"Discount 5 mg prinivil with amex, arrhythmia in pregnancy".
Y. Aidan, M.A., M.D., Ph.D.
Clinical Director, Pennsylvania State University College of Medicine
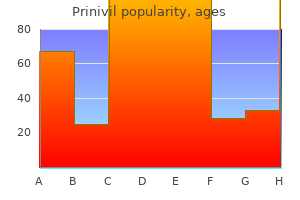
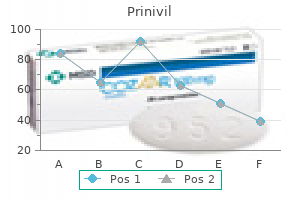
The dairy products provided <1300 mg Ca/d; it was assumed that the remainder of the diet provided <200 mg. TreatmentControl, Adherence Evaluations Outcome assessment/ Results and Conclusions severity were not significantly different between the 2 treatment periods. Conclusion(s): Authors conclude that the symptoms resulting from lactose maldigestion are not a major impediment to the ingestion of a dairy-rich diet supplying <1500 mg Ca/day. Quality of the Study and 2 in the lactose digestion group believed that the ingestion of dairy products resulted in appreciable abdominal symptoms. Subjects reporting symptoms based on ratings (0=none to 4=severe), 8 hours after lactose challenge. Conclusion(s): Subjective ratings of the severity of symptoms (cramps, belching, flatulence, diarrhea) were significantly decreased with the lactose treatment Allocation concealment: unclear Blinding: Double Intent-to-treat analyses: 100% followup Study withdrawals adequately described: no withdrawals reported D-360 Appendix Table D8. Evidence table for blinded lactose intolerance treatment studies: Question 4 (continued) Author, Year, Study Design, Study Sponsorship, Country, Length of Followup Subject Selection, Data Source, Methods to Measure Outcomes, Inclusion/Exclusion Criteria symptoms 8 hours after consuming tests and then every 8 hours until 24 hours elapsed. Exclusion criteria: Subject Characteristics Treatment-Active, Adherence Evaluations TreatmentControl, Adherence Evaluations Outcome assessment/ Results and Conclusions compared to placebo. Race/ethnicity: Asian 69%; black 8%; Hispanic 15%; white 8% 240 mL lactose hydrolyzed milk (lactose totaling 11. Mean symptom severity scores ranked scale on a scale as follows: 0=none; 1=trivial; 2= mild; 3=moderate; 4= strong; 5= severe. Conclusion(s): Authors concluded lactase-nonpersistent subjects can tolerate two cups of milk per day without appreciable symptoms. Allocation concealment: unclear Blinding: Double Intent-to-treat analyses: 100% followup Study withdrawals adequately described: no withdrawals reported D-361 Appendix Table D8. Methods to measure outcomes: Subjects rated symptoms (bloating, borborygmi, abdominal pain or cramps, and subjective impressions of rectal gas excretion) on 4 occasions daily (morning, noon, afternoon, night) during the baseline and the 2 test periods. Race/ethnicity: not reported Comorbidities: not reported Cointerventions: not reported 200 mL lactose-free milk (0. Allocation concealment: unclear Blinding: Double blinding attempted, although it was noted that full fat milk can be readily discerned from fatfree milk. Evidence table for blinded lactose intolerance treatment studies: Question 4 (continued) Author, Year, Study Design, Study Sponsorship, Country, Length of Followup Subject Selection, Data Source, Methods to Measure Outcomes, Inclusion/Exclusion Criteria symptom followup during the test day. Exclusion criteria: No gastrointestinal diseases, were not on medications, on antibiotics at least two months prior to study, or had irritable bowel syndrome. Data source: 39 Finnish subjects with lactose maldigestion and 15 lactose digesters. Inclusion criteria: Lactose maldigestion based on a positive lactose H2 breath test (39%) or lactose tolerance test with ethanol (61%). Lactose maldigesters who experienced at least moderate gastrointestinal symptoms, i. Conclusion(s): A marked difference in the fat content of milk did not affect the symptoms of lactose intolerance. Maldigesters reported significantly more abdominal bloating and abdominal pain than the digesters. There was no difference in the mean severity of the reported symptoms between the test milks and the lactose-free milk in the group of Allocation concealment: unclear Blinding: Double Intent-to-treat analyses: 100% followup Study withdrawals adequately described: no withdrawals reported D-363 Appendix Table D8. Evidence table for blinded lactose intolerance treatment studies: Question 4 (continued) Author, Year, Study Design, Study Sponsorship, Country, Length of Followup Subject Selection, Data Source, Methods to Measure Outcomes, Inclusion/Exclusion Criteria flatulence, were selected for in the study group. Exclusion criteria: No gastrointestinal diseases or on antibiotics one month prior to study. The same proportion (64%) of the maldigesters experienced symptoms after both the lactose-free milk and the milk with 7 g lactose. Conclusion(s): Gastrointestinal symptoms in most lactose maldigesters are not induced by lactose when small amounts (0. Quality of the Study Cointerventions: not reported Data source: 30 American subjects who reported severe lactose intolerance with consistent related symptoms. Subjects were classified as having lactose mal absorption if their breath H2 concentrations increased by more than 10 parts per million -6 (ppm) (0.
What are the intermediate, clinical, and adverse outcomes after treatments for lactose intolerance? In the clinical situation, a graduated definition of a potentially lactose intolerant subject, might be as follows: 1. The quantity of lactose routinely ingested by the individual that causes symptoms. The quantity of lactose ingested in some situations by the individual causes the above symptoms. The quantity of lactose that the individual would like to ingest (but does not due to fear of symptoms) causes the above symptoms. The quantity of lactose ingested in the course of obtaining 1,500 mg/day of calcium entirely via lactose-containing dairy products causes the above symptoms. We excluded studies that were published in non English languages and small case reports or descriptive case series with less than 100 subjects unless there are no reliable data from other higher quality studies. Only larger studies (at least 100 participants) of populations outside of the United States were included. The 50 gram dose of lactose, the quantity present in a quart of milk, was selected because this quantity of milk provides the maximal recommended daily intake of calcium (1,500 mg), and this dosage approaches the maximal daily volume of milk likely to be ingested by most Americans digestive. We excluded congenital lactase deficiency, developmental lactase deficiency among pre-term infants, milk allergies commonly seen in infants, and acute lactose intolerance (<30-60 days duration) due to such things as antibiotic use or illness. Primary lactase deficiency is also referred to as adulttype hypolactasia, lactase nonpersistence, or hereditary lactase deficiency. We attempted to review differences in prevalence in individuals of different age groups defined as: Preschool Children: 4-5 years, Children: 6-12 years, Adolescents: 13-18 years, Adults: 19-44 years, Middle Aged: 45-64 years, Aged: 65+ years, and Elderly Adults: 80 and over. Studies assessing only intestinal biopsies were reviewed for quality and applicability. A critical aspect of this question was to clearly define and differentiate between: (1) lactase nonpersisters, (2) lactose malabsorbers, and (3) lactose intolerance. There is no objective laboratory test (intestinal biopsies are rarely done and only assess lactase enzyme levels; physiologic tests. We defined dairy exclusion diets as low lactose diets that generally eliminate only milk and milk products or lactose free diets that eliminate all lactose products, including foods that are prepared with milk, both at home and in commercially packaged foods. We defined interventions when patients followed lactose free diets prescribed by health care professionals. We defined exposure when subjects followed low lactose or lactose free diets without recommendations from health care professionals. We included indirect evidence of the effect of dairy exclusion on health outcomes by including studies of populations known or suspected of having low dairy intake. We included studies in primary and specialty outpatient settings and population based settings. We reviewed co-interventions in studies that reported patient outcomes after low lactose and lactose free diets. Studies that examined patient outcomes among healthy populations consuming dairy exclusion (or very low dairy) diets. Meta-analyses and systematic reviews that synthesized the association between dairy (dietary Ca++) intake and patient outcomes. We analyzed the adjustment for the known factors that could confound the association between lactose intake and bone health, including age, gender, race, menopausal status in women, external calcium supplementation, renal function, and smoking. The main long-term health concern related to lactose exclusion diets from this report was predominately related to potentially low calcium and vitamin D intake associated with these diets. We reviewed whether the studies that examined patient outcomes in association with low dietary milk intake addressed calcium intake from other sources and supplementation with Ca++ or vitamin D. This provided us with contextual information regarding the potential role of low lactose or lactose free diet on bone health independent of other sources of Ca++ or vitamin D. Key Question 3: What amount of daily lactose intake is tolerable in subjects with diagnosed lactose intolerance? We quantified the type and severity of symptoms and the amount and type of lactose causing patient reported symptoms. We assessed for the percentage reporting these outcomes as well as scores reported on symptom questionnaires. If there are gaps in evidence related to 32 amount and type of daily lactose intake, symptoms were defined as patient reported: gas/flatulence, abdominal pain, bloating, and diarrhea. We evaluated the following interventions: · Commercially available lactase · Prebiotics and probiotics · Incremental lactose loads for colonic adaptation · Other dietary strategies Comparators.
Taken together, the alveoli and capillary membranes form a respiratory membrane that is approximately 0. Asthma is a chronic disease characterized by inflammation and edema of the airway, and bronchospasms (that is, constriction of the bronchioles), which can inhibit air from entering the lungs. In addition, excessive mucus secretion can occur, which further contributes to airway occlusion (Figure 22. Cells of the immune system, such as eosinophils and mononuclear cells, may also be involved in infiltrating the walls of the bronchi and bronchioles. Symptoms of an asthma attack involve coughing, shortness of breath, wheezing, and tightness of the chest. Symptoms of a severe asthma attack that requires immediate medical attention would include difficulty breathing that results in blue (cyanotic) lips or face, confusion, drowsiness, a rapid pulse, sweating, and severe anxiety. The severity of the condition, frequency of attacks, and identified triggers influence the type of medication that an individual may require. Short-term, fast-acting drugs that are used to treat an asthma attack are typically administered via an inhaler. For young children or individuals who have difficulty using an inhaler, asthma medications can be administered via a nebulizer. The main function of the lungs is to perform the exchange of oxygen and carbon dioxide with air from the atmosphere. To this end, the lungs exchange respiratory gases across a very large epithelial surface area-about 70 square meters-that is highly permeable to gases. Gross Anatomy of the Lungs the lungs are pyramid-shaped, paired organs that are connected to the trachea by the right and left bronchi; on the inferior surface, the lungs are bordered by the diaphragm. The diaphragm is the flat, dome-shaped muscle located at the base of the lungs and thoracic cavity. The right lung is shorter and wider than the left lung, and the left lung occupies a smaller volume than the right. The cardiac notch is an indentation on the surface of the left lung, and it allows space for the heart (Figure 22. The apex of the lung is the superior region, whereas the base is the opposite region near the diaphragm. A bronchopulmonary segment is a division of a lobe, and each lobe houses multiple bronchopulmonary segments. Each segment receives air from its own tertiary bronchus and is supplied with blood by its own artery. Some diseases of the lungs typically affect one or more bronchopulmonary segments, and in some cases, the diseased segments can be surgically removed with little influence on neighboring segments. A pulmonary lobule is a subdivision formed as the bronchi branch into bronchioles. An interlobular septum is a wall, composed of connective tissue, which separates lobules from one another. Blood Supply and Nervous Innervation of the Lungs the blood supply of the lungs plays an important role in gas exchange and serves as a transport system for gases throughout the body. In addition, innervation by the both the parasympathetic and sympathetic nervous systems provides an important level of control through dilation and constriction of the airway. Blood Supply the major function of the lungs is to perform gas exchange, which requires blood from the pulmonary circulation. This blood supply contains deoxygenated blood and travels to the lungs where erythrocytes, also known as red blood cells, pick up oxygen to be transported to tissues throughout the body. The pulmonary artery is an artery that arises from the pulmonary trunk and carries deoxygenated, arterial blood to the alveoli. The pulmonary artery branches multiple times as it follows the bronchi, and each branch becomes progressively smaller in diameter. As they near the alveoli, the pulmonary arteries become the pulmonary capillary network.
Syndromes
- Shock
- Fluids and electrolytes
- Excessive height (when excess growth hormone production begins in childhood)
- Psoriasis
- Does anything make you feel worse?
- Cough
- Nausea and vomiting, possible with blood
- Endoscopic retrograde cholangiopancreatography (ERCP) (can also determine cause)
While the epidural space extends only up to the foramen magnum, the subdural space extends all the way upward. Subdural block should be recognized by an unexpected increase in anesthesia level and presentation with slow onset, patchy blockade, minimal sacral analgesia, cranial nerve palsies, and a relative lack of sympathetic blockade. Subsequent injection of large volumes of local anesthetic into the subdural space may rupture the arachnoidal mater and exert intrathecal effects. Katarina Jankovic mL), low-concentration formulation of bupivacaine/fentanyl will initiate good analgesia. This method has a rapid onset, so that the patient is comfortable and can even be ready for cesarian section within 5 minutes. If vaginal delivery is unsuccessful and caesarian section is necessary, how should one proceed with intraand postoperative analgesia? Our patient from the beginning of the chapter has been monitored for fetal heart rate, and the obstetrician is indicating urgent cesarian section due to fetal distress. Then you might think about using spinal instead of general anesthesia, since it is easy, cheap, safe, and provides prolonged analgesia. Over the past 15 years, there has been a large increase in the number of cesarian sections done under regional anesthesia. It is therefore tempting to advocate that general anesthesia is no longer indicated, but certain factors must be taken into account when changing the standard anesthesia technique from general to spinal anesthesia. It is important to remember that when spinal anesthesia is used, the standard of care cannot be lower than for general anesthesia. The work-up for the mother having an elective or emergency cesarian section is the same regardless of the anesthesia plan. This must include preoperative fasting, if possible, and preparation of gastric content with appropriate antacids. The anesthetist must have access to all the equipment (including difficult airways equipment) and recovery facilities required for both techniques. Spinal anesthesia is probably safer (one study calculated 16 times safer) than general anesthesia, provided it is performed carefully with good knowledge of maternal physiology. Difficult airways and obesity-related edema become less of an issue, but remember that a pregnant woman lying supine can become hypotensive, even without augmenting the problem by giving local anesthetics intrathecally. Poor management of this problem can cause severe hypotension, vomiting, and loss of consciousness, which can lead to aspiration of gastric contents. Occasionally, a parturient reaches the second stage of labor before neuraxial analgesia is requested. The patient may not have wanted an epidural catheter earlier, or the fetal heart rate tracing or position may necessitate assisted delivery. Initiation of epidural analgesia is still possible at this point, but the prolonged latency between catheter placement and start of adequate analgesia may make this choice less desirable than a spinal technique. On the other hand, the initiation of an epidural catheter cannot be done be too early. The argument that early catheter placement may prolong the first stage of labor has not be confirmed in studies. If an epidural is used, ultra-low concentrations of local anesthetics may not be adequate to relieve the intense pain of the second stage. Some medical conditions can cause additional problems, all related to poor compensatory response to rapid change in afterload in low cardiac output states. Minimal preload of 200500 mL is good enough in most situations in combination with a vasopressor. There are certain situations when a general anesthetic will be more appropriate than a regional one. These situations include maternal refusal of regional blockade, coagulopathy, low platelet count, anticipated or actual severe bleeding, local infection of the site of insertion of the spinal or epidural needle, anatomical problems, and certain medical conditions. Lack of time is the most common reason to choose general anesthesia, although for a skilled clinician, time is not an issue. If there is an epidural catheter in place, assessment and top-up should not take more than 10 minutes, which is usually more than enough time for the majority of circumstances. Maternal hypotension is a common complication of blockade of sympathetic nerves, most characteristically cardiac sympathetic nerves.