Gholam K. Motamedi, M.D.
- Department of Neurology
- Baylor College of Medicine
- Houston, TX
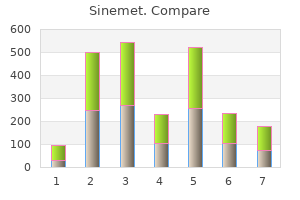
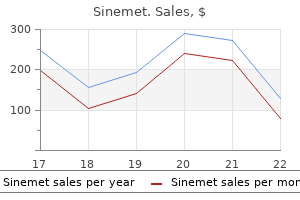
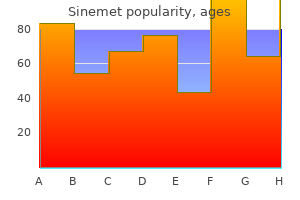
A malleable retractor is placed medially after the delicate tissues have been emancipated with a Cobb or comparable elevator medicine you can take while pregnant sinemet 110 mg cheap. The femoral osteotomy is slightly below the lesion medicine etodolac buy 110 mg sinemet with mastercard, to present disease-free bone stock for fixation of the proximal femur alternative treatment 6th february discount sinemet 125 mg without prescription. The size of the modular bodies available per the manufacturer is taken into account treatment management system purchase discount sinemet online. The modular prosthesis in situ treatment atrial fibrillation sinemet 125 mg visa, similar to treatment gonorrhea purchase sinemet overnight the length of the resected specimen. I prefer to use a gentle tissue washer drilled via any residual larger trochanter that could be available. Careful preoperative planning and familiarity with the incremental reconstruction ranges of the selected implant are important to facilitate efficient reconstruction. If no acetabular reconstruction is deliberate, a trial head is examined for dimension as ordinary. Although a big stem diameter is preferable, overzealous reaming on this affected person population is discouraged. Continual lavage and irrigation of the medullary contents is of critical importance. A cement mantle of no much less than 1 mm is most popular; due to this fact, the stem diameter must be at least 2 mm smaller than the final reamed measurement for ease of introduction at cementation and keep away from monomer introduction into the circulatory system. Taper and face-reaming of the proximal femur as described by the implant manufacturer could additionally be necessary. After discount of the trial, the capsule is pulled tight by stay sutures, and stability and size are assessed. Orientation of the prosthesis is essential, with anteversion based on the sagittal plane created by the linea aspera. A lengthy laparoscopic-type suction device ought to be used continually throughout instrumentation of the femoral canal, and consideration must be given to venting if a long stem is to be deployed. As the cement matures after prosthetic deployment, the surgeon should instantly and punctiliously verify the chosen version. Soft tissue reconstruction is of paramount importance for a sound functional end result. Numerous strategies have been described for reattaching the abductor mechanism to the implant. The surgeon should pay shut consideration to the reattachment mechanism, as a end result of that is the restrict of the useful reconstruction. The vastus lateralis muscle is repaired, as are the gluteus maximus and iliotibial band. Intraoperatively, the surgeon must carefully determine the suitable version, which is about ninety five to one hundred degrees off the midsagittal plane as determined by the linea aspera. I choose to use two smaller-diameter soft tissue washers to screw down the mechanism. The larger-bore bolts which are out there are inclined to destroy any residual greater trochanter in this compromised affected person population. If a drain has been positioned for metastatic circumstances, it ought to be discontinued inside seventy two hours. Depending on the method and the extent of the dissection, hip precautions must be carried out for six to 12 weeks. Proximal femoral replacement is related to complication charges as excessive as 28%. No better alternatives with lower risks than proximal femoral replacement exist for this tough patient inhabitants. Cemented total or hemiarthroplasty for femoral head, neck, and peritrochanteric lesions stays, generally, the process of selection on this affected person population, with good to wonderful outcomes relative to the omnipresent comorbidities. Fat embolization and deadly cardiac arrest throughout hip arthroplasty with methylmethacrylate. Prosthetic hip replacement for pathologic or impending pathologic fractures in myeloma. Comparison of fixation of the femoral part with out cement and fixation with use of a bonevacuum cementing method for the prevention of fats embolism during complete hip arthroplasty. Complications of cemented long-stem hip arthroplasties in metastatic bone illness. Perioperative cardiopulmonary complications related to cementing hip arthroplasty components are nicely described. In addition to cementation, this contains porous bone and the usage of long-stem femoral implants. Long-stem elements have been proposed to increase pressurization of the canal, producing extra embolic events, with the speed of cardiopulmonary issues reported to be as high as 62%. The pelvic landmarks that assist in component removal and positioning include the ischium, pubis, anterior and posterior acetabular columns, anterior inferior iliac spines, transverse acetabular ligament, sciatic notch, and acetabular partitions. Neurologic constructions at risk embrace the sciatic nerve, which could be identified in three distinct anatomic areas: As it exits the sciatic notch Lying over the ischium posterior and inferior to the posterior acetabular column Beneath the femoral insertion of the gluteus maximus tendon insertion into the posterior femur. The superior gluteal nerve is in danger throughout part elimination because it travels anteriorly along the ilium, approximately four to 5 cm superior to the tip of the larger trochanter, to innervate the gluteus medius muscle. The femoral nerve is nicely anterior to the hip for most approaches however could also be at risk with additional anterior dissection and retraction and with anterior supine approaches to the hip. The femoral artery and vein are properly anterior to the dissection and usually are protected by the iliopsoas tendon and muscle stomach. The proximal femoral anatomy includes the higher and lesser trochanter and the vastus ridge, which is a degree of relatively weak bone in most revisions because of osteolysis, previous trochanteric osteotomies, or previous surgical procedure in this area. The femoral diaphyseal anatomy consists of the attachments of the vastus musculature on the vastus ridge and posteriorly at the linea aspera. Both are indications for trochanteric osteotomy to facilitate exposure of the acetabulum and possible stem elimination. Component elimination with attention to bone preservation for subsequent reconstruction is crucial. Judet indirect radiographs demonstrating anterior column deficiency and acetabular loosening with a well-fixed stem. Biplanar radiographs of the complete implant and the joint above and under the prosthesis are essential. These findings are helpful in guiding plans for bone grafting of lytic lesions and figuring out remaining bone stock. Plain radiographs normally tremendously underestimate the extent of osteolysis involvement within the pelvis from polyethylene particles. Bone scan examination may reveal subtle implant loosening that will not be appreciated on plain radiographs or on the time of surgery and may help the surgeon resolve whether or not to retain or remove implants that appear well mounted. Care must be taken to protect as much bone stock as potential during the removal for subsequent reconstruction. These osteotomes are designed so that the rotation point is within the middle of the acetabular element. Positioning In general, patients can be positioned supine or in the lateral decubitus position. In the anterior supine method, the patient is positioned within the supine position and an anterior strategy to the hip is carried out in the interval between the tensor fascia lata and the sartorius muscles. An anterior or anterolateral method to the hip can be performed in the supine or lateral position and is extensile in each the proximal and distal directions ought to extra publicity be required. An axillary roll is used to provide protection for the brachial plexus during surgery. This approach retains much of the posterior capsule and buildings, which doubtless reduces the incidence of dislocation after revision. Lateral A direct lateral method to the hip involves a break up within the anterior third of the gluteus medius and minimus musculature. Acetabular exposure with retractors in place earlier than femoral head dislocation on this hip, which shows severe polyethylene wear and osteolysis. New polyethylene liner is inserted with the femoral head in view and retracted posteriorly. The vastus lateralis stays hooked up to the lateral portion of the osteotomy but is reflected anteriorly to permit visualization of the lateral and posterior femoral cortex. An oscillating noticed is used to carry out the posterior portion of the osteotomy just superior to the linea aspera. The distal extent of the osteotomy is beveled within the distal and anteroposterior direction. The anterior portion of the osteotomy is made with a small (1/4-inch) osteotome perforated through the vastus musculature. The capsule surrounding the prosthesis under the greater trochanter is released or excised and the "shoulder" of the prosthesis uncovered. About one third of the lateral portion of the femoral circumference is a half of the osteotomy. The vastus lateralis that continues to be attached to the lateral portion of the osteotomy is reflected anteriorly to enable visualization of the lateral and posterior femoral cortex. The anterior portion of the osteotomy is made with a 1/4-inch osteotome perforated by way of the vastus musculature. The whole prolonged trochanteric fragment is mirrored anteriorly, with care to not fracture the tip of the trochanteric fragment, which is the weakest point within the osteotomized fragment. Bennett and Charnley retractors retract soft tissue and the trochanteric fragment to visualize the femoral prosthesis. The cement�implant and cement�bone interfaces or the ingrowth interface is now accessible. The trial implants are inserted and a trial discount performed before the trochanteric fragment is reattached. Anterior and medial capsular attachments are taken right down to the level of the psoas tendon. All tissue lateral to the psoas tendon may be removed at this level if wanted to allow visualization of the stem. Osteotomes, ultrasonic gadgets, or high-speed burrs now have entry to the cement�implant and cement�bone interfaces or the ingrowth interface, as wanted for removal. The femoral preparation for long-stem implant insertion is completed with versatile reamers and proximal femoral tapered reamers. The trial implants are inserted and a trial reduction performed with the trochanteric fragment not hooked up. It is necessary not to gouge the acetabulum or to break off large pieces by aggressively twisting or pulling a well-secured cup. Acetabular osteotome techniques facilitate cup elimination by utilizing the middle of the acetabular polyethylene as a reference for osteotome insertion. The osteotome blade is inserted and turned in a agency, controlled method, sustaining its orientation to the rim of the cup. First, a small osteotome is inserted that matches the radius of the acetabular element. The acetabular osteotome used to take away cups allows skinny osteotome insertion exactly in the bone implant interface. A small osteotome is first used to enter the bone�implant interface around the rim of the acetabular element. Using the acetabular explant chisel on a handle, the implant is eliminated with minimal bone loss. Extended trochanteric osteotomy Bevel the distal transverse arm of the osteotomy to stop distal fracture propagation. Pass a cerclage wire distal to the osteotomy before femoral preparation and trial and ultimate implant insertion. Pay careful attention to trochanteric osteolysis and fracture threat on the vastus ridge at the junction of the vastus lateralis and the abductor attachment into the trochanter. Have enough bone graft available, including morselized cancellous graft and cortical struts for contained and uncontained defects. Leave vastus muscle attached to the trochanteric fragment to provide sufficient blood provide for osseous healing and implant stability. The polyethylene should be faraway from the acetabular element to allow screw removing, then changed for a information or reference for removing devices. With polyethylene exchanges and part retention of osseointegrated implants, weight bearing as tolerated is beneficial. When an implant is eliminated and an antibiotic-impregnated static spacer is inserted, foot-flat (essentially non�weight bearing) weight bearing is beneficial. The fate of secure cemented acetabular parts retained during revision of a femoral part of a complete hip arthroplasty. The fate of secure femoral components retained during isolated acetabular revision: a six-to-twelveyear follow-up study. Acetabular deficiencies may be intensive in the face of polyethylene put on and osteolysis. The proximal facet of the femur consists of the pinnacle, the neck, and the higher and lesser trochanters. Vascular and neurologic buildings embrace the femoral artery and vein and the sciatic nerve. The presence of this debris will increase over time, resulting in a macrophage response that leads to periprosthetic bone loss. Aseptic loosening could occur secondary to this particle-induced periprosthetic osteolysis. Other systemic medical situations and up to date surgical or medical remedies should also be documented to be sure that the affected person can tolerate and will benefit from hip revision.
A single skin incision could also be used with subperiosteal publicity of the cranial and caudal basis websites medicine university cheap sinemet 125 mg with visa. The lateral view exhibits the straight tandem connector positioned in the thoracolumbar region medicine wheel buy generic sinemet 300 mg. The trajectory of the pedicle screws can be seen and varies between patients treatment pancreatitis purchase sinemet line. Close-up of the cranial basis reveals four pedicle screws spanning two ranges within the thoracic area medications starting with p discount sinemet 300 mg fast delivery. Close-up of the caudal foundation exhibits 4 pedicle screws spanning two ranges in the lumbar spine medicine klonopin cheap sinemet 110 mg. Growing rod technique for the remedy of progressive early onset scoliosis in fusionless surgery for spine deformity medicine you can overdose on order 300mg sinemet with visa. These transverse connectors improve the soundness of the construct, especially when hooks have been used. The cranial anchors and transverse connector are tightened first, followed by the caudal anchors and transverse connectors. Cranial and caudal set screws are located on the facet of the tandem connector that correlates to essentially the most prominent facet. Next, the rod construct on the convex aspect of the curve is created equally and tightened. The surgical area is then irrigated, followed by a limited arthrodesis making use of autograft bone or different graft extenders between the vertebrae making up every foundation. Dual-Incision Technique the dual-incision approach differs from the single-incision technique in a couple of ways. The subperiosteal dissection is identical, as are placement methods of both hooks or pedicle screws for anchors. In placing the rods, however, subcutaneous or subfascial dissection must be performed rigorously and bluntly with either a finger or blunt clamp to facilitate rod passage. Careless dissection or poor management of the rod throughout passage can result in pleural violation. Lengthening and Exchange Lengthening of the dual rod assemble could additionally be carried out as either an in- or outpatient process with neural monitoring for sufferers with regular neurologic perform. The connector is located by way of palpation or fluoroscopy, and a small incision is remodeled that space the place the lengthening is planned. Lengthening may be performed by inserting the distractor between the rods through the slot of the tandem connector. Alternatively, a rod clamp can be placed on the rod a couple of centimeters from the connector and the distractor positioned between the rod clamp and the end of the connector. The set screw nearest the rod clamp is then loosened, the distractor employed, and the screw retightened. Lateral radiograph after the dual growing rod process was carried out on the same affected person. Once further distraction is not achievable, last correction and arthrodesis are performed. Changing the Connector or Rod Exchange of the tandem connector or the rod may be wanted if the quantity of lengthening exceeds the initial size of the tandem connector. In such a case, each set screws must be loosened and the tandem connector slid cephalad until full clearance of the caudal rod is achieved. The connector can then be removed off the cranial rod, replaced by an extended connector, and slid onto the caudal rod again. This entails exposing and eradicating the tandem connectors, exposing the foundation, and removing the rods and changing them with longer rods, making a assemble similar to the preliminary process. Final fusion is performed near the top of the adolescent progress spurt or when the rods can no longer be lengthened. The first step entails removing the twin growing rod implants, together with the anchors and exploring foundations for solid fusions. For most sufferers, the fusion ought to lengthen from the cranial foundation to the cephalad foundation. Rods are then contoured to the specified form, keeping in mind that the aim is to achieve global balance rather than a completely straight spinal phase. Thus, higher and decrease curves should be thought of collectively when contouring the rods. A consideration when performing the ultimate fusion is that posterior osteotomies may be required, particularly if a subfascial method is employed, as a end result of the posterior parts could turn into stiff after repeated exposures. This usually can be carried out safely by finding the neural canal after which osteotomizing the pars on either aspect. Another consideration is that the areas around the anchor sites typically are overgrown with bone, and taking the implants out often entails osteotomizing the bone around the anchors. Although pedicle screws offer three-column help in the foundations, changing hooks in the fusion mass provides sufficient strength if placed correctly, and hooks are simpler to place, particularly in the event that they had been used initially for the growing rods. Sublaminar wires additionally supply a gorgeous option and are helpful if lateral translation of the backbone is required. Tandem connectors are straight and must be placed at the thoracolumbar area, which also is straight. Lengthening Indications Do not be too aggressive with lengthenings, especially at the index procedure and first lengthening, to keep away from implant points. May not be indicated in very stiff curves, poor bone quality, older youngsters with restricted development potential, or kids too young to permit internal fixation. Patients with more frequent lengthenings have fewer implant issues but more wound problems, whereas sufferers with less frequent lengthenings have extra implant problems and fewer wound problems. Implant complications usually may be treated during scheduled lengthenings, but wound infections must be handled urgently. One study confirmed Cobb angle correction from a mean of eighty two levels to 36 degrees eventually go to or ultimate fusion. Instrumentation with restricted arthrodesis for the remedy of progressive early-onset scoliosis. Dual rising rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. The rib-vertebra angle in the early prognosis between resolving and progressive childish scoliosis. Comparison of single and dual rising rod methods followed by way of definitive surgical procedure: a preliminary study. It is characterised by the formation of half of a vertebral body, a corresponding pedicle, and a corresponding hemilamina. Full-segmented hemivertebra have a much greater rate of development, as a outcome of the presence of an intact disc area above and below signifies the presence of development plates and potential asymmetrical spinal progress. In the presence of healthy growth plates above and below (ie, a fully segmented hemivertebra) convex development is quicker than contralateral concave growth, causing a progressive scoliosis. In cases of hemivertebra, if the vertebral physique lies within the posterolateral quadrant, a progressive kyphosis could arise with the scoliosis. The disordered progress ultimately may cause curvature to such a degree that usually segmented areas of the spine become concerned in the curve, inflicting deformity and spinal imbalance. Hemivertebrae that are fully segmented progress at roughly 2 levels a year and can exceed over 45 degrees at maturity. Partially segmented hemivertebrae have much much less progress potential (less than 1 degree per year), not often exceeding 40 levels at maturity. Hemivertebra on the lumbosacral junction virtually at all times require therapy, as a outcome of the lumbar backbone takes off obliquely from the sacrum, inflicting a long compensatory curve in normally segmented areas of the lumbar backbone, with resultant beauty deformity and spinal imbalance. Anatomically, it may be joined to the extent above or under at either the physique, the hemilamina, or each. A native kyphotic or lordotic deformity could occur with hemivertebra if the associated failure of formation is greater anteriorly or posteriorly. A full musculoskeletal examination on the lookout for diagnoses corresponding to clubfoot, developmental dysplasia of the hip, and limb anomalies is warranted. A full neurologic examination ought to be carried out, because as many as 40% of sufferers with congenital scoliosis have a corresponding spinal dysraphism. Occult signs of spinal dysraphism embrace cutaneous manifestations such as midline spinal hemangiomas, penetrating sacral dimples, or midline hairy patches. Foot anomalies such as vertical talus or uneven cavus ft can signify spinal dysraphism. Cardiac auscultation ought to be accomplished, because 20% of patients with congenital scoliosis have congenital heart anomalies. Rotation of the backbone in the course of the Adams ahead bend take a look at is indicative of deformity and points to its location. Bending radiographs, during which the affected person is directed to bend in a concave and then in a convex path, are essential to assess the pliability of curves above and below the hemivertebra. We have discovered that excision is best carried out between the ages of 18 months and four years. Patients youthful than this can be more difficult to instrument, and waiting till this age hardly ever has brought on irrevocable deformity. If the affected person requires neurosurgical intervention for dysraphism, that procedure ought to precede the hemivertebra excision, both at the same setting or in a staged setting, at the discretion of the spine surgeon and neurosurgeon. Studying the pedicle anatomy (ie, length and diameter) of the levels above and beneath is efficacious given the smaller size of those sufferers. Neurologic monitoring is essential and must be accomplished using somatosensory evoked potentials and motor evoked potentials. Communication between the monitoring and anesthesia groups must be facilitated to prevent any change in neurologic perform introduced on by anesthetics, hypotension, or low blood quantity. Hemivertebra associated with little or no curve progression (unsegmented or partially segmented) could also be adopted throughout Positioning We perform hemivertebra excisions with the affected person in the inclined place. This is done on a radiolucent working frame with chest and pelvic assist, which leaves the abdomen free. We even have discovered it useful to barely "airplane" the desk or bolster the affected person in order that the convex facet is slightly greater than the concave facet. Before draping the patient, we place a marker over the hemivertebra region and procure a radiograph. This each confirms the side of the hemivertebra and helps restrict excessive incisions and dissections. In the past we beneficial that hemivertebra excision be carried out as a simultaneous anterior-posterior procedure. The anterior approach is on the convex facet and ought to be marked earlier than the patient goes to the working room. We still suggest considering an anterior�posterior procedure when medical circumstances (eg, congenital coronary heart disease) warning in opposition to extreme bleeding, when a lordotic element renders access to the vertebral physique tough, and when the surgeon is unfamiliar with posterior-only approaches to circumferential surgery. Approach If an anterior�posterior process is being performed, the anterior procedure must be a normal transthoracic, transthoracic-retroperitoneal, or retroperitoneal method, depending on the situation of the hemivertebra. The anterior method often can be a limited one, as a result of the one exposure needed is of the hemivertebra and the discs above and below. The posterior strategy is a standard posterior midline incision with subperiosteal dissection out to the ideas of the transverse processes. Once fully dissected, a spot radiograph or fluoroscopic view should be obtained to confirm the appropriate degree. Screws must be positioned in a stepwise manner, starting with obtaining a cancellous blush with a burr at the acceptable starting place. A pedicle awl can then be used to acquire access down the pedicle into the vertebral body. Once the pedicle has been accessed, probing of the 4 partitions of the pedicle and floor of the physique is necessary to affirm accurate position. This step aids in protection of constructions lateral and anterior to the wall on the hemivertebra. If the hemivertebra is within the thoracic region, will most likely be necessary to resect the rib head first to get hold of access. The cartilaginous surfaces of the concave side should be resected to encourage fusion. Resection ought to extend over to the aspect, while the exiting nerve roots above and below the hemivertebra are identified and guarded. Care should be taken to avoid nerve roots, which are present rostral and caudal to the pedicle walls of the hemivertebra. The subperiosteal airplane down the lateral wall of the pedicle and body is then developed, with a Cobb elevator used to facilitate retraction and protection. Bipolar sealing of epidural vessels that lie on the medial side of the pedicle and down on the inner wall of the physique will help in controlling blood loss and enhancing visualization. Continued resection down the pedicle and into the hemivertebra physique may be done by a diamond-tipped burr, which helps defend towards unwanted injury to gentle tissue constructions. The walls of the pedicle can then be easily resected with a curette or pituitary rongeur, as can the remaining walls of the body of the hemivertebra. Protection lateral and anterior to the confines of the hemivertebra wall is critical to avoid damage to important constructions such because the aorta. This resection is a wedge resection, which incorporates the discs above and below in addition to the concave area of the disc. The disc material ought to be eliminated with a pituitary rongeur and curettes; the dura and its contents are protected with a nerve root retractor. Complete visualization of the vertebral physique (arrow) with anterolateral protection. Axial schematic illustration of working down the pedicle with medial and lateral safety. Closure of Wedge Resection We place resected vertebral cancellous bone as well as allograft clips into the wedge resection website anteriorly. We place a downgoing supralaminar hook at the superior level and an upgoing infralaminar hook on the inferior level. We place a rod and compress with closure of the resection web site and correction of the deformity.
Extra-articular fractures of the femur (low neck treatment of hyperkalemia order 125mg sinemet amex, intertrochanteric treatment of criminals discount sinemet 110 mg fast delivery, and subtrochanteric fractures) have a great prognosis for therapeutic but are inclined to medicine 60 purchase generic sinemet pills lead to shortening administering medications 7th edition cheap sinemet 110 mg without a prescription, external rotation medicine man dispensary purchase sinemet overnight, and typically varus if untreated symptoms torn meniscus buy sinemet 300mg lowest price. There are progress plates beneath the capital femoral epiphysis, the higher trochanteric apophysis, and the lesser trochanteric apophysis. Femoral areas where hips fracture: intracapsular neck (green), extracapsular neck (blue), and intertrochanteric�subtrochanteric space (red). Extra-articular fractures (low neck, intertrochanteric, and subtrochanteric fractures) in kids lower than 6 years old can be handled by closed manipulation and spica casting. Preoperative Planning the injured hip ought to be evaluated under anesthesia using fluoroscopy. Approach Extra-articular fractures that are secure after reduction should be immobilized in a spica solid. Many neck fractures can be decreased closed and stuck percutaneously from laterally. If the fracture may be anatomically decreased, the surgeon should proceed with percutaneous fixation; if not, open reduction ought to be undertaken. After reduction, pins are drilled from the lateral femoral cortex retrograde throughout the fracture. C D It is customary to use clean pins for physeal separations or neck fractures in very younger kids. A lateral view, usually by frogging the hip, is important to verify pin placement. Because there could additionally be a tense hemarthrosis that tamponades circulate in the retinacular vessels of the neck, it may be wise to aspirate the joint capsule to evacuate or decompress the hip joint. The objective is anatomic reduction to keep perfusion to the capital femoral epiphysis, optimize bony apposition for healing, and stop deformity, especially varus and external rotation. The vastus lateralis is incised longitudinally, and the muscle tissue overlying the anterior hip capsule are elevated anteriorly. The incision is curved posteriorly and then extends distally in the posterior third of the vastus fascia. The angle the guidewire makes with the femoral shaft is dictated by the fixation system to be used. The fascia of vastus lateralis is "hockey sticked" and vastus muscle is retracted anteriorly, exposing the lateral femoral cortex. After fracture discount, a guidewire is inserted from the lateral femoral cortex up the femoral neck. The angle the wire makes with the lateral cortex ought to match the angle of the fixation gadget (usually 135 degrees). Reaming is achieved over the guidewire to accommodate the lag screw and the barrel of the facet plate. The plate is secured to the femur with cortical screws and the compression screw locks the lag screw within the facet plate. The surgeon ought to contemplate decompressing the hemarthrosis to reduce the impact of tamponade of the vessels. Parents are warned upfront of the chance and implications of avascular necrosis. Perfect discount and bony apposition present the most effective opportunity for fracture healing. Decompression and stable internal fixation of femoral neck fractures in kids can have an effect on the result. In youngsters who maintain multiple traumatic accidents, the character and severity of each damage should be considered to optimize treatment. The proximal ossification heart is seen by 6 months and the distal femoral ossification middle seems at 7 months. The profunda femoris artery offers rise to 4 perforating arteries, which enter the femur posteromedially. During fracture therapeutic, however, the majority of the blood is equipped by the periosteal circulation. The diploma of trauma required to trigger harm will increase exponentially as the character of the bone modifications and gradually turns into stronger and bigger from infancy to adolescence. Low-energy accidents resulting in fractures may point to a pathologic nature of the condition, besides in toddlers, in whom low-energy femur fractures are frequent. The position of the fracture fragments after the damage depends on the extent of the fracture and reflects the gentle tissue and muscle forces performing on the femur. In the setting of an isolated femur fracture, the thigh seems swollen with minor bruises and abrasions. Open wounds could change the administration of this injury; obvious deformity helps within the preliminary prognosis. The clinician palpates the length of the lower extremity, feeling for bony deformity and checking compartments rigorously for pressure. The clinicians should verify carefully for femoral, popliteal, dorsalis pedis, and posterior tibial pulses. Sensation to light contact is tested alongside the length of the complete decrease extremity. Diminished strength might indicate nerve harm or compartment syndrome or may also be secondary to pain. The clinician strikes the patellar and Achilles tendons with a reflex hammer and appears for contraction of the quadriceps and gastrocnemius, respectively. Diminished knee or ankle reflexes could indicate femoral or sciatic nerve injury or may be secondary to guarding. In circumstances of high-energy trauma, concomitant injuries to the skin and gentle tissue in addition to other organ systems are normally current. Radiographs should embody the joints above and beneath the fracture site to avoid lacking any concomitant injuries. The clinician inspects the lower extremity and appears for open wounds, bruising, or obvious deformity. For older kids and adolescents, 3 weeks of skeletal traction followed by spica casting was once frequent however has been replaced by internal or external fixation typically. Preoperative Planning A detailed evaluation of the medical findings and all appropriate imaging studies is carried out before the procedure. Shortening ought to be decided to be less than 2 cm using a lateral radiograph, though some suggest spica casting can be accomplished regardless of shortening. In infants, steady femoral shaft fractures could be handled in a Pavlik harness or a splint. In children younger than 6 years, closed reduction and casting is used within the vast majority of cases. Positioning the kid is taken to the operating room or sedation unit and placed in the supine position on the table. The injured extremity is casted first, after which the patient is transferred to a spica desk. Because of latest reviews of compartment syndrome of the leg after spica casting for pediatric femur fractures,8,9 many centers (ours included) have been using less hip and knee flexion and not including the foot for the forged of the injured leg. To keep away from vascular compromise, care should be taken not to flex the knee once the padding is in place. The affected person is transferred to a spica table, the place the burden of the legs is supported with manual traction. The remainder of the spica forged is positioned while holding the fracture out to length. Care ought to be taken to keep away from extreme traction, which increases the danger of compartment syndrome and skin sloughing. Gore-Tex liners are used at some institutions to forestall diaper rash and superficial infections. Traditional spica casting with 90 degrees of hip flexion, 30 levels of abduction, and 15 levels of exterior rotation. The foot stays uncovered with the forged stopping in the supramalleolar area, which is protected with further padding. The pelvic band is utilized with multiple layers of stockinette folded on the stomach to forestall stomach compression from the casting. Seven or eight layers of folded fiberglass are placed within the inter-hip crease to decrease the chance of the forged breaking, while a wide pelvic band is needed to immobilize the hip as nicely as potential. Cylinder forged with 50 degrees of knee flexion and forty five levels of hip flexion for strolling spica forged. Walking spica casting position with 30 levels of abduction and 15 degrees of external rotation. Wide pelvic band and anterior reinforcement for extra assist in a final walking spica cast. Shortening of more than 2 cm (controversial) Massive swelling of the thigh Associated damage that precludes solid therapy Walking spica Effective for low-energy isolated femur fractures Toddlers sometimes pull-to-stand and start walking in 2 to three weeks. We counsel the household, instantly after discount in casting, that wedging of the solid may be necessary at about 10 to 14 days after damage. This frequently avoids pointless journeys back to the operating room within the postoperative period for loss of reduction. Prior to callus formation, if shortening of greater than 2 cm occurs, certainly one of three options may be required: cast change, traction, or external fixation. Shortening of more than 2 cm as soon as callus has fashioned may be handled with osteoclasis and lengthening methods at a pace of 1 mm per day. Illgen and colleagues6 found that standard spica casting was profitable (without solid change or wedging) about 86% of the time. Immediate spica casting in the emergency division underneath acutely aware sedation and discharge has been proven to have comparable rates of complication and re-reduction as "early" spica casting. Epidemiology of femoral fractures in youngsters within the West Midlands region of England 1991 to 2001. Spica cast utility within the emergency room for select pediatric femur fractures. Fractures of the femoral shaft in youngsters: incidence, mechanisms, and sociodemographic risk factors. Compartment syndrome of the leg after treatment of a femoral fracture with an early sitting spica forged: a report of two cases. Volkmann contracture and compartment syndromes after femur fractures in kids treated with 90/90 spica casts. Childhood femur fractures, related injuries, and sociodemographic risk elements: a populationbased examine. Chapter 12 Closed Reduction and External Fixation of Femoral Shaft Fractures Stuart M. The peak in age distribution at age 2 is due to relative weak point of primarily woven bone at a time when ambulation will increase the risk of fall-related trauma. Most kids older than 6 years are actually handled with some type of operative fracture stabilization. Nonoperative choices include Pavlik harness or splints for kids younger than 6 months and a spica solid for these older than 6 months. In proximal and midshaft femoral shaft fractures, the proximal fragment tends to be forced into abduction and external rotation. Fractures of the distal third of the femoral shaft have a tendency to not deform significantly, while supracondylar femoral fractures are often forced into apex posterior angulation. In younger youngsters, polytrauma, head injury, high-energy trauma, an open fracture, extreme comminution, or body habitus incompatible with spica cast care are relative indications for operative management. Surgical choices include versatile nailing, plating, inflexible intramedullary nailing, and exterior fixation. Indications for external fixation embrace polytrauma, concomitant head damage, open fracture with severe gentle tissue harm or contamination, extreme comminution, and very proximal subtrochanteric or distal diaphyseal�metaphyseal junction fracture. Midshaft transverse fractures are at a better risk of refracture when handled with exterior fixation compared to other methods of stabilization. In adolescents, they tend to be higherenergy accidents that will result from motorized vehicle, biking, or high-speed sporting accidents. Abuse should be thought-about in the toddler or toddler with a femur fracture, particularly if the child is nonambulatory. If child abuse is suspected, a skeletal survey must be obtained and Child Protective Services must be notified. Infants are more likely than toddlers to be the victims of kid abuse in the setting of a femoral fracture. Radiographs should be evaluated for fracture sample, location, displacement, angulation, and shortening. In each fragment there should be at least 2 cm of intervening bone between the physis and the outermost pin and at least 2 cm between the fracture and the innermost pin. Positioning the affected person should be placed on both a radiolucent working table or a fracture desk. After making a stab incision over the first pin web site, the surgeon dissects bluntly to the close to cortex. The trocar is inserted into the gentle tissue information and seated onto the femur perpendicular to its lengthy axis. The trocar is eliminated and the gentle tissue guide is impacted gently to forestall slippage. The applicable drill information (based on the chosen screw size) is inserted into the delicate tissue information. After attaching a drill cease onto the suitable bit, the surgeon drills through the near cortex, using the drill information to keep the pilot gap perpendicular to the long axis of the bone. The drill bit and the drill information are eliminated without unseating the soft tissue guide. The appropriate screw is inserted into the pilot hole, and the screw is advanced using the T-wrench until it protrudes 2 mm beyond the far cortex. The surgeon slides the telescoping arm of the assembled fixator onto the screw within the appropriate position. The soft tissue guide is inserted into another clamp place on the identical telescoping arm.
Buy sinemet 300 mg visa. The great porn experiment | Gary Wilson | TEDxGlasgow.
Injuries sustained to the medial facet of the patellofemoral joint might result in medications 5113 buy 125mg sinemet with amex ligament disruption of the medial patellofemoral ligament with or without stretching or tearing of the medial retinaculum medications you cant take with grapefruit generic 300mg sinemet free shipping. This may lead to medicine 831 buy generic sinemet on line persistent pain or recurrent instability of the patellofemoral joint severe withdrawal symptoms buy sinemet 125 mg overnight delivery. The key to remedy is the persistent complaint of instability emotions and examination in keeping with instability with or with out ache medications images generic sinemet 110 mg online. It is commonly tough to distinguish between a medial collateral ligament tear medicine jobs discount sinemet 125 mg with amex, a meniscal tear, or an acute patellofemoral subluxation or dislocation. The bony anatomy of the patellofemoral joint may also be abnormal with a deficient lateral femoral slope of the trochlear groove, resulting in decreased pressure needed to laterally translate or dislocate the patella. If a loose physique exists, as in other circumstances, surgical intervention is warranted. Forty to 60% of the resistance to lateral translation is supplied by the medial patellofemoral ligament. It extends from the medial side of the patella, about 10 to 15 mm distal to the superior pole of the patella, near the widest portion of the patella, to the medial epicondylar space just above the origin of the medial collateral ligament. The lateral retinaculum may also be tight, characterized by lower than 12 mm of medial translation. The quadriceps angle may be greater than common, growing the lateral translational force. So-called miserable malalignment syndrome may exist, including excessive femoral anteversion with or without increased exterior tibial torsion. A thorough examination will embody the next: Examination for effusion Patellar stability testing. Instability of 25% to 50% indicates elevated laxity however a still-competent retinaculum and medial patellofemoral ligament. Femoral rotation: Average rotation is exterior rotation larger than or equal to inner movement. The clinician ought to observe and palpate the patella for lateral subluxation (J sign) throughout lively vary of motion. In young athletes, it can occur during a valgus twisting maneuver such as swinging a baseball bat while twisting out of the greatest way of a pitch. Each radiograph is evaluated for fracture or loose fragment necessitating extra emergent surgical indications. Nonoperative treatment is appropriate for a number of dislocators or subluxators, especially those that have generalized ligamentous laxity or an atraumatic type of presentation. Some advocate early surgical intervention to repair the medial patellofemoral ligament and medial retinaculum even without fractures or loose body. Nonoperative routine for a dislocation contains: Rest, ice, compression, and elevation, plus anti-inflammatory medications Immobilization for about 6 weeks Immediate physical remedy to strengthen the weakened quadriceps and a patellar protection program Bracing, with a lateral patellar restraint kind of brace, for return to exercise Treatment choices for recurrent subluxation ought to embrace: Bracing with a lateral patellar restraint sort of brace Physical remedy: a patellar protection program emphasizing strengthening of the hip flexors, abductors (which are routinely weak on this patient population), and quadriceps in particular the clinician ought to emphasize to the patient that therapy requires participation at home in addition to at remedy classes. The foot of the desk is flexed about 30 to forty five degrees and a lateral publish is used for valgus moment, visualizing the medial compartment. Subcutaneous flaps could be elevated to allow great mobility of the prepatellar pores and skin to limit the size of the incision. Alternatively, an open subcutaneous lateral release may be carried out through a 1-cm incision, together with the medial plication�imbrication, or both could also be accomplished through a midline incision. The surgeon should be wary of operative therapy for sufferers with pain with out instability. Recurrent dislocators who dislocate in a brace during physical exercise regardless of good effort during remedy and coaching in addition to those that dislocate throughout activities of daily living in a brace after therapy are candidates for surgical intervention. Any free physique or patellar avulsion fractures with large displaced fragments are indications for early surgical intervention. Preoperative Planning All imaging research are reviewed for other pathology that also needs to be addressed concurrently. Before positioning, an examination of the knee underneath anesthesia (including ligamentous testing) must be carried out. The examination should include a Lachman check, pivot shift, varus�valgus stress test, and anterior�posterior drawer in addition to medial and lateral patellar stability testing at forty five levels of knee flexion. The surgical incision is centered over the medial facet of the widest portion of the patella. This incision within the tendon and the retinaculum is made from about three to four cm above the superior pole of the patella distally to 3 to 4 cm distal to the inferior pole of the patella medial to the tendon, leaving enough retinaculum with the tendon to suture to . With the three sutures held tight, the knee is placed through a spread of movement, from full extension to 90 degrees of flexion, to check that sufficient imbrication has been carried out. The sutures are then tied and a 0 absorbable suture is used above and under the imbrication to reinforce the tension set by these sutures. A operating 0 absorbable suture then can be sutured over the imbrication to help reinforce the imbrication as well as decrease its profile. Medial parapatellar incision is made with 2 to 3 mm of quadriceps tendon left attached to the vastus medialis obliquus. The knee is positioned at 45 levels of flexion, with the patella centered in the femoral groove; set the tension of the medial side by imbricating the medial retinaculum. The distance from the widest portion of the patella to the deliberate puncture web site is measured. The graft is subperiosteally reflected distally about 10 to 12 mm from the superior pole of the patella (more distally laterally than medially, to allow it to fold over on itself during fixation and tensioning). A nonabsorbable suture is placed within the free finish of the graft, with a whipstitch or other graft stitch performed with two ends. The pressure is then set through the medial retinacular suture plication as described above before setting the stress of the graft. It is additional secured by 0 absorbable sutures in the graft and retinaculum, catching the graft superficial and deep to the retinaculum because the free end of the graft is directed again towards the patella. Once the graft is secured and imbrication is full, the knee is flexed to 90 degrees to make certain that no overtightening of the quadriceps mechanism has occurred and that the sutures keep in place. The surgeon dissects deep to the medial retinaculum, posterior to the medial epicondyle and the medial intermuscular septum. If the medial patellofemoral ligament is to be reconstructed, the surgeon measures the size of graft needed. A full-thickness quadriceps tendon graft 6 to eight mm extensive is obtained, with attachment to the patella maintained at its widest portion. The medial retinaculum is punctured at the level marked by placement anterior to the intermuscular septum, distal to the vastus medialis obliquus, and superficial to the medial epicondyle. The graft is tensioned and secured to the medial retinaculum�intermuscular septum, also at 45 degrees. A careful examination ought to be accomplished to decide whether or not reconstruction of the medial patellofemoral ligament is warranted. Tension setting the surgeon should make positive that the patella interprets close to 25% of its width laterally. If medial patellofemoral ligament reconstruction is being performed on the same time, the strain should be set with the retinacular imbrication before tensioning the graft (this avoids over-tensioning). Quadriceps graft management Care should be taken not to detach the quadriceps graft from the patella utterly. Dissecting extra distally on the lateral facet of the patellar attachment permits for the graft to lay down on itself. When passing the graft through the puncture hole in the retinaculum, a snap or Kocher clamp is used to maintain the sew within the free finish. It is pulled via according to the graft (the surgeon ought to push anterior to posterior, not pull posterior to anterior). Fixation issues the graft is sutured at the patellar attachment as it folds over itself. Physical remedy for vary of motion (passive and lively assisted) ought to be started within the first few days to fight arthrofibrosis. Weight bearing is protected with crutches till the affected person is comfy enough to walk in a locked knee brace in full extension. During the preliminary section of remedy, patellar mobilization, quadriceps activation, straight-leg raises, pain modalities, and edema management are important. Range of movement is restricted to zero to 90 degrees for the first 3 to 4 weeks postoperatively. At 4 weeks, full range of movement is allowed, with progressive quadriceps strengthening, edema control, and ache management, and gait coaching is initiated. Brace use in neighborhood settings is sustained till enough quadriceps energy has returned (about 6 weeks). Late fixation failure is uncommon however can occur if flexion past 90 degrees is started too quickly postoperatively. Continued ache could happen, especially if not sufficient or too aggressive of a lateral launch was carried out, resulting in either elevated pressure on the patella or medial pressure and instability. Injury to the cutaneous nerves is frequent, and patients must be warned of this threat. Tensile energy of the medial patellofemoral ligament earlier than and after repair or reconstruction. This harm generally happens in the younger age group, significantly in these with open progress plates. The classification proposed by Meyers and McKeever was later modified by Zaricznyj to embrace a fourth sort, which might signify a comminuted fragment. Usually a patient with a tibial spine harm may have a historical past of trauma or sports-related harm; the most common mechanism is normally a fall from a bicycle. Knee joint laxity is present, as well as an incapability to bear weight on the affected extremity. Most sufferers have some extent of swelling due to hemarthrosis secondary to the intra-articular fracture. Other superficial injuries are associated to the diploma and nature of the traumatic occasion. The ligamentous ends of the medial and lateral menisci likewise insert into the intercondylar eminence. It is extra common in children, significantly these with incomplete ossification and open development plates. The incompletely ossified tibial spine is primarily cartilaginous, which is weaker in resisting tensile forces. The ordinary mechanism of harm is a forced valgus moment utilized to the knee, which is coupled with external rotation forces. Other mechanisms reported include hyperextension of the knee coupled with rotational moments. The valgus force utilized to the leg together with slight flexion of the knee ends in the pivot shift phenomenon. The intact iliotibial band reduces the femur when the knee is brought into 20 to 30 degrees of flexion. This maneuver may be effective for lesions which may be large enough to embrace a half of the tibial plateau. Previous authors have beneficial various degrees of flexion, ranging from 10 to forty levels. The leg may be placed on the operating table with the knee joint past the break within the desk. This allows the knee to flex ninety degrees when the decrease end of the table is dropped down, allowing the knee to dangle off the table. For open discount strategies, the affected person is positioned supine on the working desk, a tourniquet is placed on the thigh, and the knee is draped in a regular fashion. If the avulsed fragment has a comparatively large osseous part, plain radiographs will normally suffice in determining treatment. The choice of surgical therapy (open versus arthroscopic reduction) as well as the choice of fixation gadget largely is decided by the choice and expertise of the surgeon and the character of the lesion. Inevitably, the final determination as to which fixation gadget is finest is made intraoperatively. The hemarthrosis is eliminated to permit for direct inspection and evaluation of the knee joint. The base of the fracture fragment is d�brided using shavers and curettes and the fracture hematoma is carefully eliminated. If any interposing construction is found preventing reduction, it should be carefully retracted and sutured or repaired if essential. Midpatellar tendon portals may be added to allow using accent probes and instruments. The place of the information pin is checked under fluoroscopy to ensure proper placement and to keep away from traversing the growth plate. A second pin may be introduced, relying on the soundness of the fracture discount, to maintain the fragments in place. The screw size is essentially dependent on whether the fracture fragments will accommodate the screw. The knee is gently flexed and extended whereas the soundness of the discount is checked underneath direct vision. Once passable discount is documented, the devices are removed and the arthroscopic portals closed. A suture passer is used to grab the suture ends by way of a transphyseal tunnel and the suture ends are tied in the anteromedial border of the tibia. If discount is discovered to be insufficient, fixation could additionally be augmented with percutaneous Kirschner wires or cannulated screws as wanted. Once enough discount had been achieved, light flexion and extension of the knee is performed to check for stability of reduction. When passable discount of the fracture is obtained and documented, then the devices are removed and the arthroscopic portals are closed. Kirschner Wire Fixation and Percutaneous Pinning After adequate discount of the fracture is obtained, the fracture fragment is held in reduction. Proper placement of the Kirschner wires is documented radiographically and arthroscopically.
It is better to overimmobilize in questionable circumstances to keep away from malalignment and regain motion later with aggressive physiotherapy symptoms you are pregnant buy genuine sinemet. Removal of symptomatic hardware (ie symptoms 6 days before period discount sinemet 110 mg with mastercard, nails or plate) ought to be delayed till fracture healing and reworking are complete symptoms 4dp3dt purchase discount sinemet on line. I choose to take away elastic nails electively in all sufferers 6 to 9 months after damage treatment xerosis buy discount sinemet on-line, because the nails will turn into fully intramedullary with significant continued growth medications made from animals buy sinemet without prescription, thus making late removal extremely troublesome medications 3 times a day order generic sinemet from india. Myers and coworkers10 reported a significant complication price in high-energy tibial fractures treated with external fixation, including delayed union, malunion, leg-length discrepancies, and pin-tract infections. Kubiak and colleagues8 reported 2 delayed unions, 2 malunions, and 3 nonunions in a series of 15 sufferers managed with external fixation, although these seem to have occurred in open accidents. They reported greater practical scores in their patients handled with elastic intramedullary nailing in comparison with exterior fixation. Operative strategies normally require extra procedures for removal of pins or distinguished nails or plates. External fixation or versatile intramedullary nailing for femoral shaft fractures in kids: a potential, randomised examine. Ender nail fixation in lengthy bone fractures: experience in a level I trauma center. Problems of operative and non-operative treatment and therapeutic in tibial fractures. Operative remedy of tibial fractures in youngsters: are elastic stable intramedullary nails an enchancment over exterior fixation Flexible titanium nailing for the remedy of unstable pediatric tibial fracture. Chapter 17 Open Reduction and Internal Fixation of Tibial Tuberosity Fractures Ernest L. There have also been stories of related injuries similar to quadriceps tendon harm, cruciate ligament tears, and meniscal injury. Patients with minimally displaced fractures may lengthen the knee, however with apparent discomfort. This is unlike Osgood-Schlatter illness, by which the onset is more continual and there could also be radiographic findings of a persistent situation corresponding to calcification anterior to the secondary middle of ossification. The second, or apophyseal stage, occurs at age eight to 12 years in girls and 9 to 14 years in boys. The third, or epiphyseal, stage is when the "tongue" of the apophysis and the epiphyseal bone are steady. The ages for the third stage are 10 to 15 years for ladies and 11 to 17 years for boys. The insertion is lateral to the midline; thus, the fracture fragment is centered lateral to the midline. This is important when considering the approach for intra-articular visualization. Bleeding from its proximal branches as it retracts into the anterolateral compartment could result in compartment syndrome. There is a significant pressure that the quadriceps mechanism is ready to generate, and this overcomes the strength of the epiphysis and the encompassing periosteum. The different mechanism of harm is sudden passive knee flexion while the quadriceps is contracted. In nondisplaced fractures the place sufferers can perform a straight-leg raise, a long-leg forged could additionally be used for remedy. Even in the nondisplaced fractures, percutaneous screw fixation might enable earlier immobilization and prevent 6 to eight weeks of casting. The desk should permit good anterior and posterior views to be obtained with fluoroscopy. The tourniquet can be used to maintain the sphere dry, allowing for good visualization of the fracture fragments and the joint discount. The tourniquet, however, might prevent the quadriceps from being freely mobilized and will make reduction more challenging. The proximal extent is the midpatella and the distal facet is a few centimeters distal to the tibial tubercle fracture bed. There is a significant quantity of hematoma formation and torn periosteum; thus, the incision size permits the surgeon to define the appropriate anatomy and put together the fragment for reduction. Since the tubercle and the fracture are on the lateral side of the proximal tibia, a lateral parapatellar strategy will give better visualization of the fracture and intra-articular discount. The lateral method also limits any harm to the infrapatellar department of the saphenous nerve. Lateral radiograph of a 13-year-old woman who sustained a tibial tuberosity fracture. There is commonly a protracted periosteal flap of the proximal tibia seen with the elevated fragment that should be extracted from the fracture. The distal, medial, and lateral extent of the fracture must be surgically outlined with sharp dissection. For the sort of fracture that exits the anterior part of the knee joint, the surgeon must visualize the knee joint. This may be achieved by wanting into the knee through the fracture or by a parapatellar approach. Often the articular floor can be first reduced and the distal facet then decreased into the base. A 15-year-old boy with a displaced tibial tuberosity fracture that enters the joint floor. Initial postoperative lateral radiograph after open reduction and internal fixation. Despite initial fluoroscopic views indicating an adequate reduction, the radiographs point out a poor discount. The lateral meniscus was impeding the prior discount and it was removed from the fracture website. Provisional Kirschner wires may be placed to maintain the reduction before screw fixation. It is essential to prevent vascular damage posterior to the knee joint in this area. We usually use a washer for the thinner cortical bone on the distal region of the fracture. Anterior radiograph exhibits the screws are lateral to the midline as the fracture is more lateral. Smaller bone fragments will likely require extra immobilization than bigger bone fragments, the place higher fixation may be achieved. Avulsion fracture of the tibial tuberosity with mixed ligament and meniscal tear. Fracture of the tibial tuberosity with associated ligamentous and meniscal tears: a case report. All research have been constant in their conclusion that the fractures heal with success and patients return to normal perform. Loss of movement or quadriceps muscle weakness is extremely uncommon however could happen with a malunion or malreduction. Surgical treatment is mandated with any vital articular incongruity as in the adult inhabitants. It is our expertise that physeal fractures of the distal tibia require near-anatomic alignment to forestall the complication of untimely physeal closure. The commonest classification scheme for pediatric ankle fractures is the anatomic Salter-Harris technique for physeal fractures. We have discovered the Lauge-Hansen mechanistic classification derived for adults may be very helpful, as this aids in conceptualizing the reduction method by reversing the fracture sample. Also, our knowledge have shown that pronation-type accidents have a higher fee of premature physeal closure than the supination�external rotation type of injuries. Additional classification systems include the fibular-based Danis-Weber system, as nicely as a extra complete classification suggested by Dias and Tachdjian that makes use of the Lauge-Hansen pointers correlated with the Salter-Harris classification. Tillaux fractures happen most often in adolescents within 1 yr of distal tibial physeal closure. They involve an external rotational pressure that avulses off the anterolateral side of the tibial epiphysis, which is attached to the anterior tibiofibular ligament, which is stronger than the residual open physis laterally. The anteroinferior tibiofibular ligament attaches strongly to the anterolateral border of the tibial epiphysis, and with an external rotation force on the foot it has the flexibility to avulse off the anterior lateral fragment of the tibial epiphysis; the energy imbalance between the ligament and weaker physis can create the transitional Tillaux and triplane fractures. The anatomy of the distal tibial physis is related to understanding certain ankle fractures and their administration and prognosis. The secondary ossific nucleus of the distal epiphysis seems between 6 and 24 months, with the apophysis of the medial malleolus often extending from an elongation from this ossific nucleus or from a separate ossification heart, the os subtibiale, which ossifies between 7 and 8 years of age. Physeal closure of the distal tibia happens round 15 years of age in ladies and 17 years of age in boys. The perichondral ring of La Croix is a transitional space between the articular cartilage and the periosteum of the diaphysis, which is perichondrium and retains the potential for producing cartilage and bone. Functionally, the perichondral ring offers stability to the physis and should play a role in sure fractures and development plate injuries in kids. Specific anatomy and growth plate closure patterns create certain fractures in adolescence. For instance, the same exterior rotation mechanism can produce a Tillaux or a triplane fracture depending on the age and degree of physeal closure of the child. This is often an area of weakness in the skeletally maturing youngster, permitting an anterolateral fragment to be avulsed from the epiphysis, creating Tillaux fractures or the fragments in the triplane fracture. These data have relevance in operative indications in pediatric ankle fractures, as an earlier sequence demonstrated a 3. Our experience suggests that periosteum interposed in the physis results in residual fracture gapping and in the end premature physeal closure. The orthopaedic surgeon ought to focus on the potential for untimely physeal closure with the household on the initial go to, significantly with an abduction type of harm. Basic examination ought to encompass evaluating the skin and soft tissues, finding areas of maximal tenderness to palpation, and acquiring an accurate sensory, motor, and vascular examination. Particular points that have to be thought-about in the diagnosis of ankle fractures in youngsters embody osteomyelitis and baby abuse. It usually happens in the vascular loops of the metaphyseal areas of bone in kids and can happen due to hematogenous unfold or because of trauma, which may further complicate prognosis. A good history of the proximity of ache onset relative to the inciting trauma will assist differentiate trauma from an infection. Metaphyseal fractures of the distal tibia in children may be concerning for baby abuse, as the mechanism can be attributed to forceful pulling or twisting of the extremity, fracturing the cancellous bone through the metaphysis. Additional concerns are bilateral extremity fractures and fractures at totally different stages of therapeutic. The quality of skin can also affect the timing of surgical fixation and provides perception into the power and location of damage. Palpation of the ankle can help in locating the damage and will enable analysis of occult physeal fractures or ligamentous injuries not seen on radiographs. Establishing preoperative deficits is crucial of their postoperative management and aids in establishing the need to release the extensor retinacular compartment. In ankle injuries preoperative deficits could be due to nerve contusion or laceration, along with tendon disruption or mechanical block. If a deficit is still present after discount, a vascular study could additionally be considered versus immediate operative exploration to consider for transient spasm or vascular harm. Abduction injuries had a relatively poor prognosis for premature physeal closure whether or not the intervention was closed treatment (54. Accessory ossicles can be generally visualized on plain radiographs and may be confused with ankle fractures. These embody the os subtibiale medially (up to 20% of population), the os trigonum posteriorly (about 10% of population), and the os fibulare laterally (about 1% of population). Contralateral comparability films may be helpful to differentiate accent ossicles from a fracture. Reductions generally take place in our emergency division with the use of ketamine for acutely aware sedation and the assist of a transportable picture intensifier. Reduction maneuvers ought to reverse the established mechanism of damage derived from affected person history and fracture sample, such because the Quigley maneuver for the abduction�external rotation kind of fractures. In youngsters with a high-energy mechanism or with any neurovascular change that has not improved after discount, admission for serial neurovascular checks to monitor for compartment syndrome is really helpful. If lateral ankle exposure is necessary, a bump can be placed beneath the operative hip to improve lateral visualization. The picture intensifier is positioned with the screen on the foot of the desk angled toward the surgeon on the operative side, while the C-arm should come in directly from the alternative side of the operative ankle. The operative leg could be elevated with blankets or a foam pad to permit a pull-through lateral view unobstructed by the contralateral extremity. Nonsterile tourniquets are utilized as proximal as potential before sterile draping. Long-leg fiberglass solid after discount of distal tibial physeal fracture is univalved, spacers are later placed, and the solid is overwrapped with waterproof tape. We really feel these research are essential in preoperative planning in many complex ankle fractures, particularly triplane fractures. The anterior method includes an incision of about 8 to 10 cm over the distal tibia. The superficial peroneal nerve lies over the ankle retinaculum at this level and ought to be averted. The superior extensor retinaculum is incised at the interval between the extensor digitorum longus and the extensor hallucis longus. Care is taken to not injure the neurovascular bundle consisting of the deep peroneal nerve and anterior tibial artery, which lies on this interval. The posteromedial method to the ankle consists of an incision about eight to 10 cm roughly midway between the medial malleolus on the medial border of the Achilles tendon.