"Generic periactin 4mg mastercard, allergy testing valdosta ga".
C. Vibald, M.B.A., M.D.
Medical Instructor, University of California, Davis School of Medicine
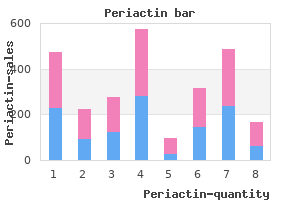
The papillary variety is also more common in this location than in other parts of the bile duct. Except in the case of the papillary variety of this cancer, patients are brought to the operating room with the diagnosis of periampullary cancer, and it is in the final pathologic analysis that the anatomic site of origin of the tumor becomes clear. The importance of distinguishing distal bile duct cancer from the other periampullary tumors is in the prognostic implications, as distal bile duct cancer has a much more favorable outcome than does the more common adenocarcinoma of the pancreas. Jaundice is the presenting symptom in up to 90% of patients with distal bile duct cancer. Abdominal pain, weight loss, fever, or pruritus are also common symptoms, though these occur in one-third of cases or fewer. Most often, however, the symptoms and signs will be indistinguishable from adenocarcinoma of the pancreatic head or other periampullary malignancies. Endoscopic brush biopsy has a low sensitivity, making a negative result virtually useless. In patients with a stricture of the distal bile duct and a clinical presentation consistent with cholangiocarcinoma, cross-sectional imaging studies are scrutinized for signs of unresectable cancer. Biliary obstruction then can also be treated by endoscopic stenting or, if necessary, through percutaneous transhepatic stenting to avoid surgery. Treatment Options Complete resection is the only effective and potentially curative therapy for cancers of the lower bile duct. The results of resection for distal bile duct cancer as compared to the other periampullary tumors are demonstrated in Figure 33. The results are similar to those for duodenal cancer, more favorable than those for adenocarcinoma of the pancreas, 293,304 and less favorable than those for neuroendocrine or ampullary tumors. Five-year survival rates of up to 40% have been reported after complete resection (Table 33. It has long been assumed that survival after resection of distal bile duct tumors is more favorable than after resection of hilar cholangiocarcinomas, 292 but this commonly held belief has been refuted by data. Though it is true that resectability rates are higher for distal bile duct cancers and the likelihood of achieving a negative margin during resection is greater, the survival rates of the various bile duct tumors, if adjusted for stage and completeness of resection, appear to be comparable. Survival after Resection of Distal Cholangiocarcinoma Because of the rarity of distal cholangiocarcinoma, no prospective data are available to guide the use of adjuvant therapy after resection. In patients with nonresectable cancers, palliation for biliary obstruction can be achieved with a surgical bypass or biliary endoprostheses. Endoprostheses for distal biliary obstruction are usually placed endoscopically and provide more durable palliation than does an endoprosthesis placed for hilar obstruction. In our practice, patients found to have unresectable disease at laparotomy are subjected to surgical bypasses, as they will already have incurred the risk of anesthesia and laparotomy. Furthermore, patients expected to survive longer than 6 months are also considered for surgical bypass. Chemotherapy or radiotherapy or both have offered generally poor results as palliative treatment for unresectable cases. Of the hepatobiliary tumors, these cholangiocarcinomas represent the greatest diagnostic and therapeutic challenge because of the vast number of vital structures that can be involved by even a small hilar cholangiocarcinoma. Proximal or hilar cholangiocarcinomas require the most extensive of liver resections and vascular reconstruction for extirpation. Most patients with cholangiocarcinoma come to medical attention because of jaundice or abnormal liver function tests. Abdominal pain or discomfort, anorexia, weight loss, and pruritus are the most common symptoms but are seen in only approximately one-third of patients. Intermittent jaundice may be seen with papillary tumors and is usually due to intermittent detachment of pieces of friable tumors from the right or left hepatic duct that pass into and occlude the common hepatic duct. The serum bilirubin level is usually greater than 10 mg/dL and averages 18 mg/dL, whereas bilirubin levels of 2 to 4 mg/dL are the norm in patients with obstruction from choledocholithiasis. Proximal biliary obstruction is usually associated with a decompressed and nonpalpable gallbladder.
Syndromes
- X-ray of the bile ducts (cholangiogram)
- Injury to nerves or blood vessels.
- If the top number (systolic number) is greater than 130 or the bottom number (diastolic number) is greater than 85, call your doctor.
- Makes vowel sounds ("oo," "ah")
- Rash on the breast
- Muscle stiffness in face or neck
- Prepare your home for after the surgery
- Mongolian blue spots
- Rash
- Provide safe copies of adult tools and equipment. Many children like to mimic activities such as cutting the grass or sweeping the floor.
The destructive process may be facilitated by thrombosis of small vessels and the resulting tissue anoxia. The ice balls generated by current methods are elliptic in shape, with the maximal radius at the tip. Therefore, it is frequently necessary to pull the cryoprobes back toward the apex of the prostate after the initial freezing at the base, to ensure complete destruction of the gland. Patients, after induction of regional or general anesthesia, are placed in the lithotomy position. A urethral warming device is placed to preserve the urethra and avoid sloughing of tissue postoperatively. An ultrasound transducer is inserted into the rectum, and volume measurements are made of the prostate and cancer or cancers. Cannulas and dilators are passed over the wires to facilitate placement of five or more cryoprobes. Generally, two probes are placed anteromedially, two posterolaterally, and one posteriorly. Liquid nitrogen is circulated through these needles, and the resulting freezing zones, or ice balls, can be monitored by ultrasonography. The anterior probes are activated first and allowed to extend posteriorly and laterally. Once these have reached the desired position, thawing is begun, and the posterior probes are activated. Most often, two freeze-thaw cycles are performed, certainly in the area of cancer. In addition, if the ice ball does not adequately extend to the apex of the prostate, the cryoprobes are pulled backward into the apex, and additional freezing is carried out. Androgen deprivation before cryosurgery should be considered in patients with large glands or extensive local disease, as such therapy serves to shrink the prostate and cancer, allows for even distribution of the cryoprobes, eliminates steep temperature gradients between the probes, reduces bulky extracapsular disease, and may allow for widening of the periprostatic space and better protection of surrounding structures. Patients who undergo cryosurgery alone rarely require hospitalization, and the procedure usually is performed on a "come and go" basis. A urethral catheter is left in place for 3 weeks, as such a period of urethral catheterization appears to be associated with a lower likelihood of postoperative tissue sloughing and urinary retention as compared to use of a suprapubic tube alone or shorter periods of urethral catheterization. The efficacy of various forms of treatment for prostate cancer can be assessed by analyzing several end points. Commonly, patients who have been treated with cryotherapy have undergone repeat prostatic biopsy 6 to 12 months after the procedure. These results must be analyzed cautiously as not all patients treated underwent biopsy, some patients received neoadjuvant androgen deprivation (which could have affected biopsy data), and false-negative biopsy results are not uncommon, certainly in those with limited disease before treatment. Not surprisingly, there is a relationship between clinical stage and the likelihood of a positive posttreatment biopsy after cryotherapy. The likelihood of a positive biopsy is approximately 9% for those with clinical stage T1 or T2 disease and at least 21% for those with T3 disease. The significance of benign epithelium is unknown, and such findings may represent areas of the prostate not frozen to low temperatures, perhaps, in the area of the urethral warmer. It must be recognized that certain areas of the prostate or seminal vesicles are more likely to be sites of treatment failure. Radiation or cryotherapy does not result in complete destruction of all prostate tissue. Both biochemical and biopsy failure tended to occur within the first 12 months after treatment. The patient population was composed of men who generally had intermediate- or high-risk disease (T3 or T4 disease in 61%). Actuarial biochemical recurrence-free survival rates at 1 year and 3 years after treatment for those patients undergoing primary cryosurgery (excluding repeat procedures and patients who failed previous radiation or radical prostatectomy) were 62% and 49%, respectively. Actuarial biochemical recurrence-free survival 1 year and 3 years after cryosurgery was 82% and 69% for low-risk patients and 58% and 45% for intermediate- to high-risk patients, respectively (P =. Neoadjuvant androgen deprivation was not shown to improve outcome significantly after cryosurgery. Prostate biopsy was performed after 167 procedures and proved to be positive in 64 (38%) such cases.
Previous studies have demonstrated no difference in outcome between cholecystojejunostomy and choledochojejunostomy. Our choice for biliary bypass at the time of surgery is a Roux-en-Y choledochojejunostomy. The endoscopic stent (if present) is removed, the distal bile duct is closed, and an end-to-side choledochojejunostomy is created with a single layer of interrupted monofilament sutures. In patients with unresectable disease, laparoscopic cholecystojejunostomy represents another alternative for biliary decompression. Tumors of the uncinate process or the inferior aspect of the pancreatic head that extend to the root of the mesentery often deform the ampulla of Vater, making endoscopic cannulation difficult. Patients with symptomatic jaundice and ascites present a unique technical challenge. A subset of these patients have such advanced disease (and poor performance status) that pain control and hospice care are all that is indicated. For the occasional patient who presents with jaundice and the rapid onset of ascites and requires palliative treatment, we prefer endoscopic stent placement followed by early peritoneovenous shunting if an initial attempt at diuretic therapy is unsuccessful. If endoscopic stenting is not technically possible, laparoscopic cholecystojejunostomy is a reasonable alternative in the absence of high-volume carcinomatosis. Transhepatic biliary drainage with an internal-external catheter is not advised in patients with ascites because the ascitic fluid leaks around the catheter at the skin entrance site. In patients with malignant ascites, the surgeon should avoid using transabdominal catheters and making large abdominal incisions because of the risk of ascitic leak. The subject of prophylactic gastrojejunostomy is not as relevant to the current surgical management of patients with pancreatic cancer as it was before the 1990s. Accurate preoperative imaging has increased resectability rates so that fewer patients are found to have unresectable disease at surgery. Advocates of prophylactic gastrojejunostomy state that the procedure can be performed safely, is not associated with postoperative delayed gastric emptying, and prevents subsequent gastric outlet obstruction in 10% to 20% of patients. Patients found to have unresectable disease and not to have intraoperative evidence of impending gastric outlet obstruction (such patients were excluded from analysis) at the time of laparotomy were randomly assigned to receive either a prophylactic gastrojejunostomy or no further surgery. Subsequent gastric outlet obstruction developed in 8 (19%) of the 43 patients who did not receive a gastric bypass, compared to 0 of 44 patients who received a gastrojejunostomy. Postoperative delayed gastric emptying occurred in 2% of patients in both groups, and the mean survival duration (8. Furthermore, no perioperative deaths occurred, and the mean hospital stay was approximately 8 days; again, no difference was noted between groups. The authors concluded that a retrocolic gastrojejunostomy should be performed routinely when a patient with pancreatic or periampullary cancer is found at operation to have unresectable disease. It appears that high-volume referral centers can perform palliative surgical biliary and gastric bypass procedures with low morbidity and mortality; however, these results may not be easily translated to low-volume centers with less experience. For example, a review of patients at 74 Department of Veterans Affairs hospitals from 1987 to 1991 concluded that prophylactic gastric bypass should be performed in patients with locally advanced, nonmetastatic pancreatic cancer, but the 30-day operative mortality rate (15% to 20%) was unacceptably high for palliative surgery in patients with such a short anticipated survival. At a median follow-up of 6 months (81% of patients had died of disease), only 3 (2%) of 155 patients had undergone a subsequent open surgical procedure. Gastrojejunostomy for symptomatic gastric outlet obstruction was performed in two of these three patients. Two additional patients underwent elective gastric bypass (one was performed laparoscopically) at the time of biliary bypass. One additional patient required a percutaneous gastrostomy tube for poor gastric emptying during the terminal phase of his disease. In their study, only 1 (3%) of 34 patients treated with endoscopic biliary decompression required surgical bypass for gastric outlet obstruction. These two nonrandomized studies do not support the practice of routine prophylactic gastric bypass.
If uptake by primary or metastases is high, it is possible to deliver very high radiation doses by increasing the administered activity. Treatment response in patients with pheochromocytomas can be measured by catecholamine secretion and standard tumor size measurements. A beneficial response to treatment was observed in nine patients (60%), four never responded, and others had a slight response. Five patients had measurable partial responses to treatment, and seven had clear hormonal responses. Toxicity included pancytopenia in one patient that resolved after discontinuation of therapy. Patients with benign pheochromocytomas have elevated plasma levels of norepinephrine or epinephrine, and none have elevated plasma levels of dopa. Sixty percent of patients with malignant pheochromocytomas have elevated plasma levels of dopa, in contrast to benign pheochromocytoma. The similarity between malignant pheochromocytoma and neuroblastoma is further supported by the astonishing responsiveness of malignant pheochromocytomas to therapy that is effective in treating neuroblastomas. The chemotherapy regimen consists of cyclophosphamide, 750 mg/m 2 intravenously, on day 1, vincristine, 1. Doses of cyclophosphamide and dacarbazine have been increased or decreased on the basis of neurotoxicity. This regimen has now been reported in 14 patients with metastatic pheochromocytoma. One patient had a complete response (both biochemical and imageable) that lasted for 9 months. One other patient also had a biochemical complete response, and a total of eight (57%) patients had clear decreases in 24-hour levels of urinary catecholamines. Seven patients (50%) also had at least a 50% decrease in the measurable size of tumor. Biochemical response (urinary catecholamines) correlated well with response evaluated on imaging studies. All responding patients have had dramatic improvement in hypertension control and performance status. The sarcoma, breast cancer, lung cancer, and adrenocortical carcinoma syndrome revisited. Highly consistent genetic alterations in childhood adrenocortical tumors detected by comparative genomic hybridization. Steroid 21-hydroxylase mutations and 21-hydroxylase messenger ribonucleic acid expression in human adrenocortical tumors. Adrenocortical carcinoma: an immunohistochemical comparison with renal cell carcinoma. Adrenocortical carcinoma: nuclear deoxyribonucleic acid ploidy studied by flow cytometry. Distinguishing cortical adrenal gland adenomas from carcinomas by their quantitative nuclear features. The pathology of adrenocortical neoplasia: a correlated structural and functional approach to the diagnosis of malignant disease. The metyrapone and dexamethasone suppression tests for the differential diagnosis of the adrenocorticotropin-dependent Cushing syndrome: a comparison. Diagnosis of adrenal tumors with radionuclide imaging Spec Top Endocrinol Metab 1984;6:1. Adrenal localization in the adrenocorticotropic hormoneindependent Cushing syndrome. Adrenal scintigraphy of well-differentiated (functioning) adrenocortical carcinomas: potential surgical pitfalls. Preeyasombat C, Sirikulchayanonta V, Mahachokelertwattana P, Sriphraprodang A, Boonpucknairig S. Renin gene expression in the adrenal and kidney of patients with primary aldosteronism.