"Discount generic forzest uk, erectile dysfunction pump implant".
B. Umul, M.B.A., M.D.
Deputy Director, Albany Medical College
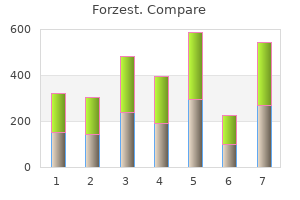
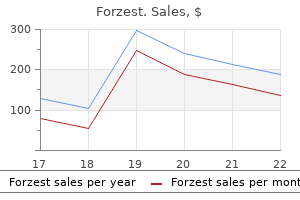
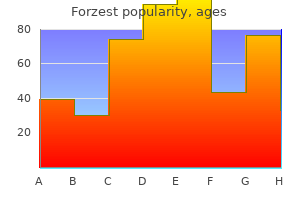
Natural history of disease must be understood Effective treatment is available A test is available by which the disease can be recognized in its pre-clinical phase the application of screening makes better use of limited resources than competing medical activities Evaluation of screening programs Early outcomes for evaluating a screening program are stage of the disease and case fatality. If the screening is effective, the stage distribution for cases should be shifted towards earlier stages and a greater proportion of patients should survive for any given time period. However, these outcome measures can all be affected by features of disease definition and natural history. Lead time is the amount of time by which screening advances the detection of the disease. Even if the interval between the (unknown) biologic onset of the disease and death is unchanged, earlier detection will lengthen the interval between diagnosis and death so that survival appears lengthened. Lead time bias results when a screening program creates the appearance of delaying morbidity and mortality but in reality does not alter the natural history. Length bias results if tumors are heterogeneous in respect to their aggressiveness, with slower growing tumors having a more favorable prognosis (or at least longer time to death). Slower growing tumors are more likely to be detected by screening, since they are present and asymptomatic longer. So tumors detected by screening will overrepresent slow growing, hence survivable, tumors than will cancers detected because of appearance of symptoms (the latter cases are called "interval cases" because they are detected during the interval between screens). Overdiagnosis results from the detection, by the screening test, of nonmalignant lesions that are judged to be malignant or to have malignancy potential. Prior to the use of the screening test, such lesions would not be detected, so their true prognosis may be unknown. Overdiagnosis is a particular concern in evaluating the efficacy of prostate cancer screening. But because they must usually be very large and of long duration, such trials are often difficult and very costly. The National Cancer Institute is currently conducting a very large (74,000 men and 74,000 women) and lengthy randomized trial to evaluate the effectiveness of screening for prostate, lung, colorectal, and ovarian cancers. Both natural history and screening considerations come into play in such questions as the interpretation of secular changes in incidence and mortality. There has also been a "dramatic" upsurge in in situ breast cancer diagnosed since 1983. Breast cancer mortality overall was stable in the 1970s and began to fluctuate in the mid-1980s. In support of that interpretation is the fact that among white women age 50 and older, localized disease has increased. There has also been a rapid increase in sales and installation of new mammography units during the 1980s, and the number of mammograms has risen dramatically. The observation of a striking increase in estrogen-receptor positive cancers suggests some biological change has occurred. Another cancer where issues of natural history and early detection are of great importance is cancer of the prostate. Although "indolent" prostate cancers have the pathological features of cancer, if their growth is so slow that they will never become clinically manifest, should they be considered as the same disease as cancers of clinical importance In addition, the lengthy natural history of most prostate cancers raises the concerns of lead time bias, length bias, and overdiagnosis for any observational approach to evaluating the efficacy of screening for early prostate cancer. In addition, there are major questions about the effectiveness of both existing modes of treatment and existing modes of early detection. In: Rothman and Greenland, Modern Epidemiology 2ed, Philadelphia, Lippincott-Raven, 1998, ch 27. Accuracy of cancer death certificates and its effect on cancer mortality statistics. Manual of the international statistical classification of diseases, injuries, and causes of death. Measuring Disease and Exposure Descriptive statistics; measuring occurrence and extent of disease; prevalence, incidence (as a proportion and as a rate), and survivorship; weighted averages, exponents, and logarithms. Boston, Little Brown, 1986, pg 23) At the beginning of this text we noted four key aspects of epidemiology: its multidisciplinary nature, and its concern with populations, measurement, and comparison.
Urologists, once again, offer medical, and if necessary, surgical interventions to ease the passage of urine. Urology requires some working knowledge of general surgery and its subspecialties, gynecology, internal medicine (particularly nephrology and endocrinology), pediatrics, neurology, and radiology. Some urologists even completed full general surgery training and then decided to Prefers working with his or her specialize in urology. For starters, surgical interns learn very specialized area of medithe basic techniques-how to hold the cine. For example, these and hand-eye young doctors begin to recognize a postcoordination. Fluid management in the postoperative period can be absolutely critical and requires an understanding of the concepts of third-spacing as well as cardiovascular restrictions. Wound care, including managing drains of all kinds, is another important concept for all surgeons-general or specialist-to master. Gynecology and obstetrics has much overlap with urology, considering the anatomic location. A urologist focusing on female urology shares some of the same patients as a gynecologist subspecializing in urogynecology. Even the general urologist, however, must have a complete understanding of male and female pelvic anatomy. And while a urologist would never perform a hysterectomy or a cesarean section, they could certainly become involved if the gynecologist or obstetrician inadvertently opened the bladder or transected a ureter. Internal medicine-particularly nephrology and endocrinology-is important to the urologist given the overlays with adrenal, renal, and testicular disorders. If a patient presents to the hospital in renal failure, the urologist is often consulted to participate in the workup. In the elderly, the renal failure may be due to a combination of prerenal, intrarenal, and postrenal obstruction. As far as endocrinology is concerned, urologists should have a working sense of male hormones, essential to any infertility workup, as well as the workings of the adrenal glands, given that someone with an adrenal mass may initially present to them for diagnosis. Of course, it is specific to urologic care, but taking care of children is different than taking care of adults and these differences must be learned. Fluid management is different, medicine dosing is different, comorbidities are different, and in general, kids have much higher physiologic reserve and therefore can look well up until the moment they crash. Neurology is a field that plays into the urology database, in that people with spinal cord injuries, congenital or acquired, inevitably have bladder dysfunction. Having a working knowledge of the nervous system, particularly as it relates to the pelvic organs, becomes paramount in treating a neurogenic bladder. Finally, it is essential for urologists to have an understanding of the radiologic imaging that a urologic patient may undergo. As with any surgical specialty, diagnosis is often predicated completely on what the scan looks like. For example, if a man with testicular pain and no palpable mass is sent for a scrotal ultrasound, and a small testicular mass is noted, he will immediately get a workup for testicular cancer. Based on the ultrasound findings alone, he may require counseling for surgical excision. Based on these findings alone, she is diagnosed with probable renal cell carcinoma and offered surgical excision. Renal function for patients with an atrophic looking kidney can be assessed using nuclear medicine. For example, a dimercaptosuccinic acid scan, a radioisotope that binds to renal parenchyma, gives a sense of how well the kidneys are filtering blood, the left compared to the right. Medical students considering a career in urology must accept that this specialty is definitely still a surgical field. In some European countries, urology has been divided into two tracts: operative urology and office urology. In the United States, some think that urology is headed toward that same division. In the meanwhile, however, urologists still manage both sides of the operating room. In reality, a community practice urologist may opt to refer all big open cases to an academic center.
In patients who are clinically unstable and the index of suspicion is high, empiric therapy should be started before laboratory confirmation. Treatment is focused on decreasing the amount of circulating thyroid hormone, antagonizing its effects on the body, supporting hemodynamic stability (anti-pyretics, volume administration, beta-blockers) and treating the precipitating event. The first medication to be administered should be an anti-thyroid medication, such as propylthiouracil or methimazole, to decrease hormone production and conversion of T4 to T3. Saturated solution of iodine should only be given after an anti-thyroid medication as iodine can cause a release of pre-formed thyroid hormone and worsen the disease. Non-specific beta-blockers also decrease peripheral conversion of T4 to T3 and help mediate the cardiovascular manifestations of hyperthyroidism. While previously thought to represent an euthyroid state, current evidence suggests the presence of hypothyroidism at the cellular level. The mechanism of decreased T3 is unclear, but may be mediated by inflammatory markers, lack of nutrients (adaptive fasting response to reduce energy expenditure during illness) or from medications such as dopamine, glucocorticoids, amiodarone and propranolol. Patients with a significantly decreased rT3 should be suspected of having clinical hypothyroidism and may warrant treatment with levothyroxine. If suspected, treatment with parenteral thyroid replacement (T3, T4 or combination) should not be delayed for confirmatory testing. Concurrent adrenal insufficiency may be present; a cortisol level should be obtained with initial labs and treatment started with hydrocortisone until adrenal insufficiency is ruled out. Additional supportive care includes cardiac monitoring, electrolyte replacement (hyponatremia), glucose management, empiric antibiotics, passive rewarming, volume expansion, vasopressors, mechanical ventilation and identification of precipitating causes. Adrenal Insufficiency: Cortisol is a glucocorticoid that mediates many important functions in the critically ill: immunity (cellular and cytokines), sensitivity to inotropes (norepinephrine, epinephrine, and angiotensin) and increasing blood glucose levels (gluconeogenesis). In non-critically ill patients, there is a steady secretion of cortisol with a diurnal variation that peaks in the morning and evening. Clinical signs of adrenal insufficiency include: shock that is refractory to intravenous fluids and vasoconstrictors, low diastolic blood pressure, mental status changes, hypoglycemia, hyponatremia, and hyperkalemia. Despite vasoplegic shock, the overall cardiac output in these 396 patients may be elevated, normal or reduced. In addition to clinical presentation, two tests, a random cortisol level and the corticotropin stimulation test can help establish the diagnosis. Cortisol levels below this threshold are highly suggestive of adrenal insufficiency when clinical signs are present. Levels between 15-25 mcg/dL for patients without septic shock and 15-34 mcg/dL for patients in septic shock may indicate adrenal insufficiency and should be further evaluated by a corticotropin stimulation test. Patients not in septic shock with levels greater than >25 mcg/dL and patients in septic shock with levels >34 mcg/dL usually do not have adrenal insufficiency and are unlikely to benefit from supplemental steroids. Both begin by drawing a baseline serum cortisol level and then giving a dose of corticotropin. Cortisol levels are measured at 30 and 60 minutes after giving the corticotropin and the increase in serum cortisol should be >9 mcg/dL or a final level >18 mcg/dL. Lack of cortisol response suggests the patient may benefit from supplemental steroids. Because of the nuances of performing a test that will yield accurate results and uncertainty when interpreting results, most physicians will choose to treat empirically with steroids and evaluate for clinical improvement rather than using a corticotropin stimulation test to evaluate for adrenal insufficiency. Cortisol levels in patients with septic shock are normally lower than patients with similar degrees of shock precipitated by other causes. The mechanism for this is unclear but may be mediated by cytokines that are released secondary to the infection. This led to studies in septic shock that suggested a decreased mortality and faster reversal of shock when treating patients with hydrocortisone and fludrocortisone. The Surviving Sepsis Campaign limits its recommendation for steroid use to those patients that have shock refractory to intravascular volume repletion and vasopressors. The role of steroids in the development of infections and critical illness myopathy is not entirely clear. Etomidate suppresses the function of 11-hydroxylase, which is involved in cortisol production. Long-term infusions of etomidate have been associated with increased mortality, but while single induction doses appear to decrease cortisol levels, the clinical consequences are still uncertain.
Vascular Surgery Vascular surgery involves the arteries and veins of the entire body, from the neck to the distal extremities. To help an older man with severe peripheral vascular disease in his leg, which could lead to gangrene, vascular surgeons perform a bypass operation to go around the diseased artery segment. Vascular surgeons, therefore, maintain a high level of technical skill and finesse. It is a subspecialty full of great variety: elective procedures such as arteriovenous fistulas for dialysis access to emergencies like repairing a ruptured aortic aneurysm. Most patients undergoing vascular surgery have multiple comorbidities, in particular heart disease and diabetes. This highlights the need to know a great deal about the medical management of these disorders. If you enjoy medicine, surgery, and critical care, completing a 1-to 2-year fellowship in vascular surgery is the ideal combination for a gratifying career. Advances in endovascular surgery (stent-grafts for treatment of abdominal aortic aneurysm) are revolutionizing the field and expanding the scope of vascular surgery. Surgery is the perfect field for those who want to see that their actions have an immediate and essential effect on their patient. It is an ideal career for those who want to heal, quite literally, with their hands. Consider the treatment of a teenager with appendicitis: a discussion with the patient, a dose of antibiotics, anesthesia, incision, resection of the appendix, and discharge the following day. Before the era of antibiotics and rapid surgical treatment, appendiceal perforation was much more common, often leading to death from overwhelming abdominal infection. A survey of 59 surgeons currently in practice said that it brought them joy to "fix patients. If they see what surgeons do and how they love it, they will be bitten by the bug that has bitten so many-generation after generation. Nothing is greater than the unbelievable surge of adrenaline that occurs while scrubbing in, stepping into the operating room, and gowning up. Surgeons combine the scientific nature of a technician with the passion of an artist and the empathy of a physician. They demand nothing but the best for the patients, and they give nothing but the best in all of their efforts. Although challenging and demanding, surgery amply rewards all the effort you put into it. Danagra Georgia Ikossi is a resident in general surgery at Stanford University Medical Center. After growing up both here and in Cyprus, she earned her undergraduate degree from Bates College. Jonathan Long Le, is a resident in plastic surgery at the University of California-San Francisco. Many medical students, patients, public policy makers, and even physicians in other fields of medicine might find it difficult to define. In fact, nearly half of all patients confuse these physicians with family practice doctors, general practitioners, or even interns (first-year residents). In a single day, they can act as a diagnostician, an educator, a director, an advocate, a motivator, a healer, and a comforter. Some internists spend their time providing acute and chronic primary care; others become subspecialists in cardiology, gastroenterology, endocrinology, and more. Whether focusing on one organ system or taking care of the whole patient, internists approach everything with great intellectual curiosity. Sick patients with complex medical problems turn to internists for high quality care. In many ways, internists are similar in practice style to pediatricians-but the kids have grown up.
There is no indication for neuromuscular relaxation in myasthenia gravis patients. Transcranial dopplers show elevated velocity with a high lindegaard ratio consistent with vasospasm. Within the fixed volume of the skull, there is little ability to compensate for increases in the volume of any of the three components. When there is an increase in the volume of one component, the volume of the other components decrease, to a point. Patient Case: A 41-year-old woman is involved in a high speed motor vehicle accident and hits a tree. On exam, she has numerous superficial abrasions, an actively bleeding left eyebrow laceration, clear breath sounds bilaterally, and normal heart sounds. Cerebrospinal fluid Cerebrospinal fluid is produced by the choroid plexus at a rate of 20ml/kg/day (approximately 500ml/day in adults). Obstructive hydrocephalus is when the ventricular system within the brain is disrupted and the ventricles are no longer patently connected. This can be caused by damage to the arachnoid villi or by blood in the subarachnoid space. Also falling into the category of increased parenchyma are space occupying lesions which can refer to tumors (benign or malignant), as well as abscesses. Increased brain parenchyma presents as cerebral edema and there are two types: vasogenic and cytotoxic. This occurs when osmotic and hydrostatic pressure favor plasma water leaving the intravascular space into the extravascular space. This can occur with rapid electrolyte or osmolar shifts, hypertensive emergency, and venous outflow obstruction. Cytotoxic cerebral edema is caused by direct neural injury and cell death resulting in cellular edema. There are many different ways, but the most common method and gold standard is via an intraventricular catheter (ventriculostomy catheter) connected to an external pressure transducer. These procedures are typically performed by neurosurgeons or neurocritical care providers. However, they are not useful if placed incorrectly and cannot be recalibrated once inserted. Studies show that patients with less intracranial hypertension have better outcomes. High dose corticosteroids are indicated in cases of vasogenic edema caused by a tumor, abscess or neuroinflammatory process. Tier 1 treatment strategies include securing the airway, short term hyperventilation (effective for up to 6 hours), bolusing mannitol 0. If starting hypertonic saline infusion, check labs every 2-4 hours for a goal serum sodium of 140-150 mEq/L. Remember that concentrations of NaCl >2% require central venous access to administer. However, not all patients are surgical candidates and surgery comes with its own inherent risks. These interventions have a significantly higher risk of morbidity and mortality associated with them. Kristiansson H, Nissberg E, Bartek Jr J, Andresen M, Reinstrup P, Romner B: Measuring elevated intracranial pressure through noninvasive methods: A review of the literature. Which of the following is not a Tier 0 intervention for elevated intracranial pressure A meta-analysis of randomized controlled trials of mannitol versus hypertonic sodium solutions to manage raised intracranial pressure in traumatic brain injury. Three subtypes of delirium describe two constellations of specific symptoms in each domain. Although he responds to commands during these incidents, several attempts are needed to gain his attention. He continues to have periods of confusion and paranoia, claiming the staff is trying to harm him. Hypoactive delirium presents with symptoms associated with diminished cognition, including lethargy, behavioral withdrawal, and impaired motor skills. Patients who display cardinal features of both hyperactive and hypoactive delirium are diagnosed with the mixed subtype of the syndrome.