Tue Ngo, M.D., M.D.H.
- Infectious Diseases Fellow
- Division of Infectious Diseases
- Vanderbilt University School of Medicine
- Nashville, Tennessee
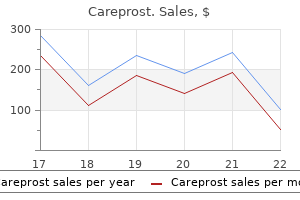
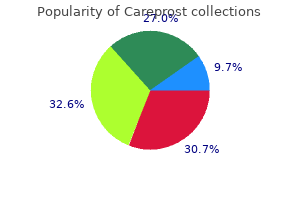
Treatment of fibrous dysplasia consists of curettage medicine ball slams discount careprost online mastercard, fracture restore and prevention of deformities counterfeit medications 60 minutes purchase careprost cheap. These lesions may be divided into four main clinicopathologic subtypes including (1) calvarial and mandibular osteomas treatment example buy careprost 3ml low price, (2) osteomas of the sinonasal and orbital bones chi royal treatment purchase careprost without prescription, (3) bone islands occurring in medullary bone and (4) floor osteomas of lengthy bones medications similar to abilify buy discount careprost online. Microscopically crohns medications 6mp careprost 3 ml, bland spindle cells are arranged in an interlacing, whorled pattern in which multinuclear giant cells and foamy macrophages could also be seen. The rare symptomatic or expanded lesions are handled with curettage and bone grafting. Nonossifying Fibroma Is a Solitary Lesion of Childhood Nonossifying fibroma, also termed fibrous cortical defect, is a benign tumor that occurs in the metaphysis of a protracted bone-most commonly, the tibia or femur. Whether nonossifying fibroma is a neoplasm or developmental Osteoid Osteoma Is a Benign, Painful Lesion Osteoid osteoma is composed of osseous tissue (the nidus) and surrounded by a halo of reactive bone formation. Osteoid osteoma regularly arises in the cortex of the diaphysis of the tubular bones of the leg. Chromosomal evaluation of a few cases has disclosed abnormalities of chromosome 22q13 and loss of part of 17q, which means that osteoid osteomas are neoplasms. Microscopically, the cartilaginous tissue is properly differentiated with sparse chondrocytes. Microscopically, the tumor consists of thin, irregular, trabeculae inside a cellular granulation tissue containing osteoblasts and osteoclasts. It represents one fifth of all bone cancers and is most frequent in adolescents between 10 and 20 years old, affecting boys more often than ladies (2:1). There are additionally many other chromosomal and molecular abnormalities pertaining to apoptosis, replicative potential, insensitivity to growth inhibitory alerts and cell cycle regulation. Osteosarcoma can develop in adults and kids previously subjected to external, therapeutic radiation for an additional tumor corresponding to lymphoma. When osteosarcomas come up in older sufferers, they nearly at all times occur within the context of Paget disease or radiation publicity. Several pre-existing benign bone lesions are related to an elevated risk of developing osteosarcoma, including fibrous dysplasia, osteomyelitis and bone marrow infarcts. It is usually exacerbated by ingesting alcohol and is promptly relieved by aspirin, probably due to the excessive prostaglandin content of the tumor and nerve fibers throughout the tumor. Solitary Chondroma Features Hyaline Cartilage Solitary chondroma (enchondroma) is a benign, intraosseous tumor composed of well-differentiated hyaline cartilage. A photomicrograph reveals pleomorphic malignant cells, tumor large cells and mitoses (arrow). Radiologic proof of bone destruction and bone formation is characteristic, the latter representing neoplastic bone. The neoplastic tissue may invade and break through the cortex, spread into the marrow cavity or develop into the epiphysis, even reaching the joint house. Histologic examination reveals malignant cells with osteoblastic differentiation producing woven bone Often, foci of malignant cartilage cells or pleomorphic large cells are intermixed. In areas of osteolysis, nonneoplastic osteoclasts are discovered on the advancing entrance of the tumor. As pain intensifies, the realm becomes swollen and tender, and the adjoining joint becomes functionally restricted. Serum alkaline phosphatase is increased in half of the patients and may lower after amputation, solely to improve once more with recurrence or metastasis. Chondrosarcoma Is a Cartilaginous Malignancy Whose Grade Determines Prognosis Chondrosarcoma is a malignant tumor of cartilage that arises from preexisting cartilage rests or enchondroma. Some sufferers have a historical past of enchondromas, solitary osteochondroma or hereditary multiple osteochondromas. Chondrosarcoma is the second most common main malignant bone tumor, occurring extra generally in males than in ladies (2:1). It is most regularly seen within the fourth to sixth many years (average age, 45 years). There most likely is a special molecular mechanism resulting in tumor improvement between central chondrosarcoma and secondary peripheral chondrosarcoma (tumors arising within the cartilaginous cap of an osteochondroma) (see below). Resected gross specimen demonstrates lobulated hyaline cartilage with calcifications, ossification and focal liquefaction. Chondrosarcoma is doubtless certainly one of the few tumors during which microscopic grading has a major prognostic worth. The different mononuclear cell inhabitants has chromosomal abnormalities and molecular alterations in oncogenes corresponding to p53 and c-myc. The neoplasm is usually a lytic lesion that grows slowly sufficient to allow a periosteal reaction. It usually occurs in the third and fourth decades, has a slight predilection for girls and seems to be extra widespread in Asia than in Western nations. The tumor extends to the subchondral bone plate and breaks by way of cortex into the delicate tissue. Photomicrograph shows osteoclast-type big cells and plump, oval, mononuclear cells. Microfractures and pathologic fractures are frequent, due to thinning of the cortex. The tumor is often handled with thorough curettage and bone grafting, though more aggressive management, including en bloc resection and even amputation, could additionally be necessary. Most of those patients could get pleasure from an primarily normal life span, particularly if the metastatic deposits are few and can be surgically removed. The tumor could infiltrate the medullary spaces without destroying the bony trabeculae. In many instances, the tumor mass penetrates the periosteum and extends into the delicate tissues. The mononuclear ("stromal") cells are plump and oval, with massive nuclei and scanty cytoplasm. Large osteoclastic large cells, some with more than one hundred nuclei, are scattered all through the richly vascularized stroma. A medical radiograph demonstrates expansile cortical destruction with poor circumscription and a delicate interrupted periosteal reaction (arrows). A biopsy specimen reveals pretty uniform small cells with spherical, dark blue nuclei and poorly defined cytoplasm. The illness may be divided into two major varieties: (1) inflammatory arthritis, often involving the synovium and mediated by inflammatory cells Osteoarthritis is a slowly progressive destruction of articular cartilage that impacts weight-bearing joints and fingers of older persons or the joints of youthful individuals subjected to trauma. Osteoarthritis is the one most common form of joint disease and the most important type of noninflammatory arthritis. Many circumstances of major osteoarthritis exhibit a familial clustering, suggesting a hereditary predisposition. Metastatic Tumors Are the Most Common Malignant Tumors in Bone Most metastatic lesions to bone are carcinomas, particularly of the breast, prostate, lung, thyroid and kidney. The vertebral column is, by far, the commonest web site in adults, and the appendicular skeleton is the typical location in youngsters. Some tumors (thyroid, gastrointestinal tract, kidney, neuroblastoma) produce mostly lytic lesions by stimulating osteoclasts. A few neoplasms (prostate, breast, lung, stomach) provoke osteoblastic components to make bone, creating dense foci on radiographs. However, most deposits of metastatic most cancers within the bones have mixtures of both lytic and blastic components. Progressive degradation of articular cartilage leads to joint narrowing, subchondral bone thickening and ultimately a nonfunctioning, painful joint. Secondary osteoarthritis has a identified underlying cause, including congenital or acquired defects of joints, trauma, crystal deposits, an infection, metabolic diseases, endocrinopathies, inflammatory diseases, osteonecrosis and hemarthrosis. Damage to the coarse cancellous bone results in an elevated unit load on the cartilage due to a rise in the stiffness of subchondral bone Proteoglycan content and aggregation decrease, and glycosaminoglycan chain size is reduced. Although matrix synthesis by chondrocytes is increased early in osteoarthritis, protein synthesis ultimately declines, as does chondrocyte replication. Apparently, the cells attain a point at which they fail to respond to reparative stimuli. Collagenase is absent in normal cartilage, however is present in osteoarthritic cartilage. The earliest adjustments of osteoarthritis are the loss of proteoglycans from the floor of the articular cartilage, which is seen histologically as decreased metachromatic staining accompanied by empty lacunae, indicating that chondrocytes have died. Viable chondrocytes enlarge, combination into teams or clones and turn out to be surrounded by basophilic staining matrix known as the territorial matrix. Osteoarthritis might arrest at this stage for a number of years before progressing to the following stage, which is characterised by fibrillation. Eventually, pieces of articular cartilage break off and lodge in the synovium, inducing inflammation and a foreign-body large cell response. As the crack extends downward, neovascularization from the epiphysis and subchondral bone extends into the area of the crack, inducing subchondral osteoclastic bone resorption. As neovascularization progressively extends into the world of the crack, mesenchymal cells invade and fibrocartilage varieties as a poor substitute for the articular hyaline cartilage. The subchondral bone turns into uncovered and burnished because it grinds against the opposite joint floor, which is undergoing the identical process. These thick, shiny, easy areas of subchondral bone are referred to as eburnated (ivorylike) bone. In some areas, the eburnated bone cracks, allowing synovial fluid to extend from the joint surface into the subchondral bone marrow, the place it eventually produces a subchondral bone cyst An osteophyte develops, usually in the lateral portions of the joint, when the mesenchymal tissue of the synovium differentiates into osteoblasts and chondroblasts to kind a mass of cartilage and bone. They might occur at lateral edges of intervertebral disks, the place they produce the "lipping" pattern seen on radiographs as osteoarthritis of the spine. In the fingers, osteophytes on the distal interphalangeal joints are termed Heberden nodes. The involved joints could also be enlarged, tender and boggy and will reveal crepitus. Below the tidemark, new vessels develop in from the epiphysis and fibrocartilage (D) is deposited. A femoral head with osteoarthritis exhibits a fibrocartilaginous plug (far right) extending from the marrow onto the joint surface. A section through the articular floor of an osteoarthritic joint demonstrates focal absence of the articular cartilage, thickening of subchondral bone (left) and a subchondral bone cyst. Pain is normally a sign of significant joint destruction and arises in the periarticular structures because articular cartilage lacks a nerve supply. Discomfort can be brought on by brief periods of stiffness, which is regularly skilled in the morning or after periods of minimal activity. Restricted joint motion signifies extreme disease and will result from joint or muscle contractures, intraarticular unfastened bodies, large osteophytes and loss of the joint floor congruity. Therapy is directed at particular orthopedic situations and contains exercise, weight reduction and different supportive measures. Commonly, joints of the extremities are concurrently affected, often symmetrically. The broad spectrum of clinical manifestations ranges from barely discernible to extreme, destructive, mutilating disease. Immune complexes containing such antibodies are produced within the synovium and activate complement. This will increase vascular permeability and the uptake of immune complexes by leukocytes, which in flip launch lysosomal enzymes, reactive oxygen species and different injurious merchandise. Activated macrophages in the synovium continue to current antigens to T cells, thereby continuing the manufacturing of cytokines, which amplify inflammation and tissue injury. In addition, immune-complex deposits are present within the articular cartilage and the synovium. Abundant T lymphocytes in rheumatoid synovium are incessantly Ia positive ("activated") and of the helper sort. T cells might immediately or indirectly interact with macrophages through manufacturing of cytokines that inhibit migration and proliferation of the latter. Vascularity will increase, with exudation of fibrin into the joint area, which may result in small fibrin nodules that float within the joint (rice bodies). In this course of, the synovium creeps over the surface of the articular cartilage and adjacent buildings. This inflammatory synovium, now containing mast cells, is termed a pannus (cloak). The pannus covers the articular cartilage and isolates it from the synovial fluid. Lymphocytes combination into plenty and finally develop follicular centers The pannus erodes the articular cartilage and adjoining bone, probably by way of the motion of collagenase produced by the pannus Eventually, the joint is destroyed and undergoes fibrous fusion, termed ankylosis. A attribute lesion, termed the rheumatoid nodule, is present in extra-articular places. The influx of lymphocytes, plasma cells and mast cells, along with neovascularization and edema, results in hypertrophy and hyperplasia of the synovium. Eventually, the joint is destroyed and becomes fused, a situation termed ankylosis. Hyperplastic synovium from a patient with rheumatoid arthritis shows quite a few finger-like projections with focal pale areas of fibrin deposition. A microscopic view reveals distinguished lymphoid follicles (Allison-Ghormley bodies), synovial hyperplasia and hypertrophy, villous folds and thickening of the synovial membrane by fibrosis and inflammation. A larger energy view of the inflamed synovium demonstrates hyperplasia and hypertrophy of the liner cells. Beyond the macrophages is a circle of lymphocytes, plasma cells and different mononuclear cells. The total appearance resembles a peculiar granuloma surrounding a core of fibrinoid necrosis. Rheumatoid nodules are sometimes found in visceral organs, similar to the heart, lungs and intestinal tract and even the dura. Most patients describe slowly growing fatigue, weight reduction, weakness and imprecise musculoskeletal discomfort, which finally localizes to the concerned joints. Unabated illness causes progressive destruction of the joint surfaces and periarticular structures.
In some instances of unstable angina medications knee buy careprost 3ml online, episodes of chest ache turn out to be progressively more frequent and longer in duration over a 3- to 4-day period medicine park ok discount careprost 3ml online. Unstable angina can additionally be termed preinfarction angina treatment 4 stomach virus buy discount careprost line, accelerated angina or "crescendo" angina symptoms 0f low sodium cheap careprost 3ml free shipping. Without pharmacologic or mechanical intervention to "open up" the coronary narrowing treatment for depression order cheap careprost on-line, many patients with unstable angina progress to myocardial infarction treatment jiggers purchase generic careprost online. The improvement of an infarct is related to the length of ischemia and the metabolic rate of the ischemic tissue. In experimental coronary artery ligation, foci of necrosis form after 20 minutes of ischemia and turn out to be more intensive because the period of ischemia lengthens. Contractile impairment in these patients is due to irreversible lack of myocardium from previous infarcts and hypoperfusion of surviving muscle, which finally ends up in chronic ventricular dysfunction. In many circumstances, lethal arrhythmia is in all probability going triggered by acute ischemia without overt myocardial infarction. However, the presence of a healed infarct or ventricular hypertrophy will increase the danger that an episode of acute ischemia will initiate a life-threatening ventricular arrhythmia. Any certainly one of these components considerably increases the danger of myocardial infarction, however a mixture of a number of components augments the risk more than sevenfold (see Chapter 8). In 1950, the age-adjusted annual dying fee from myocardial infarction in the United States was 226 per 100,000 population-50 years later, it was one hundred fifty. This shift displays many components, together with reduced smoking, lower dietary saturated fat and new medicine that control hypertension, scale back ldl cholesterol and lyse coronary thrombi. The risk of ischemic coronary heart disease will increase in proportion to the variety of cigarettes smoked. Increased levels of plasma factors involved in thrombosis or the inhibition of thrombolysis, such as fibrinogen, plasminogen activator inhibitor-1, homocysteine and decreased fibrinolytic activity, contribute to the chance of myocardial infarction. Levels of selected serum markers of inflammation, similar to C-reactive protein, are also predictors of ischemic heart disease. During the previous a number of years, there was a outstanding increase within the incidence of type 2 diabetes within the United States, which mirrors an identical increase in weight problems (see Chapter 22). Ischemic heart disease is a consequence of each sort 1 and sort 2 diabetes, and the chance is twofold to threefold greater than in nondiabetic people. Other danger elements for ischemic coronary heart illness embrace: Obesity: In a serious, longitudinal examine of one inhabitants (Framingham Heart Study), weight problems was an impartial threat issue for cardiovascular disease, with an increased danger for overweight persons over those that are lean of two to 2. The genetic basis for this familial threat could interact with the other risk components. Use of oral contraceptives: Women over 35 years who smoke cigarettes and use oral contraceptives have a modestly increased incidence of myocardial infarction. In one research that utilized exercise testing, the least-fit quartile of persons had six times the chance of myocardial infarction than did those in the fittest quartile. Causes of Ischemic Heart Disease Decreased Supply of Oxygen Conditions that influence the supply of blood Atherosclerosis and thrombosis Thromboemboli Coronary artery spasm Collateral blood vessels Blood stress, cardiac output and coronary heart fee Miscellaneous: arteritis The anaerobic glycolysis used by skeletal muscle underneath circumstances of extreme bodily exertion is inadequate to sustain cardiac contraction. Ischemic heart illness is caused by an imbalance between the oxygen calls for of the myocardium and the availability of oxygenated blood. Conditions that elevate blood pressure or cardiac output, corresponding to exercise or pregnancy, increase oxygen demand by the myocardium, which can lead to angina pectoris or myocardial infarction in the compromised organ. The elevated metabolic fee and tachycardia in patients with hyperthyroidism are additionally accompanied by elevated oxygen demand as well as a rise in the workload of the guts (Table 11-3). Here, the features of particular significance to ischemic heart illness are briefly mentioned. In a normal heart, the big coronary arteries present almost no resistance to blood move. To compensate for lowered perfusion strain, intramural microvessels dilate, thereby maintaining regular resting blood circulate. In sufferers with long-standing angina pectoris, the extent and distribution of collateral circulation exerts an important influence on the risk of acute myocardial infarction. Although myocardial infarction usually happens during bodily demanding actions, such as operating or shoveling snow, many infarcts happen at relaxation and even throughout sleep. Thus, for most people, conversion of the clinically silent illness of coronary atherosclerosis to the catastrophic event of myocardial infarction involves a sudden, marked decrease in myocardial blood circulate, with or with out a rise in myocardial oxygen demand. It is now nicely established that coronary artery thrombosis is the occasion that normally precipitates an acute myocardial infarction. Thrombosis typically results from spontaneous rupture of an atherosclerotic plaque, often in a area that contains quite a few inflammatory cells and a skinny fibrous cap. A subendocardial infarct affects the inner one third to one half of the left ventricle. Subendocardial infarction usually happens as a consequence of hypoperfusion of the heart. It may result from atherosclerosis in a specific coronary artery or develop in problems that restrict myocardial blood flow globally, corresponding to aortic stenosis, hemorrhagic shock or hypoperfusion throughout cardiopulmonary bypass. Because necrosis is restricted to the inner layers of the center, issues arising in transmural infarcts A transmural infarct involves the full left ventricular wall thickness and normally follows occlusion of a coronary artery. As a end result, transmural infarcts sometimes conform to the distribution of one of many three major coronary arteries Rather, it first develops within the subendocardium and progresses as a wavefront of necrosis from subendocardium to subepicardium over the course of several hours. Transient coronary occlusion could cause only subendocardial necrosis, whereas persistent occlusion ultimately leads to transmural necrosis. Infarcts contain the left ventricle rather more generally and extensively than they do the proper ventricle. This difference could additionally be partly defined by the larger workload imposed on the left ventricle by systemic vascular resistance and the higher thickness of the left ventricular wall. After 30 to 60 minutes of ischemia, when myocyte damage has turn into irreversible, mitochondria are tremendously swollen, with disorganized cristae and amorphous matrix densities. The nucleus exhibits clumping and margination of chromatin and the sarcolemma is focally disrupted. The noncontractile ischemic myocytes are stretched with every systole and by light microscopy turn out to be "wavy fibers. By 24 hours, the infarct can be recognized on the minimize floor of the concerned ventricle by its pallor. After three to 5 days, the infarcted area turns into mottled and more sharply outlined, with a central pale, yellowish, necrotic area bordered by a hyperemic zone. Within 2 to three weeks, the infarcted region is depressed and delicate, with a refractile, gelatinous look. A cross-section of the heart from a person who died after a protracted history of angina pectoris and several myocardial infarctions shows circumferential scarring of the left ventricle. Left circumflex coronary artery: Obstruction of this vessel is the least widespread cause of myocardial infarction and results in an infarct of the lateral wall of the left ventricle. After a quantity of months, healed infarcts are firm and contracted and have the pale grey appearance of scar tissue. After about 12 to 18 hours, the infarcted myocardium shows eosinophilia (red staining) in sections of the guts stained with hematoxylin and eosin. About 24 hours after the onset of infarction, polymorphonuclear neutrophils infiltrate necrotic myocytes on the periphery of the infarct. The necrotic debris has been largely removed from this space, and a small amount of collagen has been laid down. Muscle cells are more clearly necrotic, nuclei disappear and striations turn out to be less prominent. The means of replacing necrotic muscle with scar tissue is initiated at about 5 days, starting at the periphery of the infarct and gradually extending towards the center. Reperfused infarcts (unlike those demonstrating persistent occlusion) are sometimes hemorrhagic, the results of blood flow via a broken microvasculature. One of probably the most attribute options of reperfused infarcts is contraction band necrosis. Contraction bands are thick, irregular, transverse eosinophilic bands in necrotic myocytes. By electron microscopy, these bands are small teams of hypercontracted and disorganized sarcomeres with thickened Z strains. The bands type because of large infusion of Ca2 into the myocytes as a outcome of sarcolemmal damage mediated by reactive oxygen species. The necrotic myocardial fibers, which are eosinophilic and devoid of cross-striations and nuclei, are immersed in a sea of acute inflammatory cells. The debris is progressively removed, and the scar turns into more solid and less cellular because it matures. In truth, the onset of acute myocardial infarction is usually sudden and related to extreme, crushing substernal or precordial pain. These signs may be accompanied by sweating, nausea, vomiting and shortness of breath. One fourth to one half of all nonfatal myocardial infarctions occur without any symptoms, and infarcts are identified solely later by electrocardiographic changes or at post-mortem. These "clinically silent" infarcts are significantly widespread among diabetic sufferers with autonomic dysfunction and in addition in cardiac transplant patients whose hearts are denervated. Arrhythmias nonetheless account for half of all deaths brought on by ischemic heart illness, although the arrival of coronary care items and defibrillators has significantly reduced early mortality. A section at the fringe of a healed infarct stained for collagen shows dense, acellular areas of collagenous matrix sharply demarcated from the adjoining viable myocardium. During this susceptible period, the infarct consists of soppy, necrotic tissue in which the extracellular matrix has been degraded by proteases released by inflammatory cells but new matrix deposition has not yet occurred. The remaining viable, contractile myocardium adjacent to the infarct produces mechanical forces that may initiate and propagate tearing alongside the lateral border of the infarct the place neutrophils accumulate. The magnitude of the ensuing left-to-right shunt and, due to this fact, the prognosis varies with the size of the rupture. After acute transmural infarction, the affected ventricular wall tends to bulge outward during systole in a single third of patients. Localized thinning and stretching of the ventricular wall within the region of a therapeutic myocardial infarct has been termed "infarct enlargement" but is definitely an early aneurysm. However, the aneurysm continues to dilate with every beat, thereby "stealing" a few of the left ventricular output and increasing the workload of the heart. Thus, the wall of a false aneurysm is composed of pericardium and scar tissue however not left ventricular myocardium. In turn, half of those sufferers have some proof of systemic embolization, the outcomes of which can embrace strokes and visceral infarcts. Pericarditis is manifested clinically as chest pain and should produce a pericardial friction rub. One fourth of sufferers with acute myocardial infarction, notably those with bigger infarcts and congestive coronary heart failure, develop a pericardial effusion, with or with out pericarditis. Postmyocardial infarction syndrome (Dressler syndrome) refers to a delayed type of pericarditis that develops 2 to 10 weeks after infarction. Antibodies to heart muscle appear in these patients, and the situation improves with corticosteroid remedy, suggesting that Dressler syndrome has an immunologic foundation. Restoration of arterial blood flow stays the one way to salvage ischemic myocytes completely, although a quantity of interventions can delay ischemic damage. Percutaneous transluminal coronary angioplasty is dilation of a narrowed coronary artery by inflation with a balloon catheter. Coronary artery bypass grafting can restore blood move to the distal segment of a coronary artery with a proximal occlusion. Procedures that restore blood flow have to be carried out as quickly as potential, ideally in the first few hours after the onset of symptoms. A transverse part of the heart exhibits marked hypertrophy of the left ventricular myocardium with out dilation of the chamber. This scenario often displays a mix of ischemic myocardial dysfunction, diffuse fibrosis and multiple small healed infarcts. In some sufferers, the dysfunctional myocardium has been subjected to repetitive episodes of ischemic damage, which causes degenerative adjustments in myocytes, characterised principally by lack of myofibrils. Diastolic dysfunction is the most common practical abnormality caused by hypertension and by itself can result in congestive coronary heart failure. Some interstitial fibrosis typically develops as part of hypertrophy, which additional contributes to left ventricular stiffness. Hypertension can be related to increased severity of coronary artery atherosclerosis. The combination of elevated cardiac workload (systolic dysfunction), diastolic dysfunction and narrowed coronary arteries leads to a greater risk for myocardial ischemia, infarction and heart failure. Systemic hypertension is considered one of the most prevalent and critical causes of coronary artery and myocardial disease in the United States. Chronic hypertension leads to stress overload and outcomes first in compensatory left ventricular hypertrophy and, eventually, cardiac failure. The time period hypertensive heart illness is used when the center is enlarged in the absence of a cause aside from hypertension. Microscopically, hypertrophic myocardial cells have an elevated diameter, with enlarged, hyperchromatic and rectangular ("boxcar") nuclei. Death can also end result from coronary atherosclerosis and myocardial infarction, dissecting aneurysm of the aorta or ruptured berry aneurysm of the cerebral circulation. Cor Pulmonale Cor pulmonale refers to right ventricular hypertrophy and dilation secondary to pulmonary hypertension. Increased strain in the pulmonary circulation might replicate a dysfunction of the lung parenchyma or, extra not often, a primary illness of the vasculature Acute cor pulmonale is the sudden prevalence of pulmonary hypertension, most commonly on account of sudden, massive pulmonary embolization. At post-mortem, the only cardiac findings are extreme dilation of the right ventricle and generally the best atrium. This frequency displays the prevalence of continual obstructive pulmonary illness normally a result of tobacco smoking.
Generic 3 ml careprost free shipping. Eye Flu क्या होता है और इसका ईलाज कैसे होता हैं (इंग्लिश भाषा मे) (1080p HD).
The crises are predominantly vaso-occlusive in nature and may be triggered by infection medicine used for pink eye cheap 3 ml careprost with amex, or the pregnancy alone symptoms 4 weeks pregnant discount careprost online amex. If this is associated with a parvovirus an infection 2d6 medications purchase careprost with visa, then the disaster can turn out to be aplastic leading to a rapid drop in haemoglobin counterfeit medications 60 minutes order careprost 3 ml on line. Painful vaso-occlusive crises can occur in any organ leading to symptoms dehydration purchase careprost amex infarction and dysfunction symptoms qt prolongation 3 ml careprost with mastercard, nevertheless the lungs are notably susceptible and can progress to a life-threatening chest disaster. Treatment of a sickle disaster in pregnancy is similar as for the nonpregnant feminine; particularly oxygen, fluids, and analgesia with the addition of antibiotics if an infective set off is suspected. It is especially important that pregnant girls with sickle cell disease are on continuous folic acid supplementation because of the high erythrocyte turnover fee. Also, as most adults with sickle cell disease have practical hyposplenism, they should obtain pneumococcal vaccination and twice daily penicillin prophylaxis. In the sickle cell syndromes, no correlation has been shown between the diploma of anaemia and obstetric or perinatal issues. In addition, no benefit has been shown by prophylactic red cell transfusion to keep the haemoglobin at 100�110 g/litre, quite than transfusing when indications arise. In addition to the issues of price and availability, prophylactic transfusion exposes the mom to the hazards of blood transfusion including an infection and notably the chance of alloimmunization of the mom to minor pink blood cell antigens. This can lead to extreme, delayed, and sometimes fatal haemolytic reactions in the mother and haemolytic illness of the fetus and new child. Indications for transfusion in sickle cell disease ladies throughout pregnancy are: anaemia associated with cardiac or respiratory compromise, extreme sickle cell disease-related issues More controversial indications are: rising frequency of painful crises; sickle cell disease-related issues throughout a previous being pregnant; and multiple gestation pregnancy. The increased danger of intrauterine progress restriction is probably due to the decreased oxygen provide from the maternal anaemia and a few placental infarction. For the infant, the primary two years of life are particularly hazardous with an elevated risk of death because of infection and splenic sequestration. Most pregnancies have a profitable end result, but early collaboration between obstetric and haematology groups is strongly really helpful if there are any considerations. Thalassaemias Alpha Thalassaemia There are 4 medical syndromes depending on the number of genes that have been deleted. Hb Barts has a high oxygen affinity, which restricts oxygen supply to the tissues resulting in a hydropic fetus that normally dies in utero or shortly after birth. Pregnancy with an -thalassaemia hydrops fetus is associated with severe hypertension and proteinuria early in pregnancy, together with a high threat of antepartum and post-partum haemorrhage along with different obstetric issues secondary to a large fetus and ponderous placenta. Routine antenatal screening can detect women vulnerable to carrying an affected fetus. Parents should be referred for counselling and offered prenatal diagnosis as termination of the pregnancy may be required to avoid critical obstetric problems. However, with migration, this disorder will turn out to be extra prevalent in Western nations. The fetus can, subsequently, make some -chains, so though most of the haemoglobin will be Hb Barts there shall be some fetal Hb (HbF (22)) production. The neonate seems wholesome at start however soon develops a extreme haemolytic anaemia as HbF ranges fall. In all girls with suspected two gene deletion -thalassaemia, their companion ought to be screened and if needed they should be referred for genetic counselling. The extreme imbalance of globin chain synthesis results in ineffective erythropoiesis and a severe microcytic hypochromic anaemia. The extra unpaired -globin chains mixture to type precipitates that damage red cell membranes, resulting in intravascular haemolysis. Premature destruction of erythroid precursors leads to intramedullary death and ineffective erythropoiesis. Women with transfusion-dependent -thalassaemia major have traditionally been infertile nevertheless with bettering iron chelation the number of successful pregnancies is growing. There are also an rising number of girls with thalassaemia intermedia continuing to pregnancy. Both groups of girls have an elevated incidence of antepartum and post-partum problems with intrauterine progress restriction, recurrent infections, and hypersplenism. They need to proceed with common transfusions all through pregnancy with the incumbent dangers and problems. The defect is often a complete absence of the -globin protein or a reduced synthesis of the -globin Table 14. Diagnosis is usually made within the second and third trimesters, and treatment depends on the severity of the aplasia. Haemolytic anaemia Pregnancy-related autoimmune haemolytic anaemia is a rare dysfunction, however being pregnant can act as a trigger. Secondary causes embrace lymphoproliferative issues, connective tissue problems, and infections. If triggered by being pregnant it normally happens in the third trimester and remits spontaneously following supply. Treatment aims to keep the haemoglobin at an enough stage for placental perfusion and minimal symptomatic anaemia. Corticosteroids and intravenous immunoglobulin are sometimes used however might not all the time be efficient. Disorders of haemostasis in pregnancy Physiology Normal being pregnant is associated with marked adjustments in all aspects of haemostasis the general impact of which is to generate a state of hypercoagulability (Table 14. The purpose for that is clear when one considers that at the time of delivery, placental separation provokes an acute large blood loss in the area of seven-hundred ml/minute, which should be stopped immediately. Three weeks after delivery a lot of the modifications in clotting elements have returned to regular. Thrombocytopenia in pregnancy Thrombocytopenia is a typical finding in being pregnant and may be as a end result of a big selection of causes (Table 14. Gestational thrombocytopenia Gestational thrombocytopenia is seen in roughly 8% of all pregnancies and accounts for greater than 70% of circumstances of thrombocytopenia in being pregnant. The aetiology is unknown but most likely represents increased peripheral destruction. The platelet count is, in general, solely mildly decreased, and in 95% of girls is between 100 and 150 � 109/litre. The main differential prognosis is between gestational thrombocytopenia and immune thrombocytopenic purpura. Immune thrombocytopenic purpura Immune thrombocytopenic purpura has a prevalence of 1�5 circumstances per 10 000 pregnancies. Chronic immune thrombocytopenic purpura, characterised by immunologically mediated platelet destruction, is two to three times more frequent in girls than men. In being pregnant immune thrombocytopenic purpura has implications for each the mom and the fetus. All girls with platelet counts below a hundred � 109/litre must be screened for medical or laboratory evidence of pre-eclampsia, a coagulopathy, or autoimmune illness. Anti-Ro and anti-La antibodies can lead to congenital coronary heart block in roughly 2% of infants born to mothers with such antibodies. Platelet counts of greater than 50 � 109/litre are thought to be safe for regular vaginal supply and for caesarean section however would preclude the utilization of spinal anaesthesia for which the platelet depend ought to be greater than 80 � 109/litre. Therapies geared toward growing the platelet depend throughout being pregnant or previous to supply embrace using oral prednisolone or intravenous immunoglobulin. The mode of delivery for girls with immune thrombocytopenic purpura is dictated by obstetric causes rather than the platelet count. The platelet depend may be low at delivery but reaches a nadir on day three following supply. This may end up in severe fetal and neonatal thrombocytopenia starting early in being pregnant. Women at risk could be examined for the presence of platelet alloantibodies throughout gestation. In neonates with extreme thrombocytopenia, the commonest shows are petechiae, purpura, or cephalohaematoma at delivery, associated with major danger of intracranial haemorrhage (up to 20% of reported cases), which outcomes in death or neurological sequelae. The therapy of affected infants entails the transfusion of appropriate platelets and washed maternal platelets are often used. Antenatal administration is controversial however can embody a mixture of maternal intravenous -globulin administration, intrauterine platelet transfusions, and corticosteroid therapy, whereas monitoring fetal platelet counts intently throughout the pregnancy. The syndrome is a subtype of extreme pre-eclampsia and seems to be secondary to microvascular endothelial damage and intravascular platelet activation. Red blood cells become fragmented as they cross via small blood vessels with endothelial harm and fibrin deposits. The elevated liver enzyme levels in the syndrome are thought to be secondary to obstruction of hepatic blood flow by fibrin deposits within the sinusoids. The thrombocytopenia has been attributed to increased consumption and/or destruction of platelets. Thrombotic thrombocytopenic purpura Thrombotic thrombocytopenic purpura is a life-threatening multisystem disorder characterised by a pentad comprising: � � � � � Microangiopathic haemolytic anaemia Thrombocytopenia Neurological abnormalities Fever Renal dysfunction incompatible blood transfusion. The absence of this cleavage and the presence of extremely large von Willebrand factor multimers within the circulation is believed to result in platelet activation and the generation of platelet microthrombi. Although congenital thrombotic thrombocytopenic purpura often presents in childhood, there are circumstances in which the presentation is in maturity. Steroids may also be helpful in thrombotic thrombocytopenic purpura in addition to plasma trade. Patients also have an elevated danger of venous thromboembolic disease and are therefore maintained on low-dose aspirin. This has been used successfully in some pregnancies, but pregnancy remains a relative contraindication. Disseminated intravascular coagulation Disseminated intravascular coagulation is an acquired syndrome characterized by the intravascular activation of coagulation. Treatment of disseminated intravascular coagulation includes identifying and eradicating the set off and replacing the lacking clotting components with recent frozen plasma, restoring fibrinogen with cryoprecipitate or fibrinogen concentrate, and correcting the thrombocytopenia with platelet transfusions. Counselling must be offered to all potential carriers of haemophilia to talk about prenatal diagnosis and other elements of being pregnant management. Women who may require blood product therapy should be immunized in opposition to hepatitis B. This can be undertaken at seven to nine weeks of being pregnant and if it indicates a male then prenatal prognosis by chorionic villus sampling or amniocentesis can then be carried out to enable identification of an affected male fetus. Direct mutation analysis has now almost completely changed using linkage analysis in both provider detection and prenatal diagnosis. Women who require clotting factor substitute should receive recombinant merchandise. Its operate as an adhesive protein is most essential in conditions of high shear stress. Inherited defects in von Willebrand factor might, therefore, cause bleeding by impairing both platelet adhesion or fibrin clot formation. Von Willebrand illness is the commonest of the inherited issues of coagulation and is assessed into types 1, 2, and 3. Type three is uncommon and represents an entire absence of von Willebrand consider plasma. Type 2 (subclassified into sorts 2A, 2B, 2M, and 2N) represents qualitative defects in von Willebrand factor. In girls with kind 1 von Willebrand disease, the degrees of von Willebrand issue enhance during being pregnant and usually normalize by delivery. In kind 2 von Willebrand illness, while ranges may enhance, this enhance is of a functionally abnormal protein and alternative therapy could also be required at the time of supply. In women with type 1 or 2 von Willebrand illness, von Willebrand factor ranges must be checked at 34�36 weeks. In kind 3, the levels will stay low and replacement remedy with a von Willebrand factor-containing focus might be needed on the time of supply. In ladies with type 1 von Willebrand disease, von Willebrand issue ranges may fall quickly following supply though the rate of fall is unpredictable. In some girls a fast fall in von Willebrand issue ranges might lead to a delayed post-partum haemorrhage and women should be made conscious of this possibility. Rarer clotting issue Deficiencies Inherited deficiencies of the entire clotting factors have been reported and these might result in haemorrhage on the time of supply. Guidelines on the investigation and treatment of those uncommon issues can be found, together with the administration of delivery. Acquired haemophilia A results in a probably extreme bleeding diathesis, typically of sudden onset. Although acquired haemophilia A presents most commonly in older folks with a median age of 70�80 years, it could current in a younger age group and pregnancy is a acknowledged risk issue for the development of this disorder. The clinical options of acquired haemophilia A differ from these of congenital haemophilia in that bruising, soft tissue, muscle bleeding, gastrointestinal and urogenital bleeding are frequent manifestations, whereas haemarthroses are rare. Severe and lifethreatening bleeding is frequent, however no haemostatic treatment is required in 25�33% of circumstances. The mortality related to acquired haemophilia A has been reported to be between 7. Elimination of the inhibitor should be tried utilizing immunosuppression, which is initiated as quickly because the diagnosis has been established. Relapse of pregnancy-related acquired haemophilia seems to be relatively uncommon, but might occur and girls must be warned of this possibility. Miscellaneous haematological situations Autoimmune neutropenia this can be a rare dysfunction, most circumstances of which are delicate. It can be major or secondary (in affiliation with autoimmune issues, systemic lupus erythematosus, or rheumatoid arthritis, viral infections, drugs). Symptomatic neutropenia (recurrent infections) occurs at neutrophil counts of under 0. There are concerns that it might be related to elevated preterm birth and a small enhance in the incidence of venous thromboembolism, but there are case stories of its secure use in being pregnant. Myeloproliferative diseases Thrombosis and haemorrhage are the main reason for morbidity in pregnant sufferers with important thrombocythemia and polycythemia vera. There are limited information, but these situations are troublesome to manage during being pregnant and are associated with a excessive fetal mortality.
It is due to symptoms 8 dpo best 3ml careprost circulating antibodies in opposition to adhesion molecules of the pores and skin basement membrane zone crohns medications 6mp order careprost overnight. The pathogenicity of the circulating basement membrane zone antibodies is demonstrated by transplacental transmission of the disease treatment centers in mn best careprost 3 ml. Both antigens are present in skin symptoms 4dpiui cheap 3ml careprost with visa, mucosa symptoms 0f yeast infectiion in women cheap 3ml careprost with amex, and amnion symptoms gallstones purchase careprost amex, related to the hemidesmosome and adhesion advanced linking epithelium to dermis/mesenchyme, that are targets in other autoimmune blistering illnesses. It commences from the second trimester onwards and very often in the first week post-partum (range from 5 weeks of gestation to four weeks post-partum). It usually occurs in the first and subsequent pregnancies, although 8% of pregnancies are skipped. The eruption typically begins around the umbilicus and spreads to the entire trunk, limbs, arms, and toes, including the palms and soles, and infrequently the face. Vesicles and blisters are characteristic, however lesions comprise annular lesions, papules, and plaques. Transplacental transmission of antibodies to the fetus happens in about 3% of affected pregnancies, the neonate growing transient self-limiting blistering. Histopathology demonstrates an eosinophilic infiltrate, papillary oedema, and subepidermal blisters. Direct immunofluorescence demonstrates that C3 part of complement and IgG1 are bound at the basement membrane zone of the dermoepidermal junction. Treatment with potent or very potent topical steroids and chlorpheniramine is really helpful, nonetheless, systemic steroids The classical instructing is that it recurs earlier and is more severe in subsequent pregnancies, however this has not at all times been our experience. Onset of pemphigoid gestationis in the first or second trimester and presence of blisters might result in adverse pregnancy outcomes, including decreased gestational age at supply Such pregnancies ought to be thought of high risk and acceptable obstetric care ought to be provided. Classical dermatoses affecting pregnant girls Psoriasis Psoriasis improves in most ladies during pregnancy, but can deteriorate. Methotrexate is a folic acid antagonist and might trigger miscarriage; acitretin is teratogenic; fumaric acid causes leukopenia (whether this impacts the fetus is unknown, however case reports have proven no harm). A extreme type of pustular psoriasis, impetigo herpetiformis, could happen in being pregnant and is finest managed with bed rest, emollients, and reasonable potent topical steroids or low doses of oral prednisolone. Cutaneous lupus erythematosus could additionally be adversely affected or improved or unchanged by pregnancy. However, such sufferers ought to be screened for anti-Ro and anticardiolipin antibodies, ideally previous to conception, to establish at-risk pregnancies (see Chapter 14. Pemphigus vulgaris is an autoimmune blistering illness with widespread mucosal and/or cutaneous erosions brought on by IgG antibodies to desmosomal elements of the epithelium. The desmosomal antibodies are directed at desmoglein 3, a significant adhesion molecule in mucosa and neonatal skin, and may be transmitted throughout the placenta, inflicting extreme neonatal pemphigus with devastating results to the fetus. Both types of pemphigus may worsen in being pregnant and remedy may require systemic steroids and immunosuppressants like azathioprine. Pemphigoid gestationis: early onset and blister formation are associated with opposed being pregnant outcomes. A potential research of 200 ladies with dermatoses of being pregnant correlating medical findings with hormonal and immunopathological profiles. Ursodeoxycholic acid and S-adenosylmethionine for the treatment of intrahepatic cholestasis of pregnancy: a meta-analysis. Vulval dermatoses Many dermatoses may have an effect on the vulval skin, and this can be particularly distressing in being pregnant as concerns relating to supply could come up. A illness generally seen on the vulva is lichen sclerosus, a continual inflammatory situation of unknown trigger. They may remit or improve throughout being pregnant, but can flare or present in being pregnant or publish partum. Antiphospholipid syndrome Clinical features-antiphospholipid antibodies include anticardiolipin antibodies (IgG and/or IgM), lupus anticoagulant, and anti2-glycoprotein-I antibody. Antiphospholipid syndrome is the combination of any of those with one or both of the following medical options: (1) thrombosis-arterial, venous, or small vessel; (2) particular being pregnant morbidity. Women with isolated but persistent antiphospholipid antibodies without clinical options of antiphospholipid syndrome have obstetric outcomes much like the general inhabitants. This requires low-dose aspirin from early pregnancy for prevention of pre-eclampsia � low-molecularweight heparin. Systemic lupus erythematosus the mother-pregnancy probably exacerbates systemic lupus erythematosus and will increase the likelihood of a flare, which can be tough to diagnose since many medical options also happen in normal pregnancy. Differentiation of active renal lupus from pre-eclampsia is notoriously tough: renal flares are extra widespread if disease is active within six months of conception, particularly in ladies with hypertension, heavy proteinuria, or high baseline serum creatinine. The fetus- systemic lupus erythematosus is associated with increased risks of opposed pregnancy consequence together with fetal demise and intrauterine progress restriction. Most fetal losses occur in affiliation with secondary antiphospholipid syndrome or active illness, notably renal. For girls with systemic lupus erythematosus in remission and without hypertension, renal involvement, or the antiphospholipid syndrome, the danger of issues in pregnancy is similar to that of the final population. Management-flares of systemic lupus erythematosus have to be actively managed, pre-pregnancy counselling should be encouraged with therapy relying on each organ involvement and severity. Mild circumstances could be managed with analgesics alone (paracetamol); rash and arthritis will often respond to nonsteroidal anti-inflammatory medicine, low-dose prednisolone and/or hydroxycholorquine; more severe illness might require introduction of a disease-modifying agent Steroids stay first-line therapy for extreme lupus flares in being pregnant (and treatment of different autoimmune conditions). The baby-neonatal lupus syndromes are caused by transplacental passage of autoantibodies directed against cytoplasmic ribonucleoproteins Ro and La. Cutaneous neonatal lupus is the commonest manifestation (5%) and congenital coronary heart block essentially the most severe (20% mortality). Methotrexate is teratogenic, but with the advent of remedy with biologics, extra ladies with rheumatoid arthritis at the moment are attempting being pregnant. Overall the danger of antagonistic obstetric outcomes remains minimal and much like the conventional inhabitants. Introduction Autoimmune diseases affect 5�7% of the population and are extra frequent in ladies of childbearing age. Many girls with autoimmune rheumatic ailments have been suggested towards pregnancy in the past, but that is now not applicable with a new era of pregnancy-friendly disease-modifying antirheumatic medication and biological brokers that afford glorious disease management with out compromising fertility. Nevertheless, many women with autoimmune rheumatic diseases are older and have extra comorbidities. Pregnancy is associated with suppressed cell-mediated immunity (Th1) and enhanced humoral immunity (Th2), but these changes revert post-partum accompanied by rapid reductions of oestrogen, progesterone, and cortisol ranges. The post-partum interval is subsequently a time of susceptibility to autoimmune disorders; and ladies who already have an autoimmune dysfunction could undergo illness exacerbation following pregnancy. Flares in pregnancy are often accompanied by antagonistic obstetric outcomes for both mom and fetus. This chapter considers the connection between pregnancy and systemic lupus erythematosus, antiphospholipid syndrome, rheumatoid arthritis, vasculitides, and scleroderma, and the way being pregnant affects treatment of these conditions. Systemic lupus erythematosus Systemic lupus erythematosus is rather more frequent in women than males (ratio 9:1), with peak onset in the course of the childbearing years. A recent intensive evaluation of published epidemiological studies demonstrated that the prevalence ranges from 0. Women with systemic lupus erythematosus and secondary antiphospholipid syndrome have an elevated danger of maternal thrombosis, especially within the puerperium. There should be a low threshold for empiric therapy with low-molecular weight heparin pending appropriate diagnostic imaging. Young girls with systemic lupus erythematosus are also at risk of untimely atherosclerosis, even within the relative paucity of cardiovascular risk components. It is possible the pregnancy and its associated issues accelerate this process. Hence, myocardial infarction ought to be thought of as a differential if she presents with chest pain or shortness of breath. Idiopathic pulmonary hypertension is associated with an as a lot as 25% risk of maternal mortality, and this danger is even higher in ladies with underlying connective tissue disorders. Nevertheless, the most typical explanation for maternal death in women with systemic lupus erythematosus is infection. Effect of systemic lupus erythematosus on being pregnant Women with systemic lupus erythematosus remain fertile, besides throughout severe flares or after publicity to prolonged excessive doses of cyclophosphamide, which leads to untimely ovarian failure. However, systemic lupus erythematosus is associated with increased threat of early being pregnant losses and the later adverse pregnancy outcome on account of placental insufficiency, and manifest as pre-eclampsia, fetal growth restriction, or small for gestational age infants, placental abruption, and stillbirth-collectively often recognized as maternal-placental syndrome. The primary components influencing being pregnant outcomes in girls with systemic lupus erythematosus are disease exercise (especially at time of conception), hypertension, renal involvement, secondary antiphospholipid syndrome, and anti-Ro/La antibodies (see next). Presence of renal disease is closely associated with being pregnant outcomes in ladies with systemic lupus erythematosus. In a metaanalysis energetic nephritis at conception was associated with 25�50% price of fetal loss as in comparison with 8�12% if the illness was inactive. Active systemic lupus erythematosus within the four to six months previous conception will increase the chance of a flare during being pregnant. Several case�control studies have addressed this concern, but differ in patient ethnicity, standards for flare and systemic lupus erythematosus exercise scales employed. Hydroxychloroquine has been linked with higher disease control and improved obstetric outcomes, and therefore ought to be continued in pregnancy. Ideally, being pregnant must be deliberate when systemic lupus erythematosus is in remission, whereas on drugs that are suitable to be continued in being pregnant. Renal flares are extra frequent if illness is lively within six months of conception. There is a danger of deterioration of renal perform in being pregnant, particularly if the sufferers are hypertensive, have pre-existing heavy proteinuria, or a high baseline serum creatinine. A recent meta-analysis reported that the incidence of renal lupus flares during pregnancy was 11�69% and renal impairment occurred in 3�27%, which was irreversible in up to 10%. Baseline renal perform, blood strain, and the antiphospholipid and anti-Ro/La antibody status enable prediction of the risks to the lady and her child (see later). A choice ought to be made as to whether or not to begin aspirin and/or low-molecular weight heparin if the lady is susceptible to thromboses. Her drugs must be reviewed and altered to pregnancy-friendly drugs (if possible). It is important to guarantee clinical stability on this regime for at least six months preconception. Maternal surveillance Pregnancy care is finest undertaken in multidisciplinary, mixed clinics the place physicians and obstetricians can monitor illness activity, fetal development, and uterine and umbilical artery Doppler blood move. Women might need to be frequently reviewed for any indicators of preeclampsia or a flare. As a rule of thumb, the visits improve in frequency in direction of and during the third trimester-when superimposed pre-eclampsia is commonest. Diagnosis of flare Differentiation of energetic renal lupus from pre-eclampsia is notoriously difficult, and the two situations might co-exist. The gold normal is a renal biopsy to differentiate a renal lupus flare from pre-eclampsia. Delivery is seldom the solely real administration of choice as post-partum flares are widespread and extreme. Teratogenic brokers corresponding to cyclophosphamide should be avoided in the first 12 weeks during which organogenesis occurs. There are long-term safety information on the use of cyclophosphamide later in pregnancy with a cohort of youngsters uncovered in utero exhibiting no indicators of neurodevelopmental delay or different adverse results when followed as a lot as adolescence. Conversely, fluorinated steroids like dexamethasone and betamethasone cross the placenta more readily and are sometimes used for antenatal fetal lung maturation in ladies at danger of preterm supply. Corticosteroid usage in being pregnant does enhance the maternal threat of gestational diabetes, hypertension, an infection, danger of preterm rupture of membranes and osteoporosis. Prednisolone is safe in breastfeeding moms since less than 10% of energetic drug is secreted into breast milk. Notwithstanding the above risks, steroids stay first-line therapy for severe lupus flares in being pregnant (and remedy of different autoimmune conditions), as the benefits of fast illness control outweigh the risks. Neonatal lupus syndromes About 30% of sufferers with systemic lupus erythematosus are antiRo positive. In such ladies the risk of transient cutaneous lupus is about 5% and the danger of congenital heart block about 2%, with the two circumstances not often coexisting. Anti-Ro antibodies are current in 90 to 100% of moms of affected offspring, and sixty eight to 91% have anti-La antibodies. Maternal titres of anti-Ro antibodies as excessive as 50 U/ml or extra usually have a tendency to be related to congenital coronary heart block. The threat of neonatal lupus is increased if a previous child has been affected, at 15�25% if one and 50% if two previous kids are affected. Residual hypopigmentation or telangiectasia may persist for as much as two years, however scarring is unusual. Congenital heart block often appears in utero, around 18� 20 weeks and is related to a structurally normal coronary heart. The mechanism of injury appears to contain binding of the anti-Ro/La antibodies to antigens on the fetal cardiocytes, inducing an inflammatory process which leads to tissue injury and fibrosis of the conducting system. Complete coronary heart block causes bradycardia which may be detected on auscultation, but lesser degrees of coronary heart block require Doppler echocardiography. Overall mortality is round 20%, with deaths normally occurring in utero (after growing hydrops, pleural and pericardial effusions) or the neonatal period, however can occur up to three years of age. Most infants who survive the neonatal interval do well, though two-thirds require pacemakers. In the past, intravenous immunoglobulins, fluorinated glucocorticosteroids, plasmapheresis, salbutamol, and digoxin have all been tried and located to be ineffective. Studies on congenital coronary heart block have been troublesome to conduct due to the rarity of the condition. However, a big retrospective research did find an affiliation between maternal hydroxychloroquine use, and a reduction in heart block within the offspring. Its follow-on examine specializing in subsequent pregnancies of girls whose offspring were affected discovered that there was a particular discount within the incidence of heart block in the offspring of the ladies who have been receiving hydroxychloroquine.