Mara Decker, DrPH
- Assistant Adjunct Professor

https://publichealth.berkeley.edu/people/mara-decker/
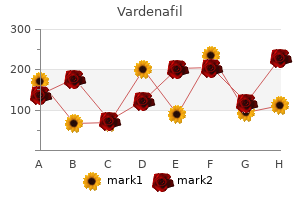
The ether bond and carbonhalogen bond are the sites in the anesthetic molecule most prone to oxidative metabolism erectile dysfunction groups cheap vardenafil 20mg amex. The exercise of hepatic cytochrome P-450 enzymes answerable for metabolism of volatile anesthetics may be increased by a selection of medication erectile dysfunction drugs in the philippines cheap vardenafil 20 mg with visa, together with the anesthetics themselves impotence is the buy vardenafil american express. An estimated 3% of absorbed enflurane undergoes oxidative metabolism by cytochrome P-450 enzymes to kind inorganic fluoride and organic fluoride compounds (see Table 4-7) latest erectile dysfunction drugs discount vardenafil online master card. Desflurane produces the highest carbon monoxide focus (package insert for desflurane describes this risk) followed by enflurane and isoflurane. Nevertheless, carbon monoxide formation is a risk of sevoflurane administration in the presence of desiccated carbon dioxide absorbent especially when an exothermic reaction between the volatile anesthetic and desiccated absorbent happens. Delayed neurophysiologic sequelae because of carbon monoxide poisoning (cognitive defects, persona changes, gait disturbances) may occur as late as 3 to 21 days after anesthesia. An estimated 5% of absorbed sevoflurane undergoes oxidative metabolism by cytochrome P-450 enzymes to form natural and inorganic fluoride metabolites (see Table 4-7). Peak plasma fluoride concentrations are larger after administration of sevoflurane than after comparable doses of enflurane, but the length of publicity of renal tubules to fluoride that results from sevoflurane metabolism is restricted due to the fast pulmonary elimination of this poorly blood-soluble anesthetic. Hepatic manufacturing of fluoride from sevoflurane may be less of a nephrotoxic danger than is intrarenal production of fluoride from enflurane. No different class of pharmacologic agents is extra central to the apply of anesthesiology than the intravenous sedatives and hypnotics (anxiolysis, gentle and deep sedation, basic anesthesia). Sedative refers to a drug that induces a state of calm or sleep, whereas hypnotic refers to drug that induces hypnosis or sleep. There is significant overlap in the two terms and infrequently refer to all of these medicine as sedativehypnotics. Depending on the particular agent, the dose, and the speed of administration, many sedative-hypnotics can be utilized to allay anxiety with minimal sedation, produce various degrees of sedation, or quickly induce the state of drug-induced unconsciousness (general anesthesia). An various to emulsion formulations of propofol and associated unwanted side effects (pain on injection, threat of an infection, hypertriglyceridemia, pulmonary embolism) is creation of a prodrug (Aquavan). Clearance of propofol from the plasma exceeds hepatic blood circulate, emphasizing that tissue uptake (possibly into the lungs), in addition to hepatic oxidative metabolism by cytochrome P450, is essential in elimination of this drug from the plasma (Table 5-1). Prompt restoration without residual sedation and low incidence of nausea and vomiting make propofol particularly nicely suited to ambulatory conscious sedation strategies. In selected Chapter 5 � Intravenous Sedatives and Hypnotics Table 5-1 Comparative Characteristics of Common Induction Drugs Elimination Half-Time (h) Propofol Etomidate Ketamine zero. Increasing metabolic acidosis, lipemic plasma, bradycardia, and progressive myocardial failure has been described. General anesthesia that includes propofol is usually related to minimal postoperative nausea and vomiting, and awakening is immediate, with minimal residual sedative effects. The incidence of postoperative nausea and vomiting is decreased when propofol is administered, whatever the anesthetic method. Propofol decreases the prevalence of wheezing after induction of anesthesia and tracheal intubation in healthy and asthmatic patients. However, a formulation of propofol that uses metabisulfite as a preservative may cause bronchoconstriction in asthmatic patients. The relaxation of vascular easy muscle produced by propofol is primarily due to inhibition of sympathetic vasoconstrictor nerve activity. Peripheral vascular effects of thiopen, tal and propofol in people with artificial hearts. The blood pressure results of propofol could also be exaggerated in hypovolemic sufferers, elderly patients, and patients with compromised left ventricular operate. Profound bradycardia and asystole after administration of propofol have been described in wholesome grownup sufferers, despite prophylactic anticholinergics (risk of bradycardia-related death throughout propofol anesthesia has been estimated to be 1. Treatment of propofol-induced bradycardia might require therapy with a direct -agonist similar to isoproterenol. Propofol produces dose-dependent melancholy of ventilation, with apnea occurring in 25% to 35% of patients after induction of anesthesia with propofol. Opioids administered with the preoperative treatment improve ventilatory depressant. Prolonged infusions of propofol can also lead to excretion of green urine, reflecting the presence of phenols within the urine (does not alter renal function). Urinary uric acid excretion is increased after administration of propofol and will manifest as cloudy urine when the uric acid crystallizes within the urine beneath circumstances of low pH and temperature (not thought-about to be detrimental). Propofol is associated with vital decreases in intraocular pressure that happen instantly after induction of anesthesia and are sustained throughout tracheal intubation. Patients who develop evidence of anaphylaxis on first exposure to propofol might have been beforehand sensitized to the diisopropyl radical, which is current in plenty of dermatologic preparations. Anaphylaxis to propofol during the first publicity to this drug has been observed, particularly in patients with a historical past of different drug allergies, often to neuromuscular blocking medicine. Lactic acidosis ("propofol infusion syndrome") has been described in pediatric and adult sufferers receiving prolonged high-dose infusions of propofol (75 g/kg/ minute) for longer than 24 hours. The mechanism for sporadic propofol-induced metabolic acidosis is unclear but might mirror poisoning (cytopathic hypoxia) of the electron transport chain and impaired oxidation of long chain fatty acids by propofol or a propofol metabolite in uniquely susceptible sufferers (mimics the mitochondrial myopathies). The majority of reported propofol-induced "seizures" throughout induction of anesthesia or emergence from anesthesia replicate spontaneous excitatory movements of subcortical origin (not thought to be as a result of cortical epileptic activity). There seems to be no reason to avoid propofol for sedation, induction, and maintenance of anesthesia in patients with known seizures. Intense dreaming activity, amorous behavior, and hallucinations have been reported during restoration from and low-dose infusions of propofol. Propofol strongly helps the growth of Escherichia coli and Pseudomonas aeruginosa. Postoperative surgical infections manifesting as temperature elevations have been attributed to extrinsic contamination of propofol. Propofol has potent antioxidant properties that resemble these of the endogenous antioxidant vitamin E (neuroprotective impact of propofol). Pain on injection is probably the most commonly reported antagonistic occasion associated with propofol administration to awake sufferers. Preceding the propofol with 1% lidocaine or prior administration of a potent short-acting opioid decreases the incidence of discomfort experienced by the patient. An oral formulation of etomidate for transmucosal supply has been proven to produce dose-dependent sedation. The anesthetic effect of etomidate resides predominantly in the R isomer, which is roughly five instances as potent as the S isomer. Etomidate is rapidly metabolized by hydrolysis of the ethyl ester aspect chain to its carboxylic acid ester, resulting in a water-soluble, pharmacologically inactive compound. Involuntary myoclonic actions are common in the course of the induction period because of alteration in the stability of inhibitory and excitatory influences on the thalamocortical tract (frequency of this myoclonic-like activity may be attenuated by prior administration of an opioid). The principal limiting issue in the scientific use of etomidate for induction of anesthesia is the flexibility of this drug to transiently depress adrenocortical perform. Suppression of adrenocortical function limits the medical usefulness for long-term treatment of intracranial hypertension. This attribute may be used to facilitate localization of seizure foci in sufferers undergoing cortical resection of epileptogenic tissue. Etomidate also possesses anticonvulsant properties and has been used to terminate status epilepticus. Etomidate has been noticed to increase the amplitude of somatosensory evoked potentials, making monitoring of those responses extra reliable. Etomidate has been proposed for induction of anesthesia in patients with little or no cardiac reserve. In nearly all of sufferers, etomidate-induced decreases in tidal quantity are offset by compensatory increases within the frequency of breathing. Pain on injection and venous irritation has been just about eradicated with use of etomidate in a lipid emulsion automobile rather than propylene glycol. These spontaneous movements, particularly myoclonus, occur in 50% to 80% of sufferers receiving etomidate in the absence of premedication. The mechanism of etomidate-induced myoclonus appears to be disinhibition of subcortical structures that usually suppress extrapyramidal motor activity. Etomidate causes adrenocortical suppression by producing a dose-dependent inhibition of the conversion of cholesterol to cortisol. Conceivably, sufferers experiencing sepsis or hemorrhage and who would possibly require an intact cortisol response could be at a drawback ought to etomidate be administered. Conversely, suppression of adrenocortical function could be thought of desirable from the standpoint of "stress-free" anesthesia.
The decrease areas include clusters of enormous erectile dysfunction over the counter cheap vardenafil 20mg without prescription, round neurones with brief and profusely branching dendrites erectile dysfunction drugs lloyds buy vardenafil overnight delivery. Upper and decrease zones differ in their connections erectile dysfunction 21 purchase vardenafil 20mg free shipping, however both obtain terminals from the dorsal spinal roots in any respect ranges erectile dysfunction 60784 order vardenafil cheap online. Dorsal funicular fibres from neurones within the spinal gray matter terminate solely within the superior, reticular zone. Variable ordering and overlap of terminals, on the basis of spinal root levels, happen in each zones. The lower extremity is represented medially, the trunk ventrally and the digits dorsally. Its center zone contains a big pars rotunda, by which rostrocaudally elongated, medium-sized neurones are clustered between bundles of densely myelinated fibres. The reticular poles of its rostral and caudal zones include scattered however evenly distributed neurones of varied sizes. The nucleus receives the lateral fibres of the fasciculus cuneatus, carrying proprioceptive impulses from the upper limb (which enter the cervical spinal twine rostral to the thoracic nucleus). A group of neurones, referred to as nucleus Z, has been recognized in animals between the upper pole of the nucleus gracilis and the inferior vestibular nucleus and is said to be present within the human medulla. Its input might be from the dorsal spinocerebellar tract, which carries proprioceptive information from the ipsilateral decrease limb, and it initiatives through internal arcuate fibres to the contralateral medial lemniscus. The trigeminal sensory nucleus receives the primary afferents of the trigeminal nerve. It is a big nucleus and extends caudally into the cervical spinal cord and rostrally into the midbrain. The principal and largest division of the nucleus is situated in the pontine tegmentum. On entering the pons, the fibres of the sensory root of the trigeminal nerve run dorsomedially towards the principal sensory nucleus, which is situated at this degree. Before reaching the nucleus, roughly 50% of the fibres divide into ascending and descending branches; the others ascend or descend with out division. The descending fibres, 90% of which are less than 4 �m in diameter, form the spinal tract of the trigeminal nerve, which reaches the higher cervical spinal twine. Fibres from the ophthalmic root lie ventrolaterally, these from the mandibular root lie dorsomedially and the maxillary fibres lie between them. The tract is completed on its dorsal rim by fibres from the sensory roots of the facial, glossopharyngeal and vagus nerves. The detailed anatomy of the trigeminospinal tract excited early scientific interest because it was recognized that dissociated sensory loss might happen in the trigeminal area. There are conflicting opinions concerning the termination pattern of fibres in the spinal nucleus. The outcomes of section of the spinal tract in cases of extreme trigeminal neuralgia support this distribution. To embrace the mandibular space, it was necessary to section on the level of the obex. More just lately, it has been proposed that fibres are arranged dorsoventrally throughout the spinal tract. There seem to be sound anatomical, physiological and scientific reasons for believing that all divisions terminate all through the whole nucleus, though the ophthalmic division might not project fibres as far caudally because the maxillary and mandibular divisions do. Fibres from the posterior face (adjacent to C2) terminate within the decrease (caudal) part, whereas these from the upper lip, mouth and nasal tip terminate at the next level. This can provide rise to a segmental (cross-divisional) sensory loss in syringobulbia. Fibres of the glossopharyngeal, vagus and facial nerves subserving frequent sensation (general visceral afferent) form a column dorsally throughout the spinal tract of the trigeminal nerve and synapse with cells within the lowest part of the spinal trigeminal nucleus. Consequently, operative section of the dorsal a half of the spinal tract ends in analgesia that extends to the mucosa of the tonsillar sinus, the posterior third of the tongue and adjoining parts of the pharyngeal wall (glossopharyngeal nerve) and the cutaneous space provided by the auricular branch of the vagus. Other afferents that reach the spinal nucleus are from the dorsal roots of the higher cervical nerves and from the sensorimotor cortex. The spinal nucleus is taken into account to include three elements: the subnucleus oralis (which is most rostral and adjoins the principal sensory nucleus), the subnucleus interpolaris and the subnucleus caudalis (which is essentially the most caudal part and is steady beneath with the dorsal grey column of the spinal cord). The construction of the subnucleus caudalis is completely different from that of the other trigeminal sensory nuclei. There is a somatotopic pattern of termination of cutaneous inputs from the upper limb on the cell clusters of the pars rotunda. The gracile and cuneate nuclei serve as relays between the spinal cord and higher ranges. Primary spinal afferents synapse with multipolar neurones in the nuclei to kind the main nuclear efferent projection. Descending afferents from the somatosensory cortex attain the nuclei by way of the corticobulbar tracts and seem to be restricted to the upper, reticular zones. Because these afferents each inhibit and enhance activity, the nuclear region is clearly considered one of sensory modulation. Neurones of dorsal column nuclei obtain terminals of long, uncrossed, primary afferent fibres of the fasciculi gracilis and cuneatus, which carry data concerning deformation of the skin, motion of hairs, joint movement and vibration. Unit recording of the neurones in dorsal column nuclei reveals that their tactile receptive fields. Some fields have excitatory centres and inhibitory surrounds, which signifies that stimulation just outdoors its excitatory subject inhibits the neurone. Neurones within the nuclei are spatially organized into a somatotopic map of the periphery (in accord with the same localization within the dorsal columns). However, some neurones receive convergent input from tactile pressure and hair follicle receptors. A number of control mechanisms can modulate the transmission of impulses by way of the dorsal column�medial lemniscus pathway. Concomitant activity in adjoining dorsal column fibres could result in presynaptic inhibition by depolarization of the presynaptic terminals of considered one of them. Stimulation of the sensorimotor cortex additionally modulates the transmission of impulses by both pre- and postsynaptic inhibitory mechanisms, and generally by facilitation. Modulation of transmission by inhibition also results from stimulation of the reticular formation, raphe nuclei and different sites. The accent cuneate nucleus, dorsolateral to the cuneate, is a part of the spinocerebellar system of precerebellar nuclei. These form the posterior 164 Chapter 10 / Brain Stem Cerebellar folium Fourth ventricle Superior medullary velum Superior cerebellar peduncle Mesencephalic tract of trigeminal nerve Principal sensory nucleus of trigeminal nerve Medial longitudinal fasciculus Motor nucleus of trigeminal nerve Central tegmental tract Trigeminal nerve Middle cerebellar peduncle Lateral lemniscus Descending fibres of cortical origin Trapezoid nucleus Medial lemniscus and trapezoid body Transverse pontine fibres. Spinal nucleus of trigeminal nerve Dorsal cochlear nucleus Lateral vestibular nucleus Medial longitudinal fasciculus Fourth ventricle Stria medullaris Vagal nucleus Tectospinal tract Inferior cerebellar peduncle Reticular formation Nucleus ambiguus Ventral cochlear nucleus Central tegmental tract Vestibular nerve Olivocerebellar fibres Medial accent olivary nucleus Inferior olivary nucleus Medial lemniscus Ventral spinocerebellar tract Lateral spinothalamic tract Arcuate nuclei Anterior exterior arcuate fibres Pyramid. Many of the neurones within the subnucleus caudalis that reply to cutaneous or tooth pulp stimulation are also excited by noxious electrical, mechanical or chemical stimuli derived from the jaw or tongue muscles. This signifies that convergence of superficial and deep afferent inputs through wide dynamic vary or nociceptive-specific neurones happens in the nucleus. Similar convergence of superficial and deep inputs occurs within the rostral nuclei and will account for the poor localization of trigeminal ache and for the unfold of pain, which regularly makes analysis troublesome. These fibres instantly or indirectly (through local interneurones) affect ache notion. Stimulation of the periaqueductal gray matter or nucleus raphe magnus inhibits the jaw opening reflex to nociception and will induce primary afferent depolarization in tooth pulp afferents and other nociceptive facial afferents. Neurones within the subnucleus caudalis may be suppressed by stimuli utilized outside their receptive subject, notably by noxious stimuli. The subnucleus caudalis is a crucial website for relay of nociceptive input and functions as a half of the pain `gate management. Tooth pulp afferents via broad dynamic range and nociceptivespecific neurones could terminate in rostral nuclei, which all project to the subnucleus caudalis. Most fibres arising within the trigeminal sensory nuclei cross the midline and ascend in the trigeminal lemniscus. They finish within the contralateral thalamic nucleus ventralis posterior medialis, from which third-order neurones project to the cortical postcentral gyrus (areas 1, 2 and 3). However, some trigeminal nucleus efferents ascend to the nucleus ventralis posterior medialis of the ipsilateral thalamus. Hypoglossal Nucleus the distinguished hypoglossal nucleus lies close to the midline within the dorsal medullary grey matter. The hypoglossal nucleus consists of enormous motor neurones interspersed with myelinated fibres.
The dorsal horn is a major receptive zone (zone of termination) of major afferent fibres drugs for erectile dysfunction pills generic vardenafil 20mg visa, which enter the spinal twine via the dorsal roots of spinal nerves impotence signs order 10mg vardenafil with visa. Dorsal root fibres include numerous molecules which are both identified or suspected to fulfill a neurotransmitter or neuromodulator function erectile dysfunction and marijuana order discount vardenafil. The bigger motor neurones within the ventral grey column are visibly grouped (cresyl quick violet stain) erectile dysfunction 21 years old vardenafil 10mg sale. This is a poorly understood dysfunction that may be caused by a gradual dropout of motor units or muscle fibres as a result of getting older superimposed on residual anterior horn cells that had been previously depleted as a result of the unique poliomyelitis. Increased metabolic demand on the maximally reinnervated motor models may play a major role. At age four years he had acute poliomyelitis, characterised by profound weak point of each lower extremities and less severe weak point of the higher extremities. Upper extremity strength improved considerably thereafter, however he had persistent weak point within the decrease extremities, which progressively improved. After 2 years he continued to exhibit weak point and significant atrophy of all muscles in the right decrease extremity, significantly the gastrocnemius. He was unchanged thereafter till age 60, when he started to expertise elevated weakness within the decrease extremities, notably on the proper facet, finally necessitating the usage of a leg brace. He additionally complains of ache in the right lower extremity, especially in the knee and ankle, and notes international fatigue. Neurological examination demonstrates mild weakness in the left lower extremity and marked weak spot of all muscle teams in the proper decrease extremity, notably the dorsiflexors and plantar flexors of the right foot. An electromyogram with a nerve conduction study of the decrease extremities reveals denervation in all muscles examined. Phagocytic neuronophagic (microglial) clusters mark the location of dying motor neurones. He has famous increasing problem jogging and has had a number of falls because of catching his foot on a curb. He additionally reviews deterioration in his penmanship and hassle typing on his pc keyboard. He denies signs referable to bulbar function and has experienced no sphincter disturbances. Pathologically, degeneration is observed primarily within the anterior horns of the spinal twine, in motor cranial nerve nuclei, and in the lateral corticospinal tracts. Although it begins at spinal ranges, the illness generally spreads to involve motor cranial nerve nuclei, with resultant dysarthria, dysphagia and impaired respiratory function. Cross-section stained for myelin sheaths demonstrates degeneration of the lateral (corticospinal) pathways (arrows); less marked modifications mirror lack of recurrent anterior horn cell collateral fibres. Kubik Laboratory of Neuropathology, Massachusetts General Hospital, Tessa Hedley-White, Director. Most if not all primary afferent fibres divide into ascending and descending branches on getting into the wire. These then journey for variable distances in the tract of Lissauer, close to the surface of the twine, and send collaterals into the subjacent grey matter. The formation, topography and division of dorsal spinal roots have all been confirmed in humans. At the dorsolateral tip of the dorsal horn, deep to the tract of Lissauer, lies a thin lamina of neurones, the lamina marginalis. It receives afferents by way of the dorsal roots and is the location of origin of the spinothalamic tract complicated. These propriospinal neurones link segments for the mediation of intraspinal coordination. In the human spinal wire, it can often be recognized from the eighth cervical to the third or fourth lumbar segments. Some ship axons into the dorsal spinocerebellar tracts, and others are interneurones. It is the supply of the sacral outflow of parasympathetic preganglionic nerve fibres. Ventral Horn Lateral Horn the lateral horn is a small lateral projection of grey matter situated between the dorsal and ventral horns. It is current from the eighth cervical or first thoracic section to the second or third lumbar phase. These develop within the embryonic twine dorsolateral to the central canal and migrate laterally, forming intermediomedial and intermediolateral cell columns. Their axons journey by way of ventral spinal roots and white rami communicantes to the sympathetic trunk. The largest cell our bodies, which may exceed 25 �m in diameter, are these of motor neurones whose axons emerge in ventral roots to innervate extrafusal fibres in striated skeletal muscle tissue. Some of these are motor neurones, which innervate intrafusal fibres of muscle spindles, and the rest are interneurones. Considered longitudinally, ventral horn neurones are organized in elongated groups and form a quantity of separate columns that reach through several segments. The ventral horn is actually divided into medial, central and lateral cell columns, all of which are subdivided at sure levels, usually into dorsal and ventral parts. In segments cranial and caudal to this area, the medial group has solely a ventromedial moiety, besides in the first cervical phase, the place solely the dorsomedial group exists. The central group of cells is the least extensive and is found solely in some cervical and lumbosacral segments. The third to seventh cervical segments contain the centrally located phrenic nucleus; abundant experimental and scientific proof reveals that its neurones innervate the diaphragm. Neurones whose axons are thought to enter the spinal accessory nerve kind an irregular accent group within the upper 5 or 6 cervical segments on the ventral border of the ventral horn. Descending corticospinal and reticulospinal tracts involved in sensory modulation are also indicated. The nucleus of Onuf, which is assumed to innervate the perineal striated muscles, is a ventrolateral group of cells within the first and second sacral segments. The fundamental arrangement is that medial cell groups innervate the axial musculature, and lateral cell groups innervate the limbs. The fundamental building block of the somatic motor neuronal populations is represented by a longitudinally disposed group of neurones that innervate a given muscle and by which the and motor neurones are intermixed. The numerous groups innervating totally different muscular tissues are aggregated into two main longitudinal columns: medial and lateral. The medial longitudinal motor column extends throughout the size of the spinal twine. Basically, epaxial muscles embrace the erector spinae group (which extend the head and vertebral column), and hypaxial muscle tissue embrace prevertebral muscles of the neck, intercostal and anterior stomach wall muscular tissues (which flex the neck and the trunk). The epaxial muscular tissues are innervated by branches of the dorsal primary rami of the spinal nerves, and the hypaxial muscle tissue are innervated by branches of the ventral primary rami. In the medial column, motor neurones supplying epaxial muscle tissue are sited ventral to these supplying hypaxial muscular tissues. The lateral longitudinal motor column is found solely in the enlargements of the spinal cord. The motor neurones on this column in the cervical and lumbar enlargements innervate muscular tissues of the higher and lower limbs, respectively. In the cervical enlargement, motor neurones that provide muscle tissue intrinsic to the upper limb are located dorsally in the ventral grey column, and people innervating probably the most distal (hand) muscles are situated farther dorsally. Motor neurones of the girdle muscle tissue lie within the ventrolateral part of the ventral horn. There is a further somatotopic organization, in that the proximal muscular tissues of the limb are provided from motor cell groups positioned more rostrally within the enlargement than those supplying the distal muscles. For example, motor neurones innervating intrinsic muscular tissues of the hand are sited in segments C8 and T1, whereas motor neurones of shoulder muscle tissue are in segments C5 and C6. A comparable total association of motor neurones innervating decrease limb muscle tissue applies within the lumbosacral wire. The primary afferent connections to motor neurones are direct monosynaptic connections from proprioceptive dorsal root afferents in the identical or close by segments, connections from axonal collaterals of dorsal horn and other interneurones and direct monosynaptic connections from the vestibulospinal and corticospinal tracts. The intrinsic connections of the spinal wire and mind stem subserve numerous reflexes by which the features of peripheral constructions are modulated in response to afferent information in a relatively computerized or autonomous trend.
Opioid-induced nausea and vomiting are brought on by direct stimulation of the chemoreceptor trigger zone in the floor of the fourth ventricle erectile dysfunction treatment lloyds pharmacy order vardenafil 20mg without prescription. Morphine can also trigger nausea and vomiting by growing gastrointestinal secretions and delaying passage of intestinal contents towards the colon erectile dysfunction code red 7 purchase vardenafil mastercard. Opioids are readily transported across the placenta (depression of the neonate can occur) erectile dysfunction from smoking purchase vardenafil australia. The principal manifestation of opioid overdose is despair of air flow erectile dysfunction niacin cheap vardenafil 20mg on-line, manifesting as a slow respiratory frequency, which can progress to apnea (triad of miosis, hypoventilation, and coma ought to recommend overdose with an opioid). Pharmacodynamic tolerance and physical dependence with repeated opioid administration are characteristics of all opioid agonists and are among the main limitations of their clinical use. The most notable characteristic of the medical use of opioids is the extraordinary variation in dose requirements for effective treatment of ache. Morphine is the prototype opioid agonist to which all other opioids are compared, producing analgesia, euphoria, sedation, nausea, and pruritus (especially within the cutaneous areas around the nose). In contrast to nonopioid analgesics, morphine is efficient against pain arising from the viscera. Analgesia is most outstanding when morphine is administered before the painful stimulus happens (in the absence of ache, nonetheless, morphine may produce dysphoria somewhat than euphoria). Table 7-4 Chapter 7 � Opioid Agonists and Antagonists Pharmacokinetics of Opioid Agonists Context Sensitive Half-Time: Effect-Site Percent Protein Volume of Elimination 4-Hour (Blood�Brain) Nonionized Binding Clearance Distribution Partition Half-Time Infusion Equilibration (pH 7. Metabolism of morphine is primarily via conjugation with glucuronic acid in hepatic and extrahepatic websites, particularly the kidneys (about 75% to 85% of a dose of morphine appears as morphine-3-glucuronide [pharmacologically inactive], and 5% to 10% as morphine-6-glucuronide [pharmacologically lively with an analgesic potency 650-fold larger than morphine]). The decrease in the plasma focus of morphine after preliminary distribution of the drug is principally as a outcome of metabolism as a end result of only a small amount of unchanged opioid is excreted within the urine. Meperidine is an artificial opioid agonist at and opioid receptors (analogues of meperidine embody fentanyl, sufentanil, alfentanil, and remifentanil). Meperidine shares a quantity of structural features which might be current in local anesthetics and structurally is similar to atropine (possesses a gentle atropine-like antispasmodic impact on clean muscle). Meperidine is about one-tenth as potent as morphine producing equivalent sedation, euphoria, nausea, vomiting, and melancholy of air flow with a duration of action of two to 4 hours. Metabolism is intensive, with about 90% of the drug initially undergoing demethylation to normeperidine and hydrolysis to meperidinic acid. Normeperidine (one-half as energetic as an analgesic) subsequently undergoes hydrolysis to normeperidinic acid. Normeperidine toxicity manifesting as myoclonus and seizures is more than likely throughout extended administration (3 days) of meperidine as throughout patient-controlled analgesia, particularly within the presence of impaired renal operate. Meperidine may be efficient in suppressing postoperative shivering that may result in detrimental will increase in metabolic oxygen consumption (antishivering effects might mirror stimulation of receptors) 5. Side effects of meperidine generally resemble those described for morphine, however meperidine, in contrast to morphine, rarely causes bradycardia but as a substitute might enhance heart fee, reflecting its modest atropine-like qualities. Large doses of meperidine end in decreases in myocardial contractility, which, amongst opioids, is unique for this drug. The greater potency and extra fast onset of motion replicate the throughout the blood�brain barrier. The lungs additionally function a large inactive storage web site, with an estimated 75% of the preliminary fentanyl dose present process first-pass pulmonary uptake. Fentanyl is extensively metabolized by N-demethylation and the pharmacologic activity of fentanyl metabolites is believed to be minimal. Despite the scientific impression that fentanyl has a short period of action, its elimination half-time is longer than that for morphine (see Table 7-4). This longer elimination half-time reflects a larger quantity of distribution (Vd) of fentanyl due to its larger lipid solubility and thus extra fast passage into highly vascular tissues compared with the much less lipid-soluble morphine (more than 80% of the injected dose leaves the plasma in 5 minutes). As the duration of steady infusion of fentanyl increases beyond about 2 hours, the context-sensitive half-time of this opioid turns into larger than sufentanil. This displays saturation of inactive tissue sites with fentanyl throughout prolonged infusions and return of the opioid from peripheral compartments to the plasma. This tissue reservoir of fentanyl replaces fentanyl eradicated by hepatic metabolism in order to gradual the rate of decrease in the plasma concentration of fentanyl when the infusion is discontinued. Side results of fentanyl resemble those of morphine (persistent or recurrent melancholy of ventilation). Analgesic concentrations of fentanyl significantly potentiate the effects of benzodiazepines (marked synergism with respect to hypnosis and melancholy of ventilation). In scientific apply, the advantage of synergy between opioids and benzodiazepines for the upkeep of affected person comfort is rigorously weighed against the disadvantages of the doubtless antagonistic depressant results of this combination. The elimination half-time of sufentanil is intermediate between that of fentanyl and alfentanil (see Table 7-4). A speedy redistribution to inactive tissue sites terminates the impact of small doses, but a cumulative drug impact can accompany massive or repeated doses of sufentanil. Sufentanil is rapidly metabolized by N-dealkylation and the products are pharmacologically inactive, whereas desmethyl sufentanil has about 10% of the activity of sufentanil. Context-sensitive half-time of sufentanil is less than that for alfentanil for continuous infusions of up to eight hours in duration. After termination of a sufentanil infusion, the decrease within the plasma drug focus is accelerated by metabolism and by continued redistribution of sufentanil into peripheral tissue compartments. Compared with alfentanil, sufentanil could have a more favorable recovery profile when used over a longer time period. Conversely, alfentanil has a pharmacokinetic benefit for the remedy of discrete and transient noxious stimuli as a end result of its brief effect-site equilibration time allows fast entry of the drug to the mind and facilitates titration. Alfentanil has a short elimination half-time compared with fentanyl and sufentanil (see Table 7-4). Despite its lesser lipid solubility, penetration of the blood�brain barrier by alfentanil is rapid because of its large nonionized fraction at physiologic pH. The effectivity of hepatic metabolism is emphasized by clearance of about 96% of alfentanil from the plasma inside 60 minutes of its administration. Attempts to develop dependable infusion regimens to attain and keep specific plasma concentrations of alfentanil have been confounded by the 10-fold interindividual variability in alfentanil pharmacokinetics. The context-sensitive half-time of alfentanil is actually longer than that of sufentanil for infusions up to 8 hours in duration. Despite the short elimination half-time of alfentanil, it may not essentially be a superior choice to sufentanil for ambulatory sedation methods. Alfentanil has a speedy onset and offset of intense analgesia, reflecting its very prompt effect-site equilibration. Alfentanil, compared with equipotent doses of fentanyl and sufentanil, is related to a lower incidence of postoperative nausea and vomiting in outpatients. Although chemically associated to the fentanyl family of short-acting phenylpiperidine derivatives, remifentanil is structurally unique because of its ester linkage structure that renders it prone to hydrolysis by nonspecific plasma and tissue esterases to inactive metabolites. This distinctive pathway of metabolism leads to (a) brief motion, (b) precise and rapidly titratable effect because of its fast onset and offset, (c) lack of accumulation, and (d) speedy restoration after discontinuation of its administration. Because of its speedy systemic clearance, remifentanil supplies pharmacokinetic advantages in scientific situations requiring predictable termination of drug impact. The mixture of speedy clearance and small Vd produces a drug with a uniquely transient impact (context-sensitive half-time of the remifentanil plasma focus is almost unbiased of the infusion duration). Remifentanil is exclusive among the opioids in undergoing metabolism by nonspecific plasma and tissue esterases to inactive metabolites. Context-sensitive half-time for remifentanil is unbiased of the duration of infusion and is estimated to be about four minutes (rapid clearance is liable for the lack of accumulation even throughout prolonged periods of infusion) (see Table 7-4). Clinical uses of remifentanil mirror the distinctive pharmacokinetics of this drug, which allows speedy onset of drug effect, precise titration to the specified effect, the Chapter 7 � Opioid Agonists and Antagonists 173 35 30 Control Propofol (1. The combined administration of remifentanil and propofol decreased the slope of the carbon dioxide response curve and triggered a rightward shift. Nausea and vomiting, melancholy of ventilation, and mild decreases in systemic blood stress and coronary heart price might accompany the administration of remifentanil. Postoperative analgesic requirements in sufferers receiving relatively large doses of remifentanil intraoperatively are often surprisingly high, suggesting remifentanil may be associated with acute opioid tolerance. Codeine is the outcome of the substitution of a methyl group for the hydroxyl group on the quantity 3 carbon of morphine. Maximal analgesia, equivalent to that produced by 650 mg of aspirin, occurs with 60 mg of codeine. Oxymorphone is about 10 occasions as potent as morphine and appears to trigger extra nausea and vomiting. Oxycodone is often used orally for treating acute pain (about twice as potent as oral morphine and has an identical duration of analgesic action).
Generic vardenafil 20mg otc. What Is Male Sexual Dysfunction? (1 Erection Herb To Boost Sex).
References
- Garner AA, Crooks J, Lee A, Bishop R. Efficacy of prehospital critical care teams for severe blunt head injury in the Australian setting. Injury. 2001;32(6):455-460.
- Hilmi IA, Damian D, Al-Khafaji A, et al. Acute kidney injury following orthotopic liver transplantation: incidence, risk factors, and effects on patient and graft outcomes. Br J Anaesth. 2015.
- Patterson DE, Segura JW, LeRoy AJ, et al: The etiology and treatment of delayed bleeding following percutaneous lithotripsy, J Urol 133(3):447n451, 1985.
- Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. J Athle Train. 2004;39(1):77-82.
- Gabrielson E. Worldwide trends in lung cancer pathology. Respirology 2006;11:533-8.