"Generic bimatoprost 3ml on line, symptoms ketoacidosis".
E. Hatlod, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Assistant Professor, University of Texas at Tyler
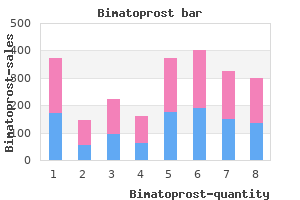
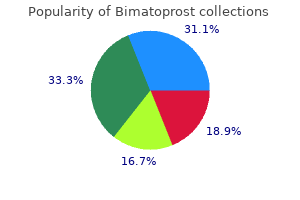
However, the rate of emergent surgery for complications of peptic ulcer (bleeding and perforation) has not changed. Perhaps as a result, the average age of patients with perforation has increased from 40 to 50 years two decades ago to 60 to 70 years now. Indications for emergent or urgent operative intervention are more common and include perforation, bleeding, and gastric outlet obstruction. A patient clearly needs surgery if there is acute peritonitis due to a perforated peptic ulcer. In the patient with equivocal signs of peritonitis, some have advocated examination of the upper gastrointestinal tract with water-soluble contrast medium followed by conservative management if the studies show that the perforation is sealed. When patients present more than 48 hours after a perforation, non-operative management is indicated provided that the perforation is sealed and the patient is not septic. In older patients or patients with more life-threatening bleeding, a surgical consultation should be obtained promptly. Truncal vagotomy and pyloroplasty should be reserved for elderly or high-risk patients in whom expediency is desirable. This minimally invasive surgery has the advantages of reduced postoperative pain, a shortened hospital stay (1 to 3 days), earlier return to work (7 to 10 days), and avoidance of a large scar. The elective procedure of choice for intractable duodenal ulcer is highly selective vagotomy, which has Figure 129-1 Model illustrating the most common surgical procedures used for peptic ulcer disease. Gastric ulcers must be sampled in four quadrants Gastric ulcers must be sampled in four quadrants Widely used,adequate results Best elective antiulcer procedure, 4-11% recurrence rate minimal morbidity (1 to 2% dumping and diarrhea), a mortality rate that approaches 0%, and a recurrence rate of 4 to 11%. The combination of truncal vagotomy and pyloroplasty, which should rarely be used in the elective setting, is reserved for those elderly or otherwise high-risk patients in whom a shorter operative procedure is advised. The primary goal of surgery is to close the perforation and prevent continuing peritoneal contamination and infection. Prospective, randomized clinical trials have shown that adding routine highly selective vagotomy is associated with a significant decrease in ulcer recurrence and subsequent need for operation but no increase in morbidity or mortality. Future randomized clinical trials are needed before this approach can be considered standard practice. Highly selective vagotomy should not be performed if the perforation is more than 24 hours old, severe peritoneal contamination exists, or the general condition of the patient is unstable. The preferred emergent operation for bleeding is suture control of bleeding by means of duodenotomy and highly selective vagotomy, except in the unstable patient in whom truncal vagotomy and pyloroplasty may be used. The operation of choice when a duodenal ulcer has caused gastric outlet obstruction is truncal vagotomy and antrectomy with gastroduodenal anastomosis. If the duodenum is involved in an inflammatory mass or is otherwise severely distorted, truncal vagotomy and gastrojejunostomy should be done, leaving the duodenum undisturbed. After operation for long-standing gastric outlet obstruction, postoperative delay in gastric emptying presents a serious problem. The choice of elective operation depends on the type of gastric ulcer (Table 129-3). The problem of an ulcerated cancer masquerading as a benign ulcer is more common than a benign gastric ulcer degenerating into a malignant one. With the advent of endoscopy, fewer patients diagnosed as having a benign ulcer have an ulcerated cancer. In the United States, carcinoma has been found in only 3% of resected gastric ulcers. Bleeding is a more serious complication in gastric ulcers than in duodenal ulcers. In a stable patient, the preferred procedure is distal gastrectomy that removes the ulcer and creates a gastroduodenal (Billroth I) anastomosis. Acid reduction and ulcer excision accomplished Behaves like duodenal ulcer More common in South America another approach, but this procedure is associated with very high recurrence rates in two types of gastric ulcers: those associated with duodenal ulcer and those located in the prepyloric area. In the less stable patient, ulcer excision alone or with vagotomy and pyloroplasty is recommended. If the ulcer cannot be excised, bleeding should be controlled by suture ligation; biopsy may be obtained if deemed safe or it may be postponed to subsequent endoscopy. For ulcers in the body of the stomach, some advocate that bleeding be controlled either by the combination of biopsy and oversewing of the ulcer or by excising the ulcer. The efficacy of this form of therapy has not been substantiated by published reports.
Several studies have localized the genetic defect to the chromosomal loci ret proto-oncogene, endothelin B, and endothelin 3. Absence of nitric oxide synthase and the consequent absence of the inhibitory mediator nitric oxide may cause the constant contraction of the affected bowel. The severity of symptoms and the age at diagnosis are related to the length of the aganglionic segment. Involvement of the entire rectum or additional parts of the colon results in constipation or obstipation in infancy, requiring emergent resection of the aganglionic bowel and a pull-through anastomosis to the anus. If a short segment of the distal rectum is aganglionic, the patient may not present with symptoms until adolescence or even adulthood. Abnormalities in anal physiology are a significant cause of constipation; impaired anal sphincter relaxation occurs relatively frequently in adults. In acquired megacolon, relaxation of the internal anal sphincter may be impaired if a large volume is not used to distend the rectum. Some patients have subtle histologic abnormalities in the myenteric plexus, suggesting that an acquired neuropathy may also account for the abnormal sphincter response. In the spastic pelvic floor syndrome (animus), the external anal sphincter and the puborectalis relax poorly or the levator ani contracts poorly, leading to impaired opening of the rectoanal angle (Chapter 143). This acquired condition, which occurs more often in multiparous women, can prevent normal stool evacuation. Impaired internal anal sphincter relaxation in an adult may respond to a posterior anal sphincter myomectomy. Slow Transit with Decreased Segmenting Contractions Patients with decreased segmenting contractions after stimulation have symptoms similar to those in patients with increased contractions. The colonic inertia form of the irritable bowel syndrome and primary colonic pseudo-obstruction may be a similar pathophysiologic disturbance. Postprandial increases in colonic motility are absent in both, but the colon is dilated in primary intestinal pseudo-obstruction, explaining the increased incidence of abdominal distention. Constipation is present in many patients with chronic, insulin-requiring diabetes mellitus, progressive systemic sclerosis, or thoracic spinal cord lesions. In patients with diabetes or spinal cord lesions, colonic smooth muscle can be stimulated with exogenous drugs, suggesting a neural lesion, not a myopathy. In progressive systemic sclerosis, the colon cannot increase intraluminal pressure after drug stimulation. In patients with neuropathy and normal smooth muscle function, prokinetic drugs have had some success. Colonic resection with an ileoanal anastomosis has successfully treated patients with colonic inertia who do not have motility disorders in the upper gastrointestinal tract. Some patients have functional, painless diarrhea with fecal urgency but with no associated anatomic or histologic abnormality of the gastrointestinal tract. These patients present with small frequent stools, consistent with a large bowel diarrhea; fecal incontinence is relatively frequent because their anal sphincters cannot retard evacuation of liquid stool. Lactose intolerance must be excluded either by history or by specific tests of lactose intolerance. The diarrhea is greater than that in the spastic irritable colon syndrome, and abdominal pain may be absent. Propagating contractions are increased and propagate into the rectum, possibly accounting for the increased urgency and fecal incontinence in these patients. The lack of segmenting contractions to impede forward movement or transit may exacerbate the urgency. Increased concentrations of fecal bile salts contribute to the functional diarrhea by irritating colonic sensory nerves. In treating functional diarrhea, antidiarrheal agents such as the opioid analogues, loperamide, and diphenoxylate decrease symptoms. If excess bile salts contribute to the diarrhea, low doses of cholestyramine may decrease the diarrhea. Surreptitious laxative abuse is a common but difficult to diagnose cause of functional diarrhea (see Chapter 227). Oxyphenisatin and bisacodyl stimulate increased numbers of propagating contractions and diarrhea. Patients may take these or other laxatives as a manifestation of a psychiatric disorder.
Because some of these conditions can be superimposed on underlying chronic essential hypertension, it is particularly important to remain alert for these diagnoses in patients who have been treated for prolonged periods but whose hypertension is progressively more difficult to control. Renovascular disease is the most common (1 to 2%) cause of curable/treatable secondary hypertension. Any lesion that obstructs either large or small renal arteries can cause renovascular hypertension. The most common and clinically important of these are intrinsic lesions of the large vessels (see Chapter 112) because they can be physically treated and the hypertension either cured or ameliorated. Of patients with renovascular hypertension, atherosclerotic disease is found in 75% overall and in nearly all elderly patients, whereas fibrous or fibromuscular disease is found in 25%, including the vast majority of younger patients. The usefulness of screening tests for renovascular hypertension is highly variable, so patients should be referred to high-volume centers for testing. Patients most likely to have renovascular hypertension include those with hypertension of abrupt onset, especially in the young or in late middle-aged or elderly patients; those with malignant hypertension or sudden acceleration of benign hypertension; and those who fail to respond to medical therapy. An upper abdominal bruit, particularly one that is systolic-diastolic or continuous in timing, is high pitched, and radiates laterally from the midepigastrium, occurs in one half to two thirds of patients with surgically proven renovascular hypertension. A definitive diagnosis of renal artery stenosis is made by selective renal angiography, which defines the anatomy of the stenotic renal artery and hence provides information needed to plan the approach to revascularization. The natural history of renal artery stenosis is progressive arterial occlusion with loss of renal function. For patients with obstruction of renal blood flow caused by an ostial stenosis at the origin of the renal artery and those who have unsuccessfully undergone balloon angioplasty, renal artery stents are useful in maintaining renal artery patency. Renal function and serum potassium levels must be monitored closely, particularly when therapy is initiated. Normal autoregulation of the glomerular filtration rate, which depends on an intact intrarenal renin-angiotensin system, is lost when the renin-angiotensin system is interrupted with these drugs. Renal function can deteriorate and renal mass can be lost very rapidly in patients with atherosclerotic disease who are treated medically. Significant reduction in renal size is the most sensitive index of loss of renal mass. Serial (every 3 to 6 months) estimates of renal size are important for monitoring patients who are receiving medical treatment for renovascular hypertension. Primary aldosteronism (see Chapter 240) and pheochromocytoma (see Chapter 241) are relatively rare causes of hypertension that are clinically important because the associated hypertension can usually be cured with appropriate surgical or targeted drug therapy. Approximately 50% of patients with obstructive sleep apnea (see Chapter 87) are hypertensive, whereas up to 30% of hypertensive patients have sleep apnea. Alternatively, hypertension and sleep apnea may simply share risk factors, such as age and obesity, and occur independently. A small percentage of women who use oral contraceptives experience the onset of hypertension, which resolves by stopping oral contraceptive therapy. The diagnosis of oral contraceptive-induced hypertension can be made by documenting the onset of hypertension de novo during contraceptive therapy and resolution of the hypertension upon drug withdrawal. This form of hypertension usually begins during the first year of taking oral contraceptives. Co-morbid conditions, principally target organ damage and major cardiovascular risk factors, that influence the choice of antihypertensive therapy have been demonstrated in 50 to 70% of patients with essential hypertension, particularly in the elderly. Other common conditions that may influence drug selection include benign prostatic hypertrophy and osteoporosis (see Table 55-6 (Table Not Available)). Hypertension is twice as common in diabetics as in the general population, and diabetics with hypertension have a greatly increased risk of cardiovascular disease when compared with either normotensive diabetics or hypertensives without diabetes. Calcium channel blockers, alpha-blockers, and low-dose diuretics are also preferred agents because of their favorable or neutral effects on glucose and lipid metabolism and on renal function. Potassium supplements and potassium-sparing diuretics should be used with caution in diabetics because of the frequent occurrence of hyporeninemic hypoaldosteronism and consequent hyperkalemia in patients with diabetic nephropathy. Older persons benefit more from antihypertensive treatment than younger people do, at least in the short term. However, older persons tend to be more sensitive to pharmacologic intervention, so antihypertensive medication should be prescribed cautiously at roughly half the usual recommended starting dose, and doses should be titrated upward slowly (6- to 8-week intervals). Low-dose diuretics and long-acting dihydropyridine calcium channel blockers are recommended as preferred agents because they have been shown in randomized clinical trials to prevent cardiovascular events and mortality in this group. Accordingly, short-acting calcium channel blockers and oral clonidine should be particularly avoided in this group.
Finally, central venous pressure measurements provide unreliable estimates of pulmonary vascular volume. The cardinal laboratory findings associated with volume contraction follow directly from the volume repletion mechanism summarized in Figure 102-2. The kidney initially responds to a decrease in effective circulating blood volume by reducing urine volume and sodium excretion. Severe degrees of volume contraction also reduce filtration rate and result in prerenal azotemia and a decrease in fractional excretion of sodium (see Chapter 100). The type of fluid, the route and rate of fluid administration, and the total amount of fluid to be given will vary with the particular circumstance. For example, a mild, non-persisting upper gastrointestinal hemorrhage may be treated appropriately by infusing normal saline, whereas a major, persisting upper gastrointestinal hemorrhage will generally require replacement with whole blood. If glucose metabolism is normal, infusing 5% dextrose in water (D5 W) is equivalent to administering solute-free water, which distributes uniformly in total body water. Because less than 10% of total body water is in the intravascular compartment, infusing 1 L of D5 W expands the intravascular volume by 75 to 100 mL, that is, by about 2%. Infusing 1 L of a normal saline solution increases blood volume by about 300 mL, or about 6%; the remaining portion is distributed in the interstitial compartment. Hypotonic sodium-containing salt solutions expand intravascular volume in a manner intermediate between that of D5 W and normal saline. Sodium-containing crystalloid solutions are indicated primarily in volume-contracted states secondary to renal or gastrointestinal sodium losses (see Table 102-2). Colloid-containing solutions, such as iso-oncotic albumin solutions and plasma, preferentially expand the intravascular compartment, because large molecules like albumin are mainly restricted to the intravascular space. This kind of fluid replacement is most helpful in burns, in which cutaneous protein losses are appreciable, and in circulatory collapse, in which rapid intravascular expansion is critical. In most other instances of volume contraction, using colloid-containing solutions is difficult to justify, since the half-life of infused albumin in ill patients is relatively short, only 4 to 6 hours, and the cost of colloid solutions such as iso-oncotic albumin is more than 50 times greater than that of an equal volume of crystalloid solution. Finally, blood-which contains formed elements-is the most potent expander of the intravascular space. In most hemorrhagic situations, the combination of packed red blood cells with either normal saline solutions or colloid solutions is adequate for volume replacement. Few circumstances occur in modern practice, with the possible exception of massive hemorrhagic shock, in which whole-blood therapy for volume expansion is used. In the preceding section we considered those disorders characterized by inadequate filling of the arterial tree that occurred because of true volume deficits. Clearly, the cardinal signs and symptoms of these disorders are referable to responses accompanying the integrated volume repletion reaction. There are also disorders in which inadequate arterial filling occurs in the absence of external fluid losses and which indeed are often associated with increased total body water. However, the signs and symptoms of these disorders mimic closely those that characterize true volume contraction. Table 102-3 lists three commonly encountered classes of derangements that may manifest clinically with tachycardia, acute hypotension, oliguria, azotemia, and a reduced fractional excretion of sodium. A profound collapse of cardiac output, due to acute myocardial infarction with pump failure (cardiogenic shock) or to acute pericardial tamponade, may clearly result in circulatory collapse. Circulatory collapse with its attendant signs and symptoms occurs when there is a sudden increase in the capacitance of the vascular bed, most notably in the venous part of the circulation. This kind of increase in ratio of vascular capacitance to vascular volume occurs most commonly in sepsis and cirrhosis with increased arteriovenous shunts and decreased systemic vascular resistance. Increased vascular capacitance also may be seen in circumstances in which peripheral vasodilators, particularly those having a postarteriolar locus of action, are administered injudiciously. Profound hypotension, tachycardia, progressive oliguria, and azotemia are also encountered when there is a translocation of fluid from vascular to interstitial compartments, presumably because of a sudden, profound increase in the permeability characteristics of peripheral capillaries or when there is decreased circulatory oncotic pressure such as in any disease process with hypoalbuminemia. Some common causes of increased translocation of vascular fluid without hypoalbuminemia having an etiologic role include infarction of the small or large intestine, extensive tissue trauma, acute pancreatitis, and rhabdomyolysis. An analogous mechanism-namely, a marked increase in the permeability of pulmonary capillaries-is also presumed to account for the formation of non-cardiogenic pulmonary edema in the adult respiratory distress syndrome.
Papilledema is occasionally seen, most often in comatose patients but occasionally as the only impressive finding of respiratory failure. A chest radiograph may reveal the presence of obvious chronic lung disease or superimposed acute pulmonary infiltrates; however, the chest roentgenogram may not be helpful except to eliminate competing diagnoses. Leukocytosis suggests infection, but severe leukoerythroblastic responses may follow the stress of severe hypoxemia. Principles of patient care that apply to most cases include applying immediate life-saving measures; determining the precipitating factors; treating the airways dysfunction; and monitoring. Appropriate life-saving measures for acute respiratory failure center on the immediate correction of hypoxemia, need for emergency intubation or assisted ventilation, and adequate circulatory support. If, as in most cases, the patient is alert or only minimally confused and has a stable cardiovascular status, low-flow O2 is the principal therapy. The physician must closely follow blood gas measurements (Table 88-12), systemic arterial pressure, respiratory rate, vital capacity, cardiac rhythm, urinary output, hemoglobin levels, and serum electrolyte levels. Occasionally, inadvertent or surreptitious sedative consumption or factors such as pneumothorax, cardiac arrhythmias, left ventricular failure, or dehydration may contribute. If adequate oxygenation can be maintained without major worsening of respiratory acidosis, conservative measures can usually be applied to reverse all of these precipitating conditions (Table 88-13. Respiratory stimulants are rarely effective to reduce hypercapnia because minute ventilation is normal or increased and mechanical work is already excessive. Most patients hospitalized with hypercapnic-hypoxic respiratory failure improve after conservative therapy without needing artificial ventilatory support. If a patient continues to deteriorate, however, assisted ventilation is indicated. High respiratory rates (>36 per minute), excessive use of accessory muscles, paradoxical thoracoabdominal movement, a subjective sense of exhaustion, and even minor mental status changes should be considered probable indications. If hypoventilation cannot be effectively reversed by mechanical assistance of some type, an endotracheal tube must be inserted. Intubation results in laryngeal and tracheal irritation, loss of effective cough, and increased risk of infection. With careful handling, endotracheal tubes may be kept in place for at least 2 weeks (see Chapter 93). When artificial ventilation is required for more than 2 weeks, a tracheostomy is often required. The most important indication for early tracheostomy is the presence of copious, tenacious secretions that cannot be adequately removed through the endotracheal tube. Tracheostomy carries some risk of bleeding, pneumothorax, and local infection and an increased incidence of aspiration. Short-term outcome following acute hypoxic respiratory failure is generally good (see Table 88-1). The long-term prognosis is dictated by underlying disease and the functional impairment before acute respiratory failure developed. If historical information is not available, however, a specific diagnosis may be difficult, because many end-stage primary lung diseases overlap clinically. Obstruction can be separated from restriction (see Chapter 72), although patients may not be able to perform the necessary rigorous pulmonary function tests. At times, superimposed infection, pleural disease, or previous surgery also blurs these distinctions. In the most severe cases of chronic hypoxic respiratory failure, progressive lung destruction also impairs ventilation, and hypercapnia develops. Many patients with chronic hypoxic respiratory failure have end-stage fibrosis (honeycomb lung) (see Chapter 78). Supportive care includes oxygen for severe hypoxia and diuretics for excessive edema. Various O2 -conserving devices are available and may allow for more cost-effective supplementation and longer periods away from home. If patients are younger than 60 years and have no other significant problems, lung transplantation (see Chapter 89) should be considered. A variety of diseases lead to chronic hypercapnic respiratory failure (see Chapters 74 and 75). Using these devices during sleep may improve quality of life and prolong survival, especially in patients with neuromuscular diseases. Younger patients with alpha1 -antitrypsin deficiency (see Chapter 75), cystic fibrosis (see Chapter 76), and other causes of bronchiectasis (see Chapter 77) are good candidates for lung transplantation (see Chapter 89).
Additional information: