"Generic colchicine 0.5mg with mastercard, virus model".
Q. Taklar, M.S., Ph.D.
Medical Instructor, California Health Sciences University
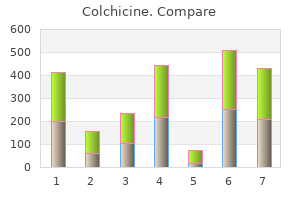
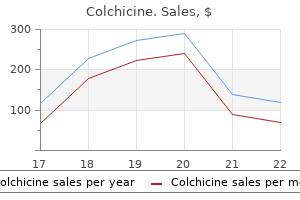
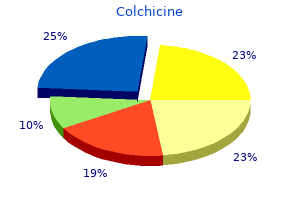
Other potential side effects include agranulocytosis, methemoglobinemia, hypersensitivity syndrome, malaise, StevensJohnson syndrome, photosensitivity, neurological side effects, nephropathy, hypothyroidism, nausea, vomiting, fever, rash, and lymphadenopathy. Sulfasalazine, sulphamethoxypyridazine and sulfapyridine act as alternative medications. In patients with sulfa allergies, oral or potent topical corticosteroids may be used in combination with anti-histamines. Although oral corticosteroids show disappointing results, topical corticosteroids may be more beneficial in terms of controlling pruritis. The third-generation anti-histamines have greater activity on eosinophils and may be helpful to alleviate itching. This combination treatment has proved effective in a case study even once heparin therapy was discontinued. Intensive heparin therapy has lead to rapid improvement in skin lesions over 2-13 days. Tetracyclines have also been found to act at the basement membrane, suppressing complementmediated inflammatory reactions and leukocyte chemotaxis. Nicotinamide, a free-radical scavenger, inhibits neutrophil and eosinophil chemotaxis and secretion, and also acts to decrease protease release from leukocytes. Heparin therapy may be difficult to maintain; however, the literature demonstrates that once heparin is discontinued, a combination of tetracycline plus nicotinamide continues to be effective. A long-term gluten-free diet as an alternative treatment in severe forms of dermatitis herpetiformis. Dermatitis herpetiformis and glutensensitive enteropathy in a patient with nodular prurigo. Clinical, pathologic, and immunopathologic features of dermatitis herpetiformis: review of the mayo clinic experience. Celiac disease and dermatitis herpetiformis: the spectrum of gluten-sensitive enteropathy. Immunoglobulin, complement and epidermal transglutaminase deposition in the cutaneous vessels in dermatitis herpetiformis. Autoantibodies against epidermal transglutaminase are a sensitive diagnostic marker in patients with dermatitis herpetiformis on a normal or gluten-free diet. Transglutaminases as diagnostically relevant autoantigens in patients with gluten sensitivity. Clinical, histological and immunopathological findings in 32 patients with dermatitis herpetiformis during. No increase in risk of fracture, malignancy or mortality in dermatitis herpetiformis: a cohort study. Dermatitis herpetiformis effectively treated with heparin, tetracycline and nicotinamide. Because of an increased risk for comorbid conditions, accurate diagnosis and treatment are imperative. As seen in our patient, patients unresponsive or intolerant to dapsone have several therapeutic options. Figure 1 Figure 2 Figure 3 42 dermatitis herpetiFormis: a case report and discussion inuous im Cont pr *myfinaceaskinsavvy. Although some reduction of erythema which was present in patients with papules and pustules of rosacea occurred in clinical studies, efficacy for treatment of erythema in rosacea in the absence of papules and pustules has not been evaluated. Finacea is for dermatologic use only, and not for ophthalmic, oral, or intravaginal use. Finacea is contraindicated in individuals with a history of hypersensitivity to propylene glycol or any other component of the formulation. In clinical trials, sensations of burning/stinging/tingling occurred in 29% of patients, and itching in 11%, regardless of the relationship to therapy. Post-marketing safety-Skin: facial burning and irritation; Eyes: iridocyclitis on accidental exposure to the eye.
The walls of the cyst are typically devoid of cutaneous adnexa and contain a stratified keratinizing squamous epithelium that is filled with desquamated keratinous debris. These cysts affect patients of all ages, and they usually present in early adulthood or middle age. These cysts may be encountered anywhere on the neck, but are more commonly seen on the trunk. Additionally, they can possess greasy material admixed with hairs as well as mural adipose tissue. Although most commonly found in lines of embryonic closure in the faces of children, they can occur in the neck and therefore constitute an important differential diagnosis to consider. This case, however, underscores the importance of considering this entity in the differential diagnosis of any midline neck anomaly at any age. Bronchogenic cyst presenting as a symptomatic neck mass in an adult: case report and review of the literature. Figure 2: High-power photomicrograph depicting pseudostratified ciliated respiratory epithelium with mucous vacuoles. We report a case of an 18-year-old female who presented to our clinic with multiple red papules and plaques with scale on her abdomen, back, and bilateral lower extremities. Introduction Perforating diseases are a group of disorders in which there is a transepidermal elimination of collagen, elastic tissue or necrotic connective tissue. The Koebner phenomenon may occur, in which injury to the skin results in the formation of new lesions. The pathology reveals transepidermal elimination of necrotic material, collagen or, rarely, elastic tissue. The disease is characterized by the development of discrete, erythematous follicular papules with a central white keratotic core. Lesions most often affect the extremities, with a predilection for the hairy portions of the arms, forearms and thighs. The exact etiology is unknown, although it is speculated to be the end result of abnormal follicular keratinization that most likely is caused by irritation, either chemical or physical, and even chronic rubbing. Case report An 18-year-old female was referred to our clinic by a pediatrician complaining of an itchy rash on her b i l a the r a l u p p e r ex t re m i t i e s, l owe r extremities, back and abdomen for about a week. Prior to the start of the rash, she did not use any new medications or any new produc ts. She also had no prior surgical history or known drug allergies, and she was taking multivitamins. On physical examination, the patient had multiple red papules and plaques with slight scale on her abdomen, back, and bilateral lower extremities. At the initial visit, a 3 mm punch biopsy was performed on one of the lesions on the back. Histopathology revealed a ruptured follicular unit surrounded by mixed cell infiltrate including neutrophils and histiocytes. Also, there was a narrow channel through which elastic tissue fibers had penetrated. Patient was prescr ibed Locoid Lipocream (hydrocortisone butyrate) to be applied twice daily to the affected area. The lesions on the back and abdomen were resolved after two weeks of treatment with Locoid Lipocream. A two-month follow-up revealed the remaining lesions on the lower extremities had resolved on their own. T h e m o l e c u l a r m e ch a n i s m o f transepidermal elimination of the elastic material is poorly understood. It has been postulated that the interaction between elastic material and keratinocytes plays an important part in this extrusion mechanism. It has been hypothesized that altered elastic fibers bind via the elastin receptor to the keratinocytes. This induces a rapid terminal differentiation with the formation of an epidermal channel.
There is neck stiffness, and worsening of her headache on straight leg raising but no focal neurology. Ophthalmoscopy is not tolerated and the patient asks you to turn the lights off as they are hurting her eyes. There is widespread abnormal high attenuation with a gyriform distribution within both cerebral hemispheres. This high attenuation material is denser than adjacent brain parenchyma but less dense than bone and represents acute blood. There is mass effect with sulcal effacement and the lateral/third ventricles are prominent in keeping with hydrocephalus. Some acute blood is seen within the third ventricle at the expected origin of the aqueduct of Sylvius. Subarachnoid haemorrhage is defined as blood collected between the pia and arachnoid mater. Commonly causing pain, haematuria and proteinuria, unrestricted cyst growth replaces normal renal parenchyma, eventually causing renal failure. He has had a low-grade fever that has not resolved despite bed rest and anti-pyrexial medication. He denies having a cough or any urinary symptoms and is usually a fit and active person. Over the last 2 days he has noticed a red rash on his legs that is becoming increasingly hot and tender, and also complains of facial swelling with an achy discomfort in his jaw. He has also had to stop wearing his contact lenses as his eyes have become red and irritable. Examination On examination he looks tired with red conjunctiva and a temperature of 38. There is smooth swelling of the parotids bilaterally with tenderness on palpation. His cardiovascular, respiratory and abdominal examination is normal but there is an ill-defined rash on the anterior aspect of both his shins that is raised, nodular and tender. A full septic screen is performed and while the blood results are awaited, a chest radiograph is performed (Figure 95. There is bilateral hilar enlargement with widening of the paratracheal stripe and loss of the normal convexity to the aortopulmonary window. The lung parenchyma also demonstrates pathology, with reticular nodular shadowing bilaterally in a mid and upper zone distribution with basal sparing. The nodules are small (<2 mm) and there is no evidence of cavitation, pneumothorax or pleural effusion. In the absence of an infective cause, biochemical and radiological findings are helpful, although definitive diagnosis relies on obtaining tissue by procedures such as transbronchial biopsy at bronchoscopy. Although bilateral hilar adenopathy is the hallmark of this disease, the lung parenchyma is involved in approximately two-thirds of cases. High-resolution (thin, 1mm) slices confirm reticular shadowing related to thickening of the interlobular septae from the interstitial lung disease. However, the presence and distribution of additional nodules is key to the diagnosis. More acutely, the patient can suffer from erythema nodosum where the skin is red and hot with tender nodularity. This is most commonly seen in the stomach, followed by the colon, oesophagus and small bowel. Late in the disease, granuloma formation can cause hepatic nodularity, however the patients often remain asymptomatic. The overlying cortex demonstrates periosteal reaction and subperiosteal resorption mimicking hyperparathyroid disease. Since its insertion, the patient has noticed that the skin at the insertion site is continuing to slowly swell. She denies any shortness of breath or pain, and there is no evidence of active haemorrhage. Examination Examination reveals an ill-defined fullness to the right lateral chest wall, which has increased in size over the last few days. The clinicians are concerned about basal crepitations over the area on auscultation with no evidence of a vascular bruit.
Success with surgical correction is much improved if undertaken before 60 days of life. If an abdominal ultrasound or liver-needle biopsy is consistent with biliary atresia, exploratory laparotomy is performed expeditiously. The initial goal at surgery is to confirm the diagnosis with demonstration of fibrotic biliary remnants and absent proximal and distal bile duct patency. These patients require cardiopulmonary stabilization prior to any operative repair. Severe hypoxia and respiratory distress at birth are a result of primary pulmonary hypertension due to hypoplasia rather than from compression of the lung from abdominal contents. Low tidal volumes and permissive hypercapnia are strategies of mechanical ventilation to prevent barotrauma. Medical therapies for pulmonary hypertension such as inhaled nitric oxide have been used. Closure of the diaphragmatic defect, which occurs posterolaterally (Bochdalek hernia), can be performed from the abdomen or the chest. Coarctation is diagnosed by echocardiography; cardiac catheterization is rarely needed. Preoperative management includes administration of prostaglandins to reopen the ductus arteriosus which improves flow distal to the coarctation and to the lower body. Without surgery, complications in adults arise with eventual death from cardiac failure, rupture of aortic aneurysms or of a cerebral artery, and bacterial endocarditis. Patients who are operated on earlier in life have a better chance of becoming normotensive. Transposition of the great vessels is a right-to-left shunt that leads to cyanosis. Except where there is persistent congenital pulmonary hypertension, patent ductus arteriosus and atrial septal defects cause a shunting of oxygenated blood from the aorta and left atrium, respectively, back into the pulmonary artery and right atrium. These anomalies cause recirculation of oxygenated blood within the cardiopulmonary circuit but not cyanosis. Other, less common congenital lesions in which the pulmonary arterial blood flow is relatively decreased include tricuspid atresia, Ebstein anomaly, and hypoplastic right ventricle. It may lead to cardiac failure and pulmonary hypertension if the defect is larger than 1 cm, or it may be asymptomatic if the defect is small. Surgery is not indicated for the asymptomatic patient with a small defect since a substantial number of these anomalies close spontaneously during the first few years of life. Operation is indicated in infants with congestive heart failure or rising pulmonary vascular resistance (owing to the left-to-right shunt). Congenital cyanosis that persists beyond the age of 2 years is associated, in the vast majority of cases, with tetralogy of Fallot. Patent ductus arteriosus is associated with the characteristic continuous machinery murmur. Index Please note that index links point to page beginnings from the print edition. Locations are approximate in e-readers, and you may need to page down one or more times after clicking a link to get to the indexed material. A Abdomen, free fluid in, 113, 136 Abdominal decompression, 215, 242 Abdominal injuries diagnosis and treatment, 93-95, 115-116, 118 duodenal hematoma, 97, 120 gunshot wounds, 100-101, 124-125 repair of, 108-109, 132 Abdominal-perineal resection, 226, 251 Achalasia, 198, 228, 262, 275 Acidosis metabolic, 4, 16, 21-22, 35 non-anion-gap, 13, 16, 32, 34 oxygen dissociation curve, 56-57 respiratory, 21, 39, 57 Active surveillance, 303 Addison disease, 50, 68, 170, 183 Adenomas, pleomorphic, 334, 339-340 Adrenal insufficiency, 8, 27, 170, 183 Adrenocortical insufficiency, 50, 68 Adrenocortical tumors, 175, 189 Adriamycin (doxorubicin), 149, 165 Air embolism, 45, 62 Airway management, 51, 69 Airway obstructions, 114, 137 Albendazole, 242 Albumin, serum levels of, 47, 64 Alcohol use, 158 Alkalosis metabolic, 3, 19, 21 respiratory, 4, 21-22 Alveolar ventilation, 46, 64 Amino acids, 126-127 Anaerobic infections, 82, 90 Analgesia, epidural, 42, 59 Anaphylactoid reactions, 45, 62-63 Anesthetics. See also specific types local, 44, 61 types of, 53, 71-72 Angina, 272 Angiography, 5, 24, 245, 288, 293, 295 Ankle-brachial indices, 100, 123-124 Anterior cruciate ligament injury, 305, 311 Antibiotic therapy perioperative, 82, 90 prophylactic treatment, 2, 20, 82, 85, 90 Antiplatelet agents, 283, 293 Antrectomy, 201, 230 Anus carcinomas, 213, 226, 241, 251 imperforate, 343-344, 351-352 Aortic aneurysm, abdominal cardiac function assessment, 54 colitis, ischemic, 279-280, 290-291 diagnosis and repair, 281, 291 fluid management, 41, 58, 279, 289-290 Aortic aneurysm, thoracic, 259, 262, 271, 276 Aortic coarctation, 263, 276, 350, 358 Aortic dissection, 255, 267-268 Aortic injury, thoracic, 110, 133 Aortic regurgitation, 263, 276 Aortic stenosis, 253, 265 Aortobifemoral bypass, 296 Appendectomy, 209, 238, 248 Appendiceal adenocarcinomas, 198, 228 Appendiceal carcinoid tumors, 181, 195, 219, 223, 245, 248 Appendicitis, 215, 242-243 Aprotinin, 70 Argyll Robertson pupil, 262, 275-276 Arterial embolus, 284, 294 Arterial injuries, 95, 97, 104, 117, 120, 123-124, 127-128 Arterial insufficiency, 117, 283, 292 Aspergilloma, 275 Aspiration cytology, 143, 159 Aspiration of gastric contents, 49, 66, 69 Aspirin intoxication, 4, 22 Aspirin prophylaxis, 283, 293 Atrial septal defect, 358 Axillofemoral bypass, 288, 296 Azathioprine, 152, 167-168 B Bacteroides fragilis, 82, 90 Balloon tamponade, 231-232, 250 Basal cell carcinoma, 77, 80, 83, 86, 91 Basal metabolic rate, 17, 36 Beck triad, 43, 61 Benign prostatic hyperplasia, 299, 303 Bevacizumab, 165 Bile ducts repair of, 96, 119, 210, 239 vanishing bile duct syndrome, 153 Biliary atresia, 348, 357 Biopsies, 145, 147, 161-163 Bladder cancer, 297, 301 Bleeding time, 10, 29, 54, 73 Bleomycin, 166 Blood gases alveolar ventilation, 46, 64 oxygen dissociation curve, 39, 56-57 Blood transfusions hypocalcemia, 30 reactions to , 4, 6, 9, 16, 22-23, 26, 29, 35, 38, 46, 55-56, 58, 63 timing of, 8, 28 Boerhaave syndrome, 257, 269 Bone marrow transplantation, 142, 157 Bowel. Patient will be switching from one antiretroviral combination to an alternate product with the same active ingredient. References Requests for continuing therapy that were approved by a previous Health Plan will be honored for at least 30 days upon receipt of documentation demonstrating that approval. Available at: Requests for continuing therapy that were approved by a previous Health Plan will be honored for at least 30 days upon receipt of documentation demonstrating that approval.
The area of the nail was noted to grow in an abnormal fashion and also appeared to have a lesion underneath. A nail matrix biopsy of her right fourth finger with nail avulsion was scheduled and performed a week after initial consult. Tumorinfiltrating lymphocytes and mitotic index of 1/mm2 were observed (Figures 1-5). After diagnosis of nail matrix melanoma was established, she was referred to an oncology surgeon, where a sentinel node biopsy revealed one of two lymph nodes positive for metastatic malignant melanoma. She underwent amputation of her right fourth finger at the distal interphalangeal joint and lymphadectomy of the right axillary sentinel lymph node. At the time of submission, she is to undergo interferon treatment for her metastatic melanoma. Results of 5-year survival rates based on Breslow depth in 49 patients with subungual melanoma at the Memorial SloanKettering Cancer Center database from 1992 to 2004 are shown in Table 3. Conclusion Nail matrix melanoma is often a challenge to diagnose early due its rarity and resemblance to other disorders of the nail. Delay in diagnosis often results in disease progression, with poorer prognosis and treatment options. Early excision and pathologic examination of all lesions with suspicious clinical features is presently the only modality to avoid misdiagnosis. Management Treatment of nail matrix melanoma is primarily surgical, with wide local excision and digit amputation as primary modalities of therapy. This formulation of minocycline has not been evaluated in the treatment of infections. Pseudomembranous Colitis Pseudomembranous colitis has been reported with nearly all antibacterial agents and may range from mild to life-threatening. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of antibacterial agents. Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of clostridia. Studies indicate that a toxin produced by Clostridium difficile is a primary cause of "antibiotic-associated colitis". If visual disturbance occurs during treatment, patients should be checked for papilledema. Concomitant use of isotretinoin and minocycline should be avoided because isotretinoin, a systemic retinoid, is also known to cause pseudotumor cerebri. After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to discontinuation of To reduce the development of drugthe drug alone. This adverse reaction is more common during long-term use of the drug but has been observed following repeated short-term courses. A decrease in fibula growth rate has been observed in premature human infants given oral tetracycline in doses of 25 mg/kg every 6 hours. Results of animal studies indicate that tetracyclines cross the placenta, are found in fetal tissues, and can cause retardation of skeletal development on the developing fetus. Evidence of embryotoxicity has been noted in Hepatotoxicity Post-marketing cases of serious liver injury, including irreversible drug-induced hepatitis and fulminant hepatic failure (sometimes fatal) have been reported with minocycline use in the treatment of acne. While this is not a problem in those with normal renal function, in patients with significantly impaired function, higher serum levels of tetracycline-class drugs may lead to azotemia, hyperphosphatemia, and acidosis. If renal impairment exists, even usual oral or parenteral doses may lead to excessive systemic accumulations of the drug and possible liver toxicity. Under such conditions, lower than usual total doses are indicated, and if therapy is prolonged, serum level determinations of the drug may be advisable. Central Nervous System Effects Central nervous system side effects including light-headedness, dizziness or vertigo have been reported with minocycline therapy. Patients who experience these symptoms should be cautioned about driving vehicles or using hazardous machinery while on minocycline therapy. These symptoms may disappear during therapy and usually rapidly disappear when the drug is discontinued. Benign Intracranial Hypertension Pseudotumor cerebri (benign intracranial hypertension) in adults and adolescents has been associated with the use of tetracyclines.