Morton J. Kern,MD
- Clinical Professor of Medicine
- Associate Chief of Cardiology
- Department of Cardiology
- University of California Irvine
- Orange, California
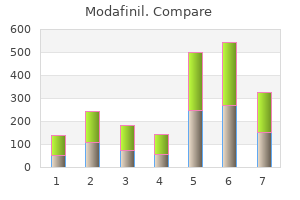
Chapter 84 Myocarditis and Pericarditis 85 Definition Epidemiology Mediastinitis Trevor C insomnia kevin gates lyrics discount modafinil 100mg amex. Diagnosis Microbiology � Esophageal rupture is often manifested by chest ache sleep aid gift ideas proven modafinil 100mg, shortness of breath sleep aid for anxiety purchase generic modafinil on line, and odynophagia insomnia ubrania purchase modafinil australia. Prevention � Oral microbiota insomnia xmovies8 purchase 100 mg modafinil overnight delivery, including streptococci insomnia used in a sentence buy 200mg modafinil free shipping, gram-negative bacilli, and anaerobes, predominate in mediastinitis as a outcome of esophageal perforation and descending head and neck infections. Mediastinitis can be organized into acute or chronic forms with etiologies, clinical shows, and treatments which may be strikingly totally different. Acute mediastinitis is an uncommon but potentially devastating an infection involving the structures of the mediastinum. Before the development of refined techniques in cardiovascular and thoracic surgery, most instances resulted from esophageal perforation or contiguous unfold from oropharyngeal foci. Mediastinitis now occurs most frequently as a postoperative an infection after median sternotomy. Regardless of the pathogenesis of an infection, a high index of suspicion have to be maintained for this infection in order that aggressive, potentially lifesaving measures can be promptly initiated. Chronic mediastinitis, also referred to as fibrosing, sclerosing, or granulomatous mediastinitis, is a uncommon dysfunction often brought on by Histoplasma capsulatum. The sternum and costal cartilages make up the anterior boundary, and the 12 thoracic vertebral bodies border the mediastinum posteriorly. The mediastinum is arbitrarily divided into four subdivisions: superior, posterior, anterior, and center. Structures throughout the mediastinum include the guts and nice vessels, esophagus, distal portion of the trachea and mainstem bronchi, vagus and phrenic nerves, thymic remnants, and thoracic duct. These buildings are surrounded by adipose tissue, loose connective tissue, and lymph nodes. The mediastinum communicates with the buildings of the pinnacle and neck through several fascial planes and potential spaces (see Chapter 64). The three main routes by which head and neck infections spread to the mediastinum are (1) the pretracheal area, (2) the long fascial planes of the posterior neck, and (3) the viscerovascular or lateral pharyngeal space. The long fascial planes of the posterior neck prolong from the bottom of the skull to the diaphragm and embody the retropharyngeal or retrovisceral area, the prevertebral space, and the hazard space. Infection Originating at Another Site Pneumonia; pleural house an infection or empyema; subphrenic abscess; pancreatitis; cellulitis or soft tissue infection of the chest wall; osteomyelitis of sternum, clavicle, ribs, or vertebrae; hematogenous spread from distant foci Lymph nodes: necrosis and hemorrhage (anthrax) or caseous necrosis (tuberculosis) by the lateral pharyngeal area in 21% and the pretracheal space in 8%. Essentially all cases of mediastinitis are due to the unfold of an infection from different websites or direct inoculation resulting from trauma or surgery. The pathogenesis, medical manifestations, and treatment differ in accordance with the underlying reason for mediastinitis. Spontaneous pneumomediastinum is caused by alveolar rupture with air transferring to the mediastinum, and is usually a benign situation not requiring antibiotics, surgical intervention, or often even hospitalization. A necrotizing chemical mediastinitis ensues, followed by a polymicrobial bacterial mediastinitis, which is usually synergistic and necrotizing. Mediastinitis Secondary to Esophageal Perforation Mediastinitis Secondary to Head and Neck Infections or From Other Sites Before the event of cardiac surgery, perforation of the esophagus was the leading reason for mediastinitis, adopted by suppurative infections of the oropharynx. Spread of infection from the neck into the mediastinum is influenced by respiratory dynamics, in which the unfavorable intrathoracic Mediastinitis secondary to pharyngeal and odontogenic infections is often known as "descending necrotizing mediastinitis or fasciitis," and earlier than antibiotics have been extensively out there, it accounted for 10% to 31% of mediastinitis instances. Middle-aged males predominate in most case collection, with typically less than half of cases of descending necrotizing mediastinitis ensuing from oral infections. The prototypic odontogenic infection resulting in mediastinitis is Ludwig angina, which usually stems from an infection of the second or third mandibular molars spreading to involve the sublingual and submandibular areas (see Chapter 64). From these spaces the an infection can unfold via the lateral pharyngeal space to contain the retropharyngeal area or carotid sheath and observe into the mediastinum. These infections can simply spread into the superior mediastinum via the long fascial planes of the neck or, if the danger space is involved, into the posterior mediastinum. Of 286 deep neck infections at a single center over 11 years, only 6% progressed to contain the mediastinum. The pretracheal area descends into the anterior mediastinum and most frequently is concerned in mediastinitis complicating procedures involving the thyroid and trachea. Cardiothoracic operations are among the many most common surgical procedures performed in bigger hospitals, and thus mediastinitis has turn into a predominantly postsurgical infection. Many research have documented the incidence and risk elements for the development of mediastinitis after cardiothoracic surgery. In 1984 Sarr and colleagues19 reviewed the obtainable literature and found the incidence of mediastinitis to be zero. Risk components generally may be divided into the following categories: preoperative, intraoperative, and postoperative (Table 85. Risk elements which were identified preoperatively embody rising age, diabetes mellitus, weight problems, earlier sternotomy, continual obstructive pulmonary disease, peripheral vascular illness, class 3 or 4 angina, renal failure requiring hemodialysis, history of endocarditis, cigarette smoking, low cardiac output states, preoperative Staphylococcus aureus colonization, hair elimination with razor versus removing with electric clippers, and prolonged preoperative hospitalization. A body mass index of greater than 30 will increase the chance of growing mediastinitis 2. This hypothesis has been supported by a quantity of laboratory and quite a few clinical studies. Most studies inspecting these threat factors are retrospective case-control research and are restricted by the problems References 20, 21, 23, 24, 25, 26, 28, 32, 33, 34, 35, 36, 37, 38. More than 20 years ago, Loop and colleagues20 discovered the risk of mediastinitis elevated with the variety of models of blood transfused postoperatively, and more just lately, Risnes and colleagues26 noted a similar association between transfusion of multiple units of blood and mediastinitis. The use of mechanical support devices, together with left ventricular help gadgets and intraaortic balloon pumps, either earlier than or after cardiac surgery, has been associated with a rise within the risk of mediastinitis. Donor-torecipient transmission of micro organism rarely has been noticed to result in mediastinitis. Through culturing the nares of medical personnel, they were also in a place to present that well being care workers had been hardly ever the supply of S. Pathogenic mechanisms and skill to cause illness may differ relying on the infecting organism. Certain strains of coagulasenegative staphylococci may be notably tailored to causing mediastinitis in the postoperative interval. Archer and Armstrong80 confirmed that sufferers are colonized by small numbers of antibiotic-resistant, coagulase-negative staphylococci, which turn into the predominant species when subjected to the selective pressure of prophylactic antibiotics. In addition, Olsson and colleagues81 famous coagulase-negative staphylococci isolated from deep sternal wounds were more more probably to produce biofilm. The bacteriology of mediastinitis complicating cardiovascular surgical procedure is strikingly totally different from mediastinitis secondary to head and neck infections or esophageal perforations (Table eighty five. Mediastinitis secondary to cardiothoracic surgery is primarily brought on by gram-positive cocci and less often by gram-negative bacilli. Bacteria are in a position to propagate in the protected avascular space of the surgical wound and cause infection. Gram-positive bacilli-Actinomyces, Eubacterium, Lactobacillus Gram-negative cocci-Veillonella Gram-negative bacilli-Bacteroides spp. Gram-positive bacilli-Corynebacterium Gram-negative cocci-Moraxella Gram-negative bacilli-Enterobacteriaceae, Pseudomonas spp. Chest radiograph reveals giant pneumomediastinum and pneumopericardium (arrows) in a affected person with mediastinitis. Synergistic an infection comprising both oral anaerobes and gram-negative bacilli is usually present. The most incessantly isolated organisms embody viridans group streptococci; staphylococci, together with S. The relative frequency with which these organisms are isolated varies due to the difficulty in acquiring reliable anaerobic tradition data. When mediastinitis occurs due to extension of an odontogenic or pharyngeal an infection, the symptoms and indicators of the first infections predominate, corresponding to pain, odynophagia, skin erythema, fever, and swelling of the affected website. Esophageal perforation could also be clinically obvious or inapparent relying on the nature of the damage. Early in the course of mediastinitis, the indicators and symptoms may be delicate, but because the condition progresses, patients observe rising chest pain, respiratory distress, and odynophagia. Chest ache is often probably the most prominent symptom and will localize relying on the portion of the mediastinum concerned. In anterior mediastinitis, ache is commonly located within the cervical or substernal region. Pain from posterior mediastinitis might localize to the epigastric area with radiation to the interscapular area. Pleural effusion is a common complication and may manifest as pleuritic chest ache. Retroperitoneal extension may be accompanied by acute abdominal indicators and should immediate unnecessary exploratory laparotomy. Examination regularly reveals fever; tachycardia, crepitus, and edema of the chest or neck can also be present. Hamman sign, a crunching, rasping sound heard over the precordium synchronous with the cardiac rhythm, brought on by emphysema of the mediastinum, could additionally be audible in 50% of patients with pneumomediastinum. In the later phases of mediastinitis, indicators of bacteremia and sepsis might predominate. The early prognosis of mediastinitis in an toddler or neonate may be notably difficult. A peculiar, interrupted, staccato type of inspiration has been described in plenty of sufferers. Complications of mediastinitis, corresponding to pleural effusion or pneumoperitoneum, can also be evident. Chest radiographs in sufferers with esophageal perforation reveal significant abnormalities in about 90% of patients, though establishing the presence of a perforation could be tough, and a number of modalities of imaging and direct visualization using endoscopy are sometimes essential to affirm the diagnosis. Although dilute barium supplies higher definition of anatomy and detection of refined defects and perforations, 1170 may experience greater-than-normal postoperative ache, which may be pleuritic in nature. Sternal instability, dehiscence, and wound drainage are frequently famous and may be the only sign of infection in patients. Poststernotomy mediastinitis manifesting as a deep neck abscess without irregular findings on chest examination has been reported, as has the event of septic shock and bacteremia with out apparent indicators of sternal infection. Biologic markers corresponding to C-reactive protein and procalcitonin are usually elevated. Procalcitonin has been shown to be superior to C-reactive protein in diagnosing infection in patients having undergone cardiopulmonary bypass however has not been particularly studied in mediastinitis. Characteristic findings embrace soft tissue swelling, pleural or pericardial effusions, fluid or air collections (or both), and sternal erosion. The diagnostic worth of nuclear scans has been espoused by several investigators and may be notably useful when different imaging is equivocal. Other authors have disagreed with the usefulness of epicardial pacer wire cultures. Two massive studies, including greater than 2000 sufferers, found routine pacer wire culture to be associated with an unacceptably excessive fee of false-positive findings. Several investigators have found mediastinal needle aspiration to be helpful within the prognosis of mediastinitis. Computed tomography scan of the chest on the level of the sixth thoracic vertebra exhibits large abscess within posterior mediastinum and left-sided pleural effusion. The patient had skilled perforation of the esophagus owing to a swallowed foreign physique. Approximately 90% of patients with inhalational anthrax exhibit mediastinal adenopathy or widening on radiographic studies. Post�cardiothoracic surgical procedure mediastinitis typically turns into clinically evident within 2 to four weeks after surgery, though uncommon instances occurring greater than 1 12 months after surgical procedure have been reported. The principles of managing mediastinitis as a result of esophageal perforation include restoration of esophageal continuity, management of mediastinal contamination, and treatment with antimicrobials. Barrett119 is credited with documenting in 1946 the first profitable remedy of mediastinitis resulting from esophageal perforation. Since then, consultants have often recommended immediate aggressive surgical drainage, d�bridement of any devitalized tissue, and repair of the perforation. Recent literature suggests that preferred algorithmic approaches keep in mind the situation, severity, and control of the esophageal leak, along with the presence of tumor and severity of sickness, to determine the most effective technique for esophageal restore. A major development in remedy of esophageal perforation has been the event of endoscopic therapies, such as retrievable esophageal stents and endoscopic clips. Clipping may be notably useful with small perforations due to overseas our bodies. A systematic evaluation of 267 esophageal perforations managed by esophageal stenting noted perforation healing was achieved in 85% of patients with an overall mortality of 11%. Children with esophageal perforation are often efficiently managed with conservative therapy with broad-spectrum antibiotics, nasopharyngeal aspiration, parenteral nutritional support, and drainage of any fluid collections. There is a few debate in the literature concerning the preferred surgical approach, however all authors agree that sufficient surgical drainage and d�bridement of all infected areas is of major importance. Some authors have suggested that a transthoracic approach is necessary in all cases, noting that transcervical drainage could additionally be inadequate. When infection is confined to the superior mediastinum, management using cervicotomy with transcervical mediastinal drainage is likely adequate. Empirical regimens should be chosen based on the underlying cause and canopy the main pathogens listed in Table eighty five. Penicillin G has historically been the antibiotic of choice in the treatment of anaerobic infections originating above the diaphragm and continues to exhibit glorious activity in opposition to most oral anaerobic micro organism. Gram-negative enteric bacilli are additionally typically involved in mediastinitis and must be accounted for when choosing an preliminary empirical regimen. Thus regimens including a -lactam/-lactamase inhibitor, a broadspectrum cephalosporin plus metronidazole or clindamycin, or a carbapenem are affordable empirical options.
Of the forty one instances reported in the literature from 1945 to 1999 insomnia ovulation discount modafinil 100mg overnight delivery, 75% appeared to outcome from erosion of the aortic wall by a contiguous focus and 25% appeared to outcome from direct seeding of the aortic intima or through the vasa vasorum sleep aid up up info discount modafinil online visa. The first two brokers might involve intracranial arteries by direct extension from foci of sinusitis sleep aid capsules cheap modafinil 100 mg without prescription. One case of a quantity of intracranial aneurysms because of insomnia forum safe modafinil 100mg Coccidioides immitis that occurred during remedy for basilar meningitis has been described insomnia bakery order modafinil 200 mg online. Fungi additionally may cause endarteritis within the aorta or on aortic grafts insomnia craig david purchase discount modafinil on-line, together with Aspergillus or Bipolaris spp. Chapter eighty Endocarditis and Intravascular Infections Etiologic Agents Laboratory Findings 1106 Pseudoaneurysms resulting from intraarterial or perivascular injection of illicit avenue medication, usually in addicts with sclerosed veins because of repeated intravenous inoculation, are related to contiguous abscesses. In a review of fifty six aneurysms occurring in 45 sufferers,902 3 of 20 patients died when therapy was limited to antibiotics alone. Likewise, 6 of 25 sufferers for whom therapy included antibiotics and surgery died and 9 of 19 survivors had been left with mild-to-moderate neurologic deficits. In different studies, the investigators reported a different experience, with a higher mortality in the nonsurgical group,827 but sufferers have been chosen solely after subarachnoid hemorrhage had occurred. In a evaluation of thirteen intracranial mycotic aneurysms,827 6 of eight sufferers who obtained therapy with antibiotics alone died; no deaths had been noticed in the surgical treatment group. In a review of eighty five circumstances handled between 1954 and 1978, 20 of 38 patients managed solely with antibiotics died, in contrast with eight of 30 sufferers who underwent surgery. The mortality rate was low (4 of 15) in patients with multiple aneurysms who received remedy with antibiotics alone. In one sequence, the mortality price was 29% after rupture of an intracranial mycotic aneurysm. The most essential issue in the management of intracranial mycotic aneurysms is whether rupture is present. If rupture was current, nonetheless, surgical or endovascular therapy appeared to be indicated, as a outcome of the result of medically managed sufferers was poor. Based on these data, most authorities advise a conservative strategy if the intracranial mycotic aneurysm is unruptured. Other factors influencing therapy selections for intracranial mycotic aneurysms embrace aneurysm location, presence of increased intracranial strain, and the extent of perfusion equipped by the affected artery. The definitive remedy for aneurysms which may be decreasing in measurement on serial angiographic studies repeated every 2 weeks is unclear. Therapy with antibiotics, proximal ligation of the vessel, resection of the pseudoaneurysm, and acceptable drainage leads to cures in 75% of the cases. Vascular reconstruction through uninfected tissue planes with autogenous grafts is important if limb viability is determined by the affected vessel. Severe ischemia developed in 9 of 28 sufferers after excision of mycotic aneurysms of the common femoral artery in a single collection of fifty two instances. Survival after surgical procedure also is extra widespread (75%) for sufferers with aneurysms contaminated with gram-positive cocci than for patients with gram-negative bacilli (25%). Antibiotics must be used on this illness, nevertheless, even if the lesion is sterilized (reported in only three cases). At surgical procedure, the aneurysm and any intraluminal thrombus should be sectioned and Gram stain carried out, and specimens must be submitted for tradition. If an infection is current, all aneurysmal tissue and surrounding areas of irritation must be resected before grafting. Basic principles of grafting in this situation embrace using autogenous quite than synthetic grafts and insertion solely in clean, noninfected tissue planes. If the graft is positioned within the contaminated space, continued an infection, leakage, thrombus formation, abscess formation, or rupture usually outcomes. Nevertheless, the kind of reconstruction have to be individualized, as a end result of outcomes of in situ repair appear to be higher for suprarenal912�915 than for extra distal aortic aneurysms if reconstruction is combined with extended programs of intravenously administered antimicrobial agents. Radical resection of intraabdominal aortic aneurysms with out prosthetic materials also has been utilized in a few instances. If a graft is inserted in situ and persistent fever with bacteremia or embolism within the decrease extremities ensues, reoperation with extraanatomic grafting is necessary. Because the resected space is contaminated, particular bypass techniques-especially for thoracoiliac, transpubic, and axillofemoral bypass-usually are required. If an axillofemoral method is used, a single graft must be inserted for both lower extremities, because patency is extended beneath these circumstances. The choice of agents is dependent upon the isolated organism (or the morphologic traits of the organisms in the surgical specimen) and on the results of in vitro susceptibility testing. Implantation of antibiotic-releasing carriers with in situ reconstruction has been used,917 but only in a couple of patients with out managed trials; use of such carriers stays of unproved benefit in remedy for mycotic aneurysm. Infective endocarditis: diagnosis, antimicrobial therapy, and administration of problems: a scientific statement for healthcare professionals from the American Heart Association. Regional variation within the presentation and outcome of sufferers with infective endocarditis. Healthcare-associated native valve endocarditis: significance of non-nosocomial acquisition. Clinical characteristics and consequence of infective endocarditis in adults with bicuspid aortic valves: a multicentre observational examine. A guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease within the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Cerebrovascular issues in sufferers with left-sided infective endocarditis are common: a potential research using magnetic resonance imaging and neurochemical mind injury markers. Association between valvular surgical procedure and mortality amongst sufferers with infective endocarditis sophisticated by coronary heart failure. Neurologic manifestations of infective endocarditis: a 17-year experience in a instructing hospital in Finland. Positron emission tomography/computed tomography for prognosis of prosthetic valve endocarditis: elevated valvular 18 F-fluorodeoxyglucose uptake as a novel major criterion. Utility of extended blood tradition incubation for isolation of Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, and Kingella organisms: a retrospective multicenter analysis. Proposed modifications to the Duke criteria for the analysis of infective endocarditis. Native valve endocarditis due to coagulase unfavorable staphylococcus: scientific significance and predictors of mortality. Analysis of the impact of early surgery on in-hospital mortality of native valve endocarditis: use of propensity score and instrumental variable methods to modify for treatment-selection bias. Right-sided Staphylococcus aureus endocarditis in intravenous drug abusers: two week mixture therapy. Antibiotic selection could not clarify poorer outcomes in sufferers with Staphylococcus aureus bacteremia and high vancomycin minimum inhibitory concentrations. High rate of decreasing daptomycin susceptibility through the remedy of persistent Staphylococcus aureus bacteremia. Staphylococcus aureus endocarditis at a neighborhood instructing hospital, 1980 to 1991: an evaluation of 106 circumstances. Epidemiological and microbiological characterization of infections attributable to Staphylococcus aureus with reduced susceptibility to vancomycin, United States, 1997-2001. Infection with vancomycin-resistant Staphylococcus aureus containing the vanA resistance gene. Candida infective endocarditis: an observational cohort research with a focus Chapter 80 Endocarditis and Intravascular Infections 336. Complicated left-sided native valve endocarditis in adults: danger classification for mortality. Suppurative pelvic thrombophlebitis: a examine of 202 instances by which the disease was treated by ligation of the vena cava and ovarian vein. Influence of referral bias on the obvious scientific spectrum of infective endocarditis. Global and regional burden of infective endocarditis, 1990-2010: a systematic evaluation of the literature. Current features of infective endocarditis within the elderly: outcomes of the International Collaboration on Endocarditis Prospective Cohort Study. Hospital-acquired infectious endocarditis not related to cardiac surgical procedure: an emerging problem. Healthcareassociated native valve endocarditis: significance of non-nosocomial acquisition. Active surveillance for rheumatic heart illness in endemic areas: a scientific review and meta-analysis of prevalence amongst youngsters and adolescents. Global, regional, and national incidence, prevalence, and years lived with incapacity for 328 illnesses and injuries for 195 nations, 1990�2016: a scientific evaluation for the Global Burden of Disease Study 2016. Prospective comparability of infective endocarditis in Khon Kaen, Thailand and Rennes, France. Bicuspid aortic valve-a silent danger: analysis of fifty instances of infective endocarditis. Bacterial endocarditis in patients with aortic stenosis, pulmonary stenosis, or ventricular septal defect. Calcification of the mitral annulus: etiology, medical associations, problems and remedy. Increasing rates of cardiac system infections amongst Medicare beneficiaries: 1990-1999. Clinical options and modifications in epidemiology of infective endocarditis on pacemaker devices over a 27-year period (1987-2013). Recurrent infective endocarditis: analysis of predisposing factors and scientific features. Infectious endocarditis in idiopathic hypertrophic subaortic stenosis: report of three cases and evaluation of the literature. Incidence and predictors of infective endocarditis in mitral valve prolapse: a population-based study. A controlled evaluation of the danger of bacterial endocarditis in individuals with mitral-valve prolapse. Infective endocarditis and mitral prolapse: a comparison with different kinds of endocarditis. Pathoanatomic, pathophysiologic, and clinical correlations in endocarditis (first of two parts). Scanning electron microscopic observations of the surface of the preliminary lesion in experimental streptococcal endocarditis in the rabbit. Experimental staphylococcal endocarditis and aortitis: morphology of the initial colonization. Nonbacterial thrombotic endocarditis in a Japanese autopsy sample: a review of eighty circumstances. Cardiac valvular vegetations in cancer sufferers: a prospective echocardiographic research of 200 patients. The presence of infection-related antiphospholipid antibodies in infective endocarditis determines a major risk factor for embolic events. On the relation between the site of valvular involvement in endocarditis and the blood strain resting on the valve. Bacteraemia and oral sepsis: with special reference to the aetiology of subacute endocarditis. Periodontal well being status and bacteraemia from day by day oral actions: systematic review/meta-analysis. Experimental Escherichia coli endocarditis in rats: roles of serum bactericidal activity and duration of catheter placement. Potential associations between virulence and bacterial genotype in Staphylococcus aureus. Methicillin-susceptible Staphylococcus aureus endocarditis isolates are associated with clonal complex 30 genotype and a distinct repertoire of enterotoxins and adhesins. An association between bacterial genotype combined with a high-vancomycin minimal inhibitory focus and risk of endocarditis in methicillin-resistant Staphylococcus aureus bloodstream an infection. Staphylococcus aureus microcapsule expression attenuates bacterial virulence in a rat mannequin of experimental endocarditis. Association between Staphylococcus aureus strains carrying gene for Panton-Valentine leukocidin and extremely lethal necrotising pneumonia in young immunocompetent sufferers. Relationships between Staphylococcus aureus genetic background, virulence elements, agr teams (alleles), and human disease. Potential associations between severity of an infection and the presence of virulence-associated genes in scientific strains of Staphylococcus aureus. Synthesis of insoluble dextran and its significance within the formation of gelatinous deposits by plaque-forming streptococci. Bacterial adherence in the pathogenesis of endocarditis: interplay of bacterial dextran, platelets, and fibrin. Adherence of glucan-positive and glucan-negative streptococcal strains to normal and damaged heart valves. Effects of molecular weight of dextran on the adherence of Streptococcus sanguis to damaged coronary heart valves. Enzymatic modification of the glycocalyx in experimental endocarditis because of viridans streptococci. Association of cell adherent glycocalyx and endocarditis manufacturing by viridans group streptococci. Comparative adhesion of seven species of streptococci isolated from the blood of patients with subacute bacterial endocarditis to fibrin-platelet clots in vitro. Clindamycin impact on glycocalyx production in experimental viridans streptococcal endocarditis. FimA, a serious virulence determinant associated with Streptococcus parasanguis endocarditis. Immunization with FimA protects in opposition to Streptococcus parasanguis endocarditis in rats.
Purchase modafinil 200 mg mastercard. Sleepyhead Sleep Aid - Walgreens.
Preoperative threat elements for mediastinitis after cardiac surgery: assessment of 2768 sufferers sleep aid amazon modafinil 100mg on-line. Nosocomial infections in adult cardiogenic shock sufferers supported by venoarterial extracorporeal membrane oxygenation insomnia korean version 100 mg modafinil mastercard. Bacterial mediastinitis after coronary heart transplant: scientific presentation insomnia craig david best 200mg modafinil, danger elements sleep aid for 9 year old discount modafinil 100mg with mastercard, and treatment insomnia definition proven modafinil 100mg. Incidence insomnia jet lag cheap modafinil amex, therapy strategies and end result of deep sternal wound an infection after orthotopic coronary heart transplantation. Impact of de novo everolimus-based immunosuppression on incisional problems in heart transplantation. Wound healing complications with de novo sirolimus versus mycophenolate mofetil-based routine in cardiac transplant recipients. Infections related to ventricular assist units: epidemiology and impact on prognosis after transplantation. Major an infection after pediatric cardiac surgery: exterior validation of threat estimation model. Risk elements and threat adjustment for surgical web site infections in pediatric cardiothoracic surgery sufferers. Delayed sternal closure after pediatric cardiac operations; single center experience: a retrospective research. Postoperative mediastinitis in youngsters: epidemiology, microbiology, and threat factors for gram-negative pathogens. A hospital-acquired outbreak of methicillin-resistant Staphylococcus aureus infection initiated by a surgeon carrier. The relationship between the nasalstaphylococcal-carrier state and the incidence of postoperative problems. Alteration of staphylococcal flora in cardiac surgical procedure sufferers receiving antibiotic prophylaxis. Coagulasenegative staphylococci isolated from sternal wound infections after cardiac surgery: attachment to and accumulation on sternal fixation stainless steel wires. Risk elements for postoperative mediastinitis as a result of methicillinresistant Staphylococcus aureus. Staphylococcus aureus poststernotomy mediastinitis: description of two distinct acquisition pathways with different potential preventive approaches. Multiply beta-lactam resistant Enterobacter cloacae infections linked to the environmental flora in a unit for cardiothoracic and vascular surgery. Outbreak of invasive aspergillosis after main coronary heart surgical procedure attributable to spores within the air of the intensive care unit. Effect of time to onset on medical options and prognosis of post-sternotomy mediastinitis. Mediastinitis after cardiac surgical procedure: enchancment of bacteriological prognosis by use of a number of tissue samples and pressure typing. Descending necrotizing mediastinitis: two case reports and evaluate of the literature. Critical care transesophageal endosonography and guided fine-needle aspiration for diagnosis and management of posterior mediastinitis. Perforation of the esophagus: correlation of website and trigger with plain movie findings. Low mortality after therapy for esophageal perforation: a single-center experience. Diagnostic value and prognostic implications of serum procalcitonin after cardiac surgical procedure: a systematic evaluate of the literature. Procalcitonin for differential analysis of graft rejection and infection in patients with coronary heart and/or lung grafts. Accuracy of blood tradition for early diagnosis of mediastinitis in febrile sufferers after cardiac surgery. Detection of mediastinitis after heart transplantation by gallium-67 scintigraphy. Diagnosing sternal wound infections with 99mTc-labeled monoclonal granulocyte antibody scintigraphy. Role of epicardial pacing wire cultures in the prognosis of poststernotomy mediastinitis. Usefulness of routine epicardial pacing wire culture for early prediction of poststernotomy mediastinitis. Report of a case of spontaneous perforation of the oesophagus efficiently treated by operation. Management of esophageal perforation in one hundred twenty consecutive sufferers: clinical influence of a structured treatment algorithm. Endoscopic clips for closing esophageal perforations: case report and pooled evaluation. Systematic evaluate: temporary stent placement for benign rupture or anastomotic leak of the oesophagus. A propensitymatched comparability of price and outcomes after esophageal stent placement or primary surgical repair for iatrongenic esophageal perforation. Conservative approach to the mediastinitis in childhood secondary to esophageal perforation. Transcervical drainage for descending necrotizing mediastinitis could additionally be adequate. Descending necrotizing mediastinitis: up to date tendencies in etiology, prognosis, management, and outcome. Clinical features and outcome of sufferers with descending necrotizing mediastinitis: potential analysis of 34 circumstances. Descending necrotizing mediastinitis: a minimally invasive method using video-assisted thoracoscopic surgery. Nonoperative catheter management for cervical necrotizing fasciitis with and with out descending necrotizing mediastinitis. Vacuum assisted closure for the remedy of sternal wounds: the bridge between debridement and definitive closure. Vacuum-assisted closure for sternal wounds: a first-line therapeutic management method. Clinical consequence after poststernotomy mediastinitis: vacuum-assisted closure versus standard therapy. Negative stress remedy for post-sternotomy mediastinitis reduces mortality rate and sternal re-infection price compared to typical treatment. Should vacuum-assisted closure therapy be routinely used for administration of deep sternal wound an infection after cardiac surgical procedure Primary therapy of the infected sternotomy wound with muscle flaps: a review of 211 consecutive instances. Omental flap for recurrent deep sternal wound an infection and mediastinitis after cardiac surgical procedure. Intercostal artery-based rectus abdominis transposition flap for sternal wound reconstruction. Two-stage management of sternal wound an infection utilizing bilateral pectoralis major advancement flap. Gentamicin resolution for mediastinal irrigation: systemic absorption, bactericidal activity, and toxicity. Iodine toxicity in a affected person handled by steady povidoneiodine mediastinal irrigation. Poststernotomy mediastinitis because of Staphylococcus aureus: comparability of methicillin-resistant and methicillin-susceptible cases. The impression of methicillin resistance on the finish result of poststernotomy mediastinitis as a end result of Staphylococcus aureus. Methicillin resistant Staphylococcus aureus infections following cardiac surgery: incidence, influence, and figuring out antagonistic consequence traits. Preventing mediastinitis surgical web site infections: government abstract of the association for professionals in infection management and epidemiology elimination information. Continuous intravenous insulin infusion reduces the incidence of deep sternal wound an infection in diabetic sufferers after cardiac surgical procedures. Comparative examine of cefazolin, cefamandole, and vancomycin for surgical prophylaxis in cardiac and vascular operations. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. Perioperative intranasal mupirocin for the prevention of surgical-site infections: systematic review of the literature and meta-analysis. Safety of targeted perioperative mupirocin therapy for preventing infections after cardiac surgical procedure. Effect of an investigational vaccine for preventing Staphylococcus aureus infections after cardiothoracic surgery: a randomized trial. Vancomycin paste doe not cut back the incidence of deep sternal wound infection after cardiac operations. Meta-analysis to assess the effectiveness of topically used vancomycin in reducing sternal wound infections after cardiac surgical procedure. Prophylaxis of sternal wound infections with gentamicin-collagen implant: randomized controlled study in cardiac surgical procedure. Local gentamicin reduces sternal wound infections after cardiac surgery: a randomized managed trial. Gentamicincollagen sponge reduces wound complications after heart surgical procedure: a managed, prospectively randomized double-blind research. Gentamicin collagen sponges for the prevention of sternal wound infection: a meta-analysis of randomized controlled trials. Management of closed sternal incision after bilateral inside thoracic artery grafting with a single-use unfavorable stress system. Prevention of poststernotomy wound infections in overweight sufferers by unfavorable pressure wound therapy. Management and outcomes of esophageal perforations: a national research of two,264 sufferers in England. Current treatment and end result of esophageal perforations in adults: systematic evaluation and meta-analysis of 75 research. Management of esophageal perforation within the endoscopic era: is operative repair nonetheless related Diffuse descending necrotizing mediastinitis: surgical therapy and outcome in a single-centre series. Deep sternal wound infection after cardiac surgery: modality of therapy and consequence. Incidence and morbidity of cytomegaloviral an infection in sufferers with mediastinitis following cardiac surgery. Evaluation of risk elements for hospital mortality and current treatment for poststernotomy mediastinitis. Fibrosing mediastinitis: scientific presentation, therapeutic outcomes, and adaptive immune response. Granulomatous mediastinitis due to Aspergillus flavus in a nonimmunocompromised patient. Idiopathic fibroinflammatory (fibrosing/sclerosing) lesions of the mediastinum: a study of 30 cases with emphasis on morphological heterogeneity. Idiopathic retroperitoneal fibrosis, inflammatory aortic aneurysm, and inflammatory pericarditis-retrospective evaluation of 11 case histories. Idiopathic mediastinitis with superior vena cava obstruction, cardiac tamponade, and cutaneous vasculitis. Sclerosing mediastinitis: improved administration with histoplasmosis titer and ketoconazole. Successful remedy of sclerosing cervicitis and fibrosing mediastinitis with tamoxifen. Catheter-based intervention for pulmonary vein stenosis due to fibrosing mediastinitis: the Mayo Clinic expertise. The commonest etiology is idiopathic, but tuberculous meningitis and fungal meningitis. Other fungi, such as Candida and Aspergillus, are uncommon causes of meningitis, although instances of Exserohilum rostratum meningitis have been reported in affiliation with epidural or paraspinal glucocorticoid injections of preservative-free methylprednisolone from a single compounding pharmacy. The major standards are altered psychological standing (defined as a decreased, altered stage of consciousness, lethargy, or personality change) lasting 24 hours with out an alternate diagnosis and is a requirement for the diagnosis. A clinical overlap between encephalitis and encephalopathy could exist, the latter referring to a medical state of altered mental standing that can manifest as confusion, disorientation, or other cognitive impairment, with or without evidence of brain tissue inflammation; encephalopathy may be triggered by a variety of metabolic or toxic circumstances however often happens in response to sure infectious agents, such as Bartonella henselae and influenza virus. Patients with acute meningitis most often present with fever, headache, meningismus, and altered psychological status (see Chapter 87). In distinction, patients with subacute (>5 days however <30 days of symptoms) or continual meningitis (>30 days of symptoms) usually present over weeks to months, and even years (see Chapter 88). Louis, La Crosse, and Japanese encephalitis viruses) and respiratory viruses can current with a thalamic and basal ganglia encephalitis presenting with tremors, together with Parkinsonism features. These latter syndromes are presumed to be mediated by an immunologic response to an antecedent antigenic stimulus provided by the infecting microorganism or immunization. After needle insertion, frequent removal of the stylet can determine whether the subarachnoid space has been entered. At that point a "pop" is felt, indicating penetration of the needle throughout the ligamentum flavum. The commonest complication after lumbar puncture is headache, which is generally observed in 10% to 25% of sufferers; the headache is characteristically absent when the affected person is recumbent and seems quickly when the patient stands.
In the primary insomnia 6 dpo generic modafinil 200mg on line, a synergistic combination of organisms converges by likelihood to type a single abscess insomnia nursing diagnosis purchase modafinil uk, and in the second quinine sleep aid order modafinil 100 mg online, a highly pathogenic organism types abscesses wherever it was seeded insomnia wikipedia purchase generic modafinil on-line. The latter has been increasingly recognized as a cause of community-acquired monomicrobial liver abscesses (discussed later) sleep aid linked to alzheimers buy generic modafinil 200mg on-line. Enterococci and viridans-group streptococci are additionally widespread insomnia zoloft cheap modafinil 100mg without a prescription, primarily in polymicrobial abscesses. Staphylococcus aureus, against this, is more generally associated with monomicrobial abscesses. Cough Jaundice Right higher quadrant tenderness Laboratory Tests (Approximate % of Cases) Leukocytosis Elevated alkaline phosphatase Solitary lesion 80 80 70 seventy five sixty five 70 infections corresponding to meningitis and endophthalmitis happen in 10% to 16% of all instances. Mutagenesis of 1 cps gene, magA (for mucoviscosity-associated gene A), abolishes hypermucoviscosity, will increase sensitivity to phagocytosis and serum-mediated lysis, and reduces virulence in mice. Only 15% to 35% of sufferers present with concurrent gastrointestinal signs, together with nausea, vomiting, stomach cramping, and diarrhea (Table seventy five. Corticosteroid use and male intercourse are well-established risk components for invasive amebic disease. Only 1 patient in 10 presents with the classic triad of fever, jaundice, and proper upper quadrant tenderness. Fever is common, typically with out localizing signs however only with a common failure to thrive, including malaise, 1040 fatigue, anorexia, or weight loss (see Table 75. The duration of signs before presentation varied widely in most case collection, and there was seldom settlement on a median period. Butler and McCarthy48 tried to tackle this issue by stratifying in accordance with acute and chronic shows. They found the previous to be typically related to acute, identifiable belly pathology such as cholangitis or appendicitis, whereas abscesses that offered chronically have been usually cryptogenic. For instance, Seeto and Rockey61 discovered that hematogenous liver abscesses presented most acutely (3 days), and those secondary to pylephlebitis had the longest period of symptoms (42 days). The prognosis of liver abscess must be suspected in all patients with fever, leukocytosis, and a space-occupying liver lesion. Because of the nonspecific symptoms on presentation, the initial scientific impression is regularly incorrect and will embody cholangitis, pneumonia, hepatic malignancy, intraabdominal disaster, or pneumonia. Leukocytosis is present in most sufferers; current studies69,70,73�75,77,114,one hundred fifteen report leukocytosis in 68% to 88% of all patients, with mean white blood cell counts of 15,000 to 17,000/mm. Abnormalities of alanine aminotransferase, aspartate aminotransferase, and bilirubin are usually small, although they may be more pronounced in some sufferers with biliary illness. Chest radiographs are abnormal about half of the time however are of no actual worth in making the diagnosis. Laboratory abnormalities could additionally be of prognostic significance, more than likely as markers of comorbidities. A multivariate analysis of danger factors found that a hemoglobin focus of less than 10 g/dL and a blood urea nitrogen concentration higher than 28 mg/dL had been unbiased predictors of mortality in sufferers found to have pyogenic liver abscess (odds ratios of thirteen and 14, respectively). Ultrasonography is the study of choice in sufferers with suspected biliary illness and in those who must avoid intravenous distinction or radiation publicity; it has a sensitivity of 70% to 90%. In sufferers with pyogenic liver abscess, blood cultures are constructive about half of the time. Failure to obtain the anticipated pus should immediate a reevaluation of the differential diagnosis, considering liver cyst, malignancy, and amebic liver abscess. Purulent materials should at all times be sent for Gram stain, which may present the only clue to a combined an infection in sufferers heavily handled with antibiotics. A Spanish research discovered that age forty five or youthful, presence of diarrhea, and a solitary proper lobar abscess favored amebic etiology. Serum amebic serology by enzyme immunoassay has a sensitivity of about 95% and is extremely particular for E. Examination of aspirated liver abscess pus can be not beneficial, on situation that trophozoites are identified in only 11% to 25% of circumstances. Bacterial superinfection of amebic liver abscess has been described in about 1% to 5% of cases, incessantly as a complication of drainage procedures. Decreased fever and belly pain are often observed inside 3 to 5 days after initiation of therapy. Drainage must also be thought of for giant lesions in danger for rupture, particularly left-sided abscesses that may rupture into the 1041 pericardium. Meticulous dealing with of the specimen and rapid transportation to a qualified laboratory are important for environment friendly restoration of anaerobes. Depending on host and epidemiologic components, microbiologic analysis for fungi, mycobacteria, and E. The catheter is normally left in place until drainage becomes minimal, typically 5 to 14 days. Recent studies suggest that the success fee for percutaneous drainage with antibiotic remedy is roughly 80% to 95%, even for large (>10 cm) pyogenic liver abscesses. Both investigations discovered that reaspiration was required in about 50% of cases, and a minority of sufferers required three or extra aspiration procedures. Attempts to deal with pyogenic liver abscess with antibiotics but no drainage have met with some success. Two early research with a mixed complete of 25 sufferers discovered remedy charges of 87% to 90%. Moreover, this success rate was substantially larger than the traditional experience on the time, when undrained abscesses carried a mortality fee of 60% to 100%. Even severely debilitated patients can tolerate percutaneous drainage, however the procedure may not all the time be required for remedy: success charges of 44% and one hundred pc with medical therapy alone have been reported in small case series. Treatment with empirical antibiotics should start as quickly as the diagnosis of pyogenic liver abscess is suspected. Antibiotic alternative should be guided by the suspected supply of the abscess (Table 75. Abscesses arising from a biliary source incessantly involve enterococci and enteric gram-negative bacilli, whereas abscesses from a colonic or pelvic source are extra commonly brought on by enteric gram-negative bacilli and anaerobes. Metronidazole at appropriately high doses should be included if amebic liver abscess is a consideration. Fluoroquinolones could also be substituted for gentamicin, but this is in all probability not advisable in cases complicated by enterococcal bacteremia. If a hematogenous (hepatic artery) source is suspected, coverage should embrace an antibiotic with activity against S. Pyogenic liver abscesses are often treated parenterally for two to 3 weeks, and a 4- to 6-week whole course is accomplished with oral brokers. Some have reported successful remedy with lower than 2 weeks of antibiotic therapy. One-third of sufferers are readmitted or have emergency room visits following discharge from the hospital, which suggests that these individuals could benefit from shut outpatient follow-up and a multidisciplinary method to care. Surgical drainage was traditionally the therapy of selection and, in the preantibiotic era, the only hope for treatment. As early as 1953, McFadzean and associates144 reported the utilization of percutaneous drainage with antibiotic remedy to deal with 14 sufferers with liver abscess. Surgical intervention must be thought-about if percutaneous drainage fails or administration of concurrent intraabdominal illness is required, and in addition for some sufferers with a quantity of giant or loculated abscesses. The lesion was aspirated beneath radiologic guidance, and more than 500 mL of frank pus had been drained. A radiodense percutaneous drainage catheter was left in place (B), and the affected person was handled with intravenous antibiotics and continued drainage. Recurrent symptoms corresponding to fever or abdominal pain ought to immediate repeat imaging and potential reaspiration. Impaction of a gallstone leads to obstruction of the cystic duct and elevated intraluminal pressure. In the United States and tons of developed international locations, gallstones are frequent and most frequently asymptomatic. Approximately one hundred twenty,000 cholecystectomies are performed every year in the United States for acute cholecystitis, mostly secondary to impacted gallstones. Stasis of bile, irritation, and lack of mechanical limitations can lead to bacterial an infection of the bile, which can result in severe morbidity and demise. Cholangitis Only about 20% of patients with gallstones expertise biliary colic, typified by proper upper quadrant pain after a fatty meal when the contracting gallbladder is prevented from emptying by an obstructing stone. In this illness, biliary obstruction is accompanied by an intense inflammatory reaction. Obstruction is assumed to lead to elevated intraluminal stress; may result in compromised blood provide and lymphatic drainage; and, in the setting of supersaturated bile, leads to acute irritation. In a microbiologic study of biliary tract processes, 46% of patients presenting with acute cholecystitis had positive bile cultures, in comparison with 22% of sufferers with symptomatic gallstones however no evidence of acute cholecystitis and no constructive cultures in normal controls. Once an infection is established, issues embody gangrenous cholecystitis, emphysematous cholecystitis, gallbladder empyema, pyogenic liver abscess (discussed earlier), and bacteremia. Pathogenesis Cholecystitis Cholangitis refers to irritation or infection of the common bile duct. The normally sterile bile might become contaminated due to the loss of protecting components, including the circulate of bile. Obstruction of the frequent bile duct leads to stasis, which favors the expansion of bacteria; elevated stress predisposes to bacteremia. Other factors could contain the lack of antibacterial activity of bile on the proximal small intestine, permitting for higher growth of micro organism. Bacteria may then ascend to the biliary tract (hence the terms ascending and suppurative cholangitis). Other routes of an infection have been proposed, including through the portal system or the lymphatics. Anastomosis of the bile duct to the small intestine, such as in a Whipple procedure, can result in cholangitis. Patients with biliary tract illness most often current with ache in the best higher quadrant of the abdomen, although occasionally localizing findings are absent. Cholecystitis and cholangitis are distinguished from easy biliary colic by the continual nature of the pain. The finding of tenderness in the right higher quadrant on bodily examination and the presence of the Murphy sign (inhibition of inspiration by ache when the area of the gallbladder fossa is palpated), with or without a mass, are extremely suggestive of biliary tract illness. Complications of acute cholecystitis, which occur in 10% to 15% of cases, include hepatic or intraabdominal abscess, necrosis or gangrene of the gallbladder, and perforation, which in flip lead to sepsis and peritonitis. Emphysematous cholecystitis, normally recognized radiologically, happens when the wall of the gallbladder is infected with gas-forming organisms, together with Clostridia, in addition to cardio and facultative gram-negative and gram-positive micro organism. Clinical Manifestations Acalculous Cholecystitis In 2% to 15% of cases, cholecystitis occurs within the absence of gallstones, although normally in the presence of other predisposing situations. These 1043 Acute or ascending cholangitis is suggested by the Charcot triad (right higher quadrant or epigastric abdominal ache; fever or chills, or both; and jaundice), reported in 50% to 70% of sufferers. Leukocytosis with a left shift is probably the most frequent laboratory abnormality in acute cholecystitis. However, in a single study of 217 sufferers with acute cholecystitis, 25% of sufferers without obstruction of the common bile duct had elevated bilirubin. The mechanism underlying these abnormalities is unclear however may be the passage of small stones or sludge through the common bile duct. International consensus follow pointers (the "Tokyo Guidelines") advocate acquiring bile and, when obtainable, tissue cultures from sufferers with cholangitis or moderate-to-severe acute cholecystitis. Abnormalities suggestive of sepsis syndrome, together with leukocytosis, are incessantly noticed. Additional laboratory abnormalities embody cholestatic liver operate tests with elevations in alkaline phosphatase and bilirubin, significantly conjugated bilirubin. Abnormal amylase might counsel an related pancreatitis, and elevations in transaminases might indicate associated irritation or infection of the liver parenchyma, or each. The Tokyo pointers suggest obtaining aerobic and anaerobic cultures of bile aspirates and blood in circumstances of acute cholangitis. In addition, the testing may be accomplished on the bedside of critically sick sufferers, is relatively inexpensive, and may directly visualize stones, notably within the gallbladder. A technetium 99m (99mTc)�labeled derivative of acetanilide iminodiacetic acid is injected intravenously and is secreted into the bile. Failure of the gallbladder to accumulate the marker is extremely suggestive of acute cholecystitis because of obstruction of the cystic duct. Normally, visualization of the widespread bile duct and small bowel happens within 30 to 60 minutes; failure to visualize these structures indicates obstruction throughout the frequent bile duct or on the ampulla. Ultrasonographic visualization of the gallbladder (sagittal view) in a case of acalculous cholecystitis, demonstrating mural thickening and hypoechoic areas inside the gallbladder wall. Bacterial cultures from the bile and surgical websites of sufferers with acute cholecystitis and acute cholangitis sometimes yield constituents of the conventional intestinal microbiota (Table seventy five. Addition of metronidazole is important because of increasing resistance of Bacteroides to fluoroquinolones other than moxifloxacin. Local antimicrobial susceptibility profiles and, if out there, isolate susceptibility should be reviewed because of increasing resistance of Escherichia coli to fluoroquinolones. Tokyo Guidelines 2018: antimicrobial remedy for acute cholangitis and cholecystitis. Clonorchis and Opisthorchis an infection can lead to the event of carcinoma of the biliary tract. Ascaris lumbricoides, a extra cosmopolitan parasite, occasionally obstructs the biliary tree, resulting in acute cholangitis. Diagnosis is often made by attribute findings on ultrasound, with dilatation of the common bile duct observed in roughly two-thirds of instances. Guidelines advocate a complete of four to 7 days of therapy as soon as supply management is obtained and anatomic points have been addressed, although longer programs of remedy could also be essential for problems corresponding to pyogenic liver abscess. However, enterococci may be necessary pathogens in high-risk sufferers, corresponding to liver transplant recipients; in these cases, treatment that also targets enterococci may be indicated. Alternatively, in unstable sufferers, cholecystotomy (percutaneous drainage of the biliary system with removing of obstructing stones) may be carried out as a temporizing measure. In the absence of extreme issues, the timing of definitive surgical intervention within the administration of acute cholecystitis is the subject of Acute Cholecystitis 1045 some debate.