are available. Complications include renal vein thrombosis and other thromboembolic events, infection, vitamin D deficiency, protein malnutrition, and drug toxicities due to decreased protein binding. Renal vein thrombosis is relatively common, more so than with other forms of nephrotic syndrome. Primary tends to be more acute, similar to minimal change disease in abruptness of nephrotic syndrome, but with added features of hypertension, renal insufficiency, and hematuria. Clinical history, kidney size, and associated conditions usually allow differentiation of primary vs. If hyperkalemia develops and cannot be controlled with (1) optimizing glucose control, (2) loop diuretics, or (3) occasional polystyrene sulfonate (Kayexalate), then tight control of blood pressure with alternative agents is warranted. Episodes of macroscropic hematuria are present with flulike symptoms, without skin rash, abdominal pain, or arthritis. Diuretics, non-dihydropyridine calcium antagonists, and -adrenergic blockers have been successfully used in a variety of clinical settings. Compared with glomerulopathies, proteinuria and hematuria are less dramatic, and hypertension is less common. Renal dysfunction usually improves after withdrawal of the offending drug, but complete recovery may be delayed and incomplete. In uncontrolled studies, glucocorticoids have been shown to promote earlier recovery of renal function. Proximal bicarbonate wasting Failure of proximal tubule protein reabsorption Damage to medullary tubules and vasculature Potassium secretory defects including aldosterone resistance Distal tubular damage with impaired sodium reabsorption Common. It is thought to be a more common cause of end-stage renal disease in Australia/New Zealand than elsewhere owing to the larger per capita ingestion of analgesic agents in that region of the world.
Infection is a risk, particularly with scalp lesions and an underlying caput succedaneum or hematoma. It usually presents during the first 2 weeks after birth as sharply demarcated; irregularly shaped; firm; and nonpitting subcutaneous plaques or nodules on the extremities, face, trunk, or buttocks. The High-Risk Newborn: Anticipation, Evaluation, Management, and Outcome Vincent C. The placenta should be saved after delivery in all cases of high-risk delivery, including cases that involve transfer from the birth hospital, since an elusive diagnosis such as toxoplasmosis may be made on the basis of placental pathology. Stillbirth, asphyxia, meconium aspiration syndrome, persistent pulmonary hypertension. Immediately evident neonatal conditions and associated risk for fetus or neonate 1. To confirm or supplement obstetric dating, the modified Dubowitz (Ballard) examination for newborns. There are limitations to this method, especially with use of the neuromuscular component in sick newborns. Although there is no universal agreement, the commonly accepted definitions are as follows: 1. As noted above, a preterm neonate is one whose birth occurs before the end of the 37th week (258th day; i. The distribution of this group is gradually shifting to a relatively older gestational age because of a 25% increase in late preterm infants (34 to 36 weeks) since 1990 to current rate of 9. Non-Hispanic black women are more than three times as likely to deliver an extremely preterm infant (28 weeks of gestation) (1. Acute or chronic maternal illness is associated with early delivery, whether spontaneous or, not infrequently, induced. Multiple-gestation births frequently deliver preterm (60% of twins and 94% of triplets in the United States in 2005). In such births, higher rate of neonatal mortality is primarily due to prematurity. Obstetric factors such as uterine malformations, uterine trauma, placenta previa, abruptio placentae, hypertensive disorders, preterm cervical shortening, previous cervical surgery, premature rupture of membranes, and chorioamnionitis also contribute to prematurity. Problems of preterm birth are related to difficulty in extrauterine adaptation due to immaturity of organ system. Perinatal depression in the delivery room due to poor transition to breathing (see Chaps. Preterm infants have a higher risk for neurologic problems, including the following: a. Preterm infants may present with cardiovascular problems, including the following: a. Patent ductus arteriosus is common and may lead to pulmonary overcirculation and diastolic hypotension (see Chap. Preterm infants require specific attention to the content, caloric density, volume, and route of feeding (see Chap. Premature infants are at increased risk for necrotizing enterocolitis; formula feeding is an additional risk factor; breast milk appears to be protective (see Chap. Problems, especially in glucose and calcium metabolism, are more common in preterm infants (see Chaps. Immature kidneys are characterized by low glomerular filtration rate, as well as an inability to handle water, solute, and acid loads. Preterm infants are especially susceptible to hypothermia and hyperthermia (see Chap. Because of deficiencies in both humoral and cellular response, preterm infants are at greater risk for infection than are term infants. Retinopathy of prematurity may develop in the immature retina of infants 32 weeks or with birth weight 1,500 g (see Chap.