Mark K. Wax, MD, FACS, FRCSC
- Professor, Otolaryngology/Head and Neck Surgery
- Professor, Oral and Maxillofacial Surgery
- Program Director
- Director, Microvascular Reconstruction
- Coordinator, Education, AAOHNS(F)
- Department of Otolaryngology/Head and Neck Surgery
- Oregon Health Sciences University
- Portland, Oregon
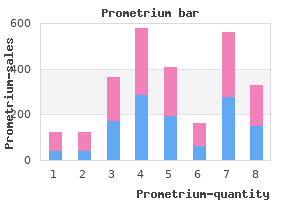
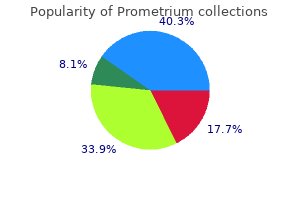
The onset of respiratory depression after neuraxial opioids is variable and has been reported to range from 2 to 12 hours medications 1-z 100 mg prometrium overnight delivery. Older antiemetics treatment xerostomia cheap 100mg prometrium amex, similar to metoclopramide and droperidol symptoms queasy stomach and headache buy 100 mg prometrium, have been used to prevent or deal with neuraxial opioid�induced emesis in the obstetric setting medications and grapefruit interactions buy prometrium 100mg. Distribution of nausea and emesis episodes (0 [nausea or emesis free] or 1 or less) within the first 24 hours symptoms 8 days past ovulation purchase prometrium 200 mg on-line. Administration of medication performing at two totally different receptor websites may enhance antiemetic efficacy via additivity or synergism treatment for vertigo buy prometrium 100mg with visa. Spinal anesthesia�induced hypotension was managed prophylactically with a phenylephrine infusion to maintain the systolic blood strain inside 20% of baseline or larger than ninety mm Hg. Several studies have investigated the prophylactic use of acupressure (using wrist Pruritus Pruritus is a standard side effect of neuraxial opioid administration in obstetric patients. In a retrospective evaluate of 4880 patients undergoing cesarean supply who received epidural morphine 2 to 5 mg, pruritus was reported by 58% of sufferers. Plasma opioid and histamine ranges are clinically insignificant at the time of symptom presentation (3 to 6 hours after intraspinal morphine administration). Studies evaluating opioid antagonists for the therapy of pruritus have demonstrated mixed results. Nalbuphine (5 mg) significantly reduced the severity of pruritus after epidural morphine, and fewer sufferers required additional therapy of persistent pruritus. Prophylactic treatment with opioid antagonists has additionally been investigated as a method of lowering the incidence of opioid-induced pruritus. However, naloxone and nalbuphine administered via patient-controlled bolus doses with a steady background infusion have been found to scale back the incidence of pruritus after cesarean supply in sufferers who received epidural morphine 5 mg. Women present process elective cesarean delivery under spinal anesthesia with intrathecal morphine zero. Pentazocine, a -opioid receptor agonist and partial �-opioid receptor agonist, could also be a helpful drug for treating opioid-induced pruritus. Pentazocine reduced the general incidence of pruritus throughout the first 24 hours in contrast with saline. However, the length of analgesia was shorter amongst patients within the nalbuphine groups. Propofol has been reported to relieve pruritus caused by neuraxial opioids in nonobstetric patients after a single 10-mg bolus dose344 and after a 10-mg bolus dose followed by a 30 mg/24 h infusion. The antipruritic results related to ondansetron might depend upon the dose, lipophilicity, and period of action of the intrathecal opioid. In one research, ondansetron 4 mg had a excessive fee of success for the therapy of moderate-to-severe pruritus in contrast with placebo (80% and 36%, respectively). Differences in examine methodology and antihistamineinduced sedation could clarify the inconsistent antipruritic effect of diphenhydramine observed in these research. To keep away from impairment of bladder/detrusor operate, urinary catheterization must be thought-about if voiding has not occurred inside 6 hours. Neuraxial Nonopioid Analgesic Adjuvants the addition of neuraxial nonopioid adjuvants to native anesthetic agents might enhance the quality of each intraoperative anesthesia and postcesarean analgesia. Nonopioid neuraxial adjuvants have totally different sites and mechanisms of actions, and interactions between neuraxial opioids and nonopioid adjuvants could additionally be additive or synergistic. Potential benefits of neuraxial drug combos include a discount in dose of particular person drugs (with subsequent reductions in dosedependent aspect effects), particularly a reduction in postoperative opioid requirements and opioid-related side effects. Both opioids caused dose-dependent decreases in detrusor contractility and the urgency to void. Volunteers receiving intrathecal sufentanil had earlier recovery of decrease urinary tract function than those receiving intrathecal morphine. Not surprisingly given the longer length of motion, problem in micturition and want for bladder catheterization have been larger in the morphine group (58%) compared with the methadone group (3%). In a study of male volunteers, naloxone reversed the influence of neuraxial morphine on urodynamic function. Epidural and intrathecal alpha2-adrenergic receptor agonists provide analgesia by activating the descending noradrenergic system. Clonidine additionally potentiates sensory and motor block when administered with epidural local anesthetics and acts additively or synergistically with intraspinal opioids. They observed shortlived, dose-dependent analgesia and sedation, and prolonged motor block, which could lead to delays within the discharge of sufferers from the postanesthesia care unit. An isobolographic analysis of epidural clonidine (in doses ranging from 50 to 400 �g) with fentanyl (15 to a hundred thirty five �g) demonstrated additivity however not synergism between clonidine and fentanyl in sufferers recovering from cesarean delivery. A variety of studies have evaluated the potential role of intrathecal clonidine for postcesarean analgesia. Early postoperative analgesia (for 1 to 2 hours) was improved in sufferers who obtained clonidine; however, no difference was present in 24-hour morphine consumption between the teams, likely reflecting the brief length of motion of a bolus dose of clonidine. Interaction studies of intrathecal opioids mixed with clonidine have investigated the contribution of each drug to analgesia and unwanted aspect effects. Patients who acquired the bupivacaine-clonidine-fentanyl combination reported less intraoperative pain and more prolonged postcesarean analgesia (time to first analgesia request 215 minutes) than those receiving bupivacaine-clonidine and bupivacaine alone (183 and 137 minutes, respectively). However, higher charges of pruritus and sedation had been reported for the bupivacaine-clonidine-fentanyl group. They concluded that the morphine-clonidine regimens provided optimum analgesia with decrease ache scores at relaxation and with coughing within the first 4 hours. The minimal effective intrathecal dose of clonidine was 30 to 60 �g combined with bupivacaine, fentanyl 15 �g, and morphine zero. However, a rise in intraoperative sedation was noticed in all teams receiving clonidine. The bupivacaine-clonidine 150-�g group had a smaller area of peri-incisional hyperalgesia and a lower incidence of hyperalgesia in contrast with the opposite examine teams. However, no between-group differences were observed in postoperative morphine consumption or in ache scores earlier than and after discharge. They evaluated outcomes associated to efficacy of clonidine as an intrathecal adjuvant, including period of analgesia and motor block. Clonidine prolonged the length of sensory block by 128 minutes and motor block by 45 minutes whereas also growing sedation in contrast with intrathecal blocks without clonidine. Eighteen studies had been included within the analysis (12 intrathecal administration, 6 epidural administration). In abstract, neuraxial clonidine may provide a small improvement in postcesarean analgesia in addition to that supplied by neuraxial morphine. Epidural clonidine (150 to 800 �g) may delay postcesarean analgesia when given in combination with epidural opioids. Intrathecal clonidine (75 to 450 �g) has modest efficacy and a comparatively quick period of action. Ongoing concern concerning the opposed side-effect profile of epidural and intrathecal clonidine-notably sedation and hypotension-limit the neuraxial administration of this agent in most patients present process cesarean delivery. In selected instances, the anesthesia provider could conclude that the potential benefits outweigh the dangers. Dexmedetomidine is a extremely selective alpha2-adrenergic receptor agonist that provides some analgesic results mediated at the spinal stage. Its systemic administration is widespread in anesthesia and important care; nevertheless, its use in peripheral nerve blocks and neuraxial anesthesia is off-label. Intrathecal dexmedetomidine supplied similar analgesia and fewer pruritus and shivering in contrast with morphine. A variety of medical studies have investigated epinephrine as a spinal or epidural adjunct. Similar prolongation of analgesia has been noticed when epinephrine (5 to 30 �g/mL) was combined with epidural diamorphine or sufentanil; however, the incidence of unwanted side effects (including vomiting that required treatment) was additionally elevated. Importantly, research of the addition of epidural epinephrine (5 �g/mL) to 2% lidocaine or zero. The addition of epinephrine 200 �g to hyperbaric spinal bupivacaine improved perioperative analgesia but was associated with a longer period of residual sensory and motor block. In distinction, plasma ranges of morphine were roughly 66% decrease in the epinephrine group than in the control group. The use of intrathecal epinephrine 200 �g does appear to improve neuraxial opioid analgesia however is associated with prolonged sensory and motor block. As each nicotinic and muscarinic receptors are essential to central and peripheral ache transmission, the resulting analgesia could additionally be attributable to central and/or peripheral alterations in pain modulation and transmission. Initial studies of intrathecal neostigmine in animals and human volunteers have demonstrated analgesic results with out neurotoxic effects. The investigators reported modest, short-lived, and doseindependent reductions in postoperative pain in the neostigmine groups. Data relating to the maternal and fetal security profile of epidural neostigmine are reassuring. Limited data exist relating to the position of neuraxial ketamine in the provision of postcesarean analgesia. In patients present process cesarean supply randomly assigned to receive intrathecal bupivacaine alone or in combination with S(+) ketamine zero. No published research have evaluated perioperative epidural ketamine administration in patients present process cesarean delivery. Studies investigating intrathecal or epidural magnesium have shown variable analgesic results after cesarean supply. They observed an general improve in the interval to first analgesic request (mean distinction of forty minutes after intrathecal administration and 110 minutes after epidural administration). However, only four trials assessed neurologic complications, and the authors concluded that there were not enough sufferers (n = 140) to consider the risk for neurologic issues. Intrathecal magnesium sulfate 50 mg extended the period of spinal anesthesia and improved postoperative analgesia in sufferers present process nonobstetric surgery with bupivacaine and fentanyl spinal anesthesia. However, extra research, including dose-response research and comparability with systemic administration, are needed to more formally assess the analgesic efficacy of epidural and intrathecal magnesium. Postoperative analgesia was longer in the midazolam group than within the management group (202 minutes and 358 minutes, respectively). It is unknown whether intrathecal midazolam has any benefit in contrast with intrathecal morphine or in addition to morphine. Several neuraxially administered medication have been shown to produce antinociceptive effects by altering calcium channel conductance in the spinal wire. Intrathecal gabapentin reduced incision-induced allodynia in rats,419,420 and epidural verapamil lowered postoperative opioid consumption after lower belly surgery. In addition, research assessing analgesic efficacy, unwanted aspect effects, and toxicity should show that these brokers lead to significant improvement over the neuraxial native anesthetic and opioid regimens at present used in clinical practice. In medical follow, the blocks are normally carried out utilizing ultrasonography to confirm right needle place and site of injection. Adenosine (and adenosine analogues) have been proposed to have antinociceptive activity related to activation of spinal adenosine A1 receptors. Several animal studies have investigated potassium channel activators (nicorandil, sildenafil) administered by the intrathecal414 or epidural415 route. A meta-analysis of research that assessed the scientific benefit and unwanted effects of intrathecal midazolam in obstetric and nonobstetric sufferers advised a positive pharmacologic profile. The transversus abdominis plane lies between the internal oblique and transversus abdominis muscles. Visualization of an elliptical distribution of the local anesthetic with well-defined margins provides evidence for the correct injection of the answer into the plane between the inner oblique and transversus abdominis muscles. A limitation of the meta-analysis was the significant heterogeneity among research. Presumably, paravertebral spread to the lumbar spinal nerves led to weak spot of the psoas and quadriceps muscular tissues. The addition of epinephrine to the local anesthetic solution decreases native anesthetic peak plasma concentration. The addition of ketorolac was associated with a lower in ache scores and opioid consumption, and decrease concentrations of inflammatory mediators had been collected from the wound. All sufferers received spinal anesthesia with bupivacaine and sufentanil, and a multiorifice catheter was inserted into the wound. The control group received saline intrathecally and thru the catheter, the morphine group obtained intrathecal morphine zero. Continuous wound infusion under the fascia has been proven to be simpler in decreasing postcesarean morphine consumption in contrast with infusion above the fascia. Although some centers use wound-infusion catheters, the additional value of the pump and a few minor inconveniences, similar to wound leakage, may have discouraged widespread use. Ilioinguinal-Iliohypogastric Block Ilioinguinal-iliohypogastric nerve block is beneficial for postoperative analgesia after decrease belly surgical procedure. Evidence is inconsistent as to whether ilioinguinaliliohypogastric blocks enhance analgesia supplied by neuraxial morphine. Pain scores were decrease within the sponge group in contrast with the management group, and fewer sufferers required rescue opioid. Wound infiltration lowered opioid consumption at 24 hours (morphine equivalent -9. Higher doses could improve opioid-related side effects with out enhancing analgesia. However, these adjuncts are associated with modest analgesic benefits, and the chance for spinal neurotoxicity associated with many of these medication remains to be decided. Adverse results associated with opioids, which frequently restrict their use, embody respiratory melancholy, sedation, constipation, nausea and vomiting, urinary retention, and pruritus. The rising development in caesarean part rates: global, regional and national estimates: 1990-2014. Postoperative pain experience: results from a national survey recommend postoperative ache continues to be undermanaged. Spread of subarachnoid block, intraoperative local anaesthetic necessities and postoperative analgesic requirements in caesarean part and whole abdominal hysterectomy. Pain: shifting from symptom control towards mechanism-specific pharmacologic administration. Local and systemic launch of cytokines, nerve progress issue, prostaglandin e2, and substance P in incisional wounds and serum following cesarean supply.
Determining the length of labor requires that investigators doc begin and finish times medicine world nashua nh prometrium 100 mg without prescription. The definition of the beginning time varies among research however is usually consistent between groups inside a research kerafill keratin treatment order prometrium 100 mg with mastercard. The finish of the first stage of labor is defined as the time of full (10 cm) cervical dilation symptoms 5 dpo cheap 200mg prometrium mastercard. Clinically medications bad for liver buy generic prometrium line, full cervical dilation is recognized when a cervical examination is performed as a outcome of the affected person complains of rectal stress medications vaginal dryness order prometrium uk. It is likely that women with effective epidural analgesia will complain of rectal pressure at a later time (and decrease fetal station) than women with systemic opioid analgesia medicine zocor buy prometrium in india. In other phrases, the patient could also be fully dilated for a major time earlier than cervical examination verifies full cervical dilation. This difference serves to artificially extend the duration of the primary stage of labor within the epidural group, although it shortens the apparent duration of the second stage of labor. Some clinicians have noted enhanced uterine activity in some patients for roughly half-hour after the initiation of neuraxial analgesia, whereas uterine activity appears to be lowered in different sufferers. Schellenberg466 instructed that aortocaval compression is responsible for the transient lower in uterine exercise that occurs after the administration of epidural analgesia in some sufferers. Because this organ also releases oxytocin, the manufacturing of that hormone may also be transiently suppressed; this potential lower in oxytocin launch could partially explain the transient adjustments in uterine contractility noticed in association with epidural analgesia. No significant distinction within the variety of contractions before and after epidural analgesia was noticed. There was greater intrauterine stress in the upper uterine section than within the decrease section (consistent with fundal dominance) each earlier than and after initiation of epidural analgesia. Further, fundal dominance was larger after epidural analgesia than in the preanalgesia period. Increased uterine activity after the initiation of neuraxial analgesia has been hypothesized to be an oblique impact of neuraxial analgesia (see later discussion). Some physicians have expressed concern that the epinephrine might exert a systemic beta-adrenergic tocolytic effect and slow labor. Early studies, which used large doses of epinephrine, instructed that the caudal epidural administration of native anesthetic with epinephrine prolonged the primary stage of labor and increased the variety of sufferers who required oxytocin augmentation of labor. In abstract, neuraxial analgesia seems to have a variable impact on the length of the first stage of labor. Second Stage of Labor There is little doubt that effective neuraxial analgesia prolongs the second stage of labor. Meta-analyses of randomized managed trials that in contrast neuraxial with systemic opioid analgesia assist this clinical statement (see Table 23. Data were abstracted for time period parturients in spontaneous labor with a singleton gestation within the vertex presentation and with normal perinatal outcome. The rate of spontaneous vaginal delivery declined as the length of the second stage of labor elevated; nonetheless, greater than 55% of ladies whose second-stage duration was 3 hours or longer nonetheless went on to deliver vaginally. Extending the length of the second stage will allow a significant variety of women to deliver vaginally. Summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Data are median (95th percentile) duration of the second stage of labor in spontaneous laboring women. Many ladies are requested to start "pushing" as quickly as full cervical dilation has been confirmed, regardless of the fetal station. Some practitioners have suggested that "delayed" pushing might result in much less maternal exhaustion and higher maternal and fetal outcomes. Several randomized research have sought to determine whether or not immediate or delayed pushing for girls with epidural analgesia during the second stage of labor affects labor length and outcome. In a 2017 meta-analysis together with thirteen research that in contrast early and delayed pushing in women with epidural analgesia, the authors judged that the proof ranged from average to very low quality. There was no distinction in perineal trauma, neonatal intensive care unit admissions, or 5-minute Apgar scores. The authors concluded that the present evidence is inadequate and inconclusive to help any specific timing and sort of pushing; additional high-quality research are essential. The duration of the third stage of labor was shorter in girls who obtained epidural analgesia and subsequently required handbook removing of the placenta. The researchers suggested that epidural analgesia Review: Pushing/bearing down strategies for the second stage of labor Comparison: 2 Analysis 2. The diamond represents the purpose estimate of the pooled threat ratio, and the size of the diamond is proportional to the confidence interval. Other Factors and Progress of Labor Oxytocin Active management of labor is an idea that consists of a disciplined, standardized labor administration protocol that includes early amniotomy and oxytocin augmentation if the cervix fails to dilate at a minimum price (usually 1 cm/hour in nulliparous women). Early research suggested that this sort of labor management decreased the speed of cesarean supply. In a search of the medical literature, they identified 16 randomized managed trials; eight of the sixteen trials included descriptions of labor management, and these trials have been included within the analysis. Seven of the eight trials described active management of labor and found no difference within the mode of delivery between groups. Only one of eight trials described using low-dose oxytocin and reported a markedly higher price of cesarean supply within the neuraxial analgesia group. The researchers had been correct in stating that the position of oxytocin in neuraxial analgesia end result studies has not been well controlled. In randomized managed trials that compared the consequences of neuraxial and systemic opioid analgesia on the outcome of labor, women who obtained neuraxial opioids had a higher price of oxytocin augmentation. Ambulation Observational research suggest that ambulation could additionally be associated with much less pain and a shorter duration of labor. There was no distinction between groups in the mode of delivery or duration of labor. These outcomes agree with those of a meta-analysis of 5 randomized controlled trials involving 1161 ladies. These results are similar to these of trials that in contrast ambulation and bed relaxation in women without neuraxial analgesia. First, systemic absorption of the anesthetic agents could also be adopted by transplacental switch of the drug, which has a direct impact on the fetus. Second, the results of neuraxial blockade on the mom could affect the fetus not directly. Effects of local anesthetics and opioids on the fetus and neonate are mentioned intimately in Chapter thirteen. The determinants of maternal plasma drug concentration, transfer across the placenta, and effects on the neonate are mentioned in Chapters four and 13. Determinants of maternal plasma drug concentration embody dose, website of administration, metabolism and excretion of the drug, and the presence of adjuvants. Factors that affect placental switch embrace maternal and fetal placental perfusion, the physicochemical characteristics of the drug, concentration of the free drug in maternal plasma, and permeability of the placenta. Most anesthetic and analgesic medication, including local anesthetics and opioids, readily cross the placenta. Indirect Effects the indirect fetal effects of epidural and intrathecal opioids may be extra significant than the direct results. Obviously, if the mom has extreme respiratory despair and hypoxemia, fetal hypoxemia and hypoxia will comply with. More frequent is the incidence of fetal bradycardia after initiation of neuraxial analgesia. The presumed trigger is that the speedy onset of analgesia ends in decreased plasma concentrations of catecholamines. A reduced circulating focus of epinephrine may result in increased uterine tone. Published observations counsel that uterine tachysystole and fetal bradycardia could observe the administration of either intrathecal or epidural analgesia during labor. Albright and Forster521 retrospectively reviewed outcomes for 2560 girls who delivered at their hospital between March Neonatal Depression Systemic absorption of native anesthetic or opioid may have neonatal results. This happens more typically after the systemic administration of opioid for labor analgesia. Additionally, scientifically rigorous studies are lacking, and many of the local anesthetic research had been carried out within the period when high-dose epidural analgesia was common; these observational research discovered that local anesthetics administered as parts of epidural analgesia have been generally related to minor, transient results on neonatal behavior. There was no difference between the 2 teams in the incidence of emergency cesarean supply (1. They found no difference between teams in the incidence of fetal bradycardia or uterine tachysystole, or want for urgent supply. Treatment of fetal bradycardia contains (1) reduction of aortocaval compression; (2) discontinuation of intravenous oxytocin; (3) therapy of maternal hypotension, if current; and (4) fetal scalp stimulation. Persistent uterine tachysystole should also prompt the administration of a tocolytic drug. Dense neuraxial anesthesia may adversely affect the progress of labor in some sufferers. However, maternal-fetal elements and obstetric management-not using neuraxial analgesia-are an important determinants of the finish result of labor. Anesthesia suppliers ought to identify these methods of analgesia that present the most effective ache aid with out unduly rising the risk for obstetric intervention. Despite these risks, many women opt for neuraxial analgesia as a result of no other method of labor analgesia offers its benefits (almost full analgesia), and the risks are acceptably low. Even no analgesia could additionally be extra hazardous to some women than neuraxial analgesia. Most ladies strongly dislike dense motor blockade, and many prefer to maintain some sensation of uterine contractions and perineal strain, particularly during the second stage of labor. However, a couple of ladies may settle for the probable improve in danger for instrumental vaginal supply in change for dense analgesia. The decision concerning the specific method and choice of drugs and doses is individualized for each parturient. Parity, stage and part of labor, use of intravenous oxytocin, and the presence of any coexisting disease(s), in addition to the standing of the fetus, are all thought of within the determination. Some anesthesia suppliers provoke intrathecal analgesia with both an opioid and a neighborhood anesthetic. The addition of a local anesthetic is pointless for reaching complete spinal analgesia throughout early labor; it may increase the danger for hypotension and lead to motor blockade in some patients, significantly whether it is followed by injection of an epidural check dose that incorporates a neighborhood anesthetic. However, the intrathecal administration of each an opioid and an area anesthetic achieves an extended period of analgesia and lower incidence and severity of pruritus than intrathecal injection of an opioid alone. Alternatively, epidural analgesia can be initiated with injection of a low-concentration native anesthetic answer (bupivacaine 0. The epidural catheter is sited and a standard epidural take a look at dose is injected, followed by administration of 5 to 15 mL of the native anesthetic/opioid resolution, injected in 5-mL increments. Ten to 15 mL supplies passable analgesia for most nulliparous ladies in early labor; injection of 20 mL may be needed if a dilute answer. We usually give an epinephrine-containing take a look at dose earlier than initiation of epidural analgesia in laboring women. Some anesthesia providers elect to omit the epidural test dose when initiating epidural labor analgesia, particularly if a lady needs to ambulate in early labor. The omission of the epidural take a look at dose requires that the therapeutic dose of local anesthetic be injected slowly, incrementally, and cautiously, because the therapeutic dose features as the test dose. These precautions must be followed with all bolus injections of local anesthetic by way of an epidural catheter. Alternatively, epidural analgesia could be initiated with a local anesthetic (bupivacaine zero. Women in lively labor could require a better whole volume of epidural local anesthetic solution (15 to 20 mL) than girls in early labor (10 to 15 mL) in addition to a better native anesthetic concentration. Labor sometimes progresses at a sooner rate in parous women, who often require a extra speedy onset of analgesia and extra in depth neuroblockade than nulliparous ladies when neuraxial analgesia is initiated at the similar cervical dilation. Sacral neuroblockade is required for full analgesia through the second stage of labor; this neuroblockade is difficult to accomplish in a well timed fashion with an initial (de novo) lumbar epidural injection of analgesic/anesthetic brokers. Maintenance epidural analgesia is usually initiated quickly after the initiation of analgesia (within 15 to 30 minutes) quite than ready for the neuroblockade to regress. The workload for the anesthesia supplier is lessened, as a result of she or he can arrange and initiate the epidural infusion whereas monitoring the patient for hypotension after initiation of neuroblockade. Patient satisfaction is better, and the workload for the anesthesia provider is decreased. For example, ladies in early labor require less drug to keep analgesia (6 to 10 mL/h), whereas women in additional advanced labor might require a higher infusion fee (8 to 15 mL/h). Similarly, a parous patient may require a higher infusion fee than a nulliparous affected person, although analgesia is initiated at the similar stage of labor. After evaluating the character of the pain, the extent of neuroblockade, and the progress of labor, we often deal with breakthrough ache with a bolus epidural injection of bupivacaine zero. Occasionally, we could elect to use a more concentrated native anesthetic resolution. In this case, the concentration of the maintenance answer can also have to be increased. This upkeep approach normally results in satisfactory perineal analgesia for supply. Occasionally, girls with epidural analgesia require extra (more dense) analgesia for supply, particularly if an instrumental vaginal delivery is planned. This usually ends in satisfactory sacral anesthesia in a patient with preexisting epidural labor analgesia. Frequent communication among members of the anesthesia, obstetric, and nursing groups is crucial to the secure and satisfactory provision of neuraxial labor analgesia.
Order prometrium overnight delivery. എയ്ഡ്സ് വൈറസ് ശരീരത്തിൽ കയറിയാലും അതിനെ നശിപ്പിക്കാൻ സാധിക്കും.. പ്രധാനപ്പെട്ട ഇൻഫർമേഷൻ.
Pregnancy end result in women with a quantity of sclerosis: outcomes from a prospective nationwide research in Finland medications januvia order prometrium online now. Birth outcomes and wish for hospitalization after delivery amongst girls with a quantity of sclerosis treatment 4th metatarsal stress fracture purchase prometrium in united states online. Perinatal characteristics and obstetric problems in mothers with multiple sclerosis: record-linkage examine symptoms 4 weeks 3 days pregnant purchase 200mg prometrium with amex. Exclusive breastfeeding and the risk of postpartum relapses in women with multiple sclerosis medications on nclex rn purchase prometrium overnight delivery. Regional analgesia for patients with persistent neurological illness and comparable situations medicine video buy cheap prometrium 100mg on line. Epidural analgesia and cesarean delivery in multiple sclerosis post-partum relapses: the Italian cohort examine medications prednisone buy prometrium 200 mg mastercard. Maternal butalbital use and selected defects within the National Birth Defects Prevention Study. Benzodiazepine exposure in pregnancy and risk of major malformations: a important overview. Antidepressant use during being pregnant and the risk of main congenital malformations in a cohort of depressed pregnant ladies: an updated evaluation of the Quebec Pregnancy Cohort. Antidepressant use late in pregnancy and danger of persistent pulmonary hypertension of the newborn. Pregnancy outcome after anti-migraine triptan use: a potential observational cohort research. Trimester-specific blood pressure ranges and hypertensive problems among pregnant migraineurs. Cerebral ischemia related to parenteral terbutaline use in pregnant migraine patients. Anesthetic administration of parturients with pre-existing paraplegia or tetraplegia: a case collection. Pregnancy and delivery in girls with a traumatic spinal twine harm in Sweden, 1980-1991. Epidural meperidine for management of autonomic hyperreflexia in a paraplegic parturient. Can epidural fentanyl management autonomic hyperreflexia in a quadriplegic parturient Management of autonomic hyperreflexia with magnesium sulfate during labor in a girl with spinal cord damage. Pregnancy and epilepsy; meeting the challenges over the past 25 years: the rise of the pregnancy registries. Antiepileptic drug clearance and seizure frequency throughout being pregnant in girls with epilepsy. Practice parameter replace: management points for girls with epilepsy�focus on being pregnant (an evidence-based review): obstetrical problems and alter in seizure frequency: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and American Epilepsy Society. Vitamin K, folic acid, blood levels, and breast-feeding: report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Monotherapy treatment of epilepsy in pregnancy: congenital malformation outcomes in the youngster. The effect of antiepileptic medicine on coagulation and bleeding within the perioperative interval of epilepsy surgical procedure: the Cleveland Clinic expertise. The epileptogenic properties of the volatile anesthetics sevoflurane and isoflurane in patients with epilepsy. Anaesthetic administration of a quadriplegic patient with extreme respiratory insufficiency present process caesarean part. Respiratory arrest throughout therapy for untimely labor in a affected person with myasthenia gravis. Prognostic factors for myasthenic disaster after transsternal thymectomy in sufferers with myasthenia gravis. Ventilatory support using bilevel constructive airway stress during neuraxial blockade in a affected person with severe respiratory compromise. Successful use of sugammadex for caesarean section in a patient with myasthenia gravis. Multivariate determinants of the necessity for postoperative air flow in myasthenia gravis. Characterization of the pattern of cognitive impairment in myotonic dystrophy sort 1. Pregnancy course and consequence in girls with hereditary neuromuscular issues: comparison of obstetric dangers in 178 sufferers. Anaesthesia for caesarean part in a affected person with myotonic dystrophy receiving warfarin remedy. Combined spinal and epidural anesthesia for belly hysterectomy in a affected person with myotonic dystrophy. Emergency caesarean section in a affected person with myotonic dystrophy: a case of failed postoperative extubation in a affected person with gentle illness. Obstetric elements in ladies with facioscapulohumeral muscular dystrophy, limb-girdle muscular dystrophy, and congenital myopathies. Anaesthetic management of a lady with autosomal recessive limb-girdle muscular dystrophy for emergency caesarean part. Epidural anesthesia in a parturient with neurofibromatosis kind 2 present process cesarean section. Responses to nondepolarizing neuromuscular blockers and succinylcholine in von Recklinghausen neurofibromatosis. Pregnancy problems in women with uncommon tumor suppressor syndromes affecting central and peripheral nervous system. Placental abruption and spontaneous rupture of renal angiomyolipoma in a pregnant woman with tuberous sclerosis. Labor analgesia and cesarean section in women affected by tuberous sclerosis: report of two instances. Conduct of anesthesia for delivery with grossly raised cerebrospinal fluid strain. The management of labour using continuous lumbar epidural analgesia in a patient with a malignant cerebral tumour. Brain tumor presenting with deadly herniation following supply underneath epidural anesthesia. Neuraxial anesthesia in parturients with intracranial pathology: a comprehensive evaluation and reassessment of risk. Anesthetic administration of neurosurgical procedures during being pregnant: a case sequence. Risk of cerebellar tonsillar herniation after diagnostic lumbar puncture in pseudotumor cerebri. Management of idiopathic intracranial hypertension in parturients: anesthetic concerns. Accidental spinal analgesia within the presence of a lumboperitoneal shunt in an obese parturient receiving enoxaparin therapy. Intrathecal anesthesia for cesarean supply by way of a subarachnoid drain in a lady with benign intracranial hypertension. Spinal anaesthesia for caesarean section for a lady with von Hippel Lindau illness. Worsening of neurologic signs after epidural anesthesia for labor in a Guillain-Barr� affected person. Guillain-Barr� syndrome after epidural anesthesia: direct nerve root damage could set off disease. Post-polio syndrome: pathophysiological hypotheses, prognosis standards, drug remedy. Oral polio vaccination during pregnancy: lack of influence on fetal growth and perinatal outcome. Cesarean delivery beneath ultrasound-guided spinal anesthesia [corrected] in a parturient with poliomyelitis and Harrington instrumentation. Successful use of succinylcholine for cesarean supply in a patient with postpolio syndrome. High-risk gestational trophoblastic neoplasia with brain metastases: individualized multidisciplinary therapy within the management of four sufferers. Anaesthetic management of uncontrolled idiopathic intracranial hypertension during labour and supply using an intrathecal catheter. An intrathecal catheter in a pregnant patient with idiopathic intracranial hypertension: analgesia, monitor and remedy Hydrocephalus and the reproductive health of women: the medical implications of maternal shunt dependency in 70 girls and 138 pregnancies. Pregnancy in girls with cerebrospinal shunts: a literature evaluate and case report. Anesthetic concerns for labor and supply in girls with cerebrospinal fluid shunts. Endovascular management of intracranial aneurysms during being pregnant in three circumstances and review of the literature. Arteriovenous malformations of the cerebral circulation that rupture in pregnancy. Diagnosis and management of cerebral venous thrombosis: a press release for healthcare professionals from the American Heart Association/American Stroke Association. Cerebral venous sinus thrombosis in being pregnant and puerperium: a pooled, systematic evaluation. Rapid development of amyotrophic lateral sclerosis presenting during being pregnant: a case report. Epidural anesthesia and pulmonary operate in a affected person with amyotrophic lateral sclerosis. Sensitivity to nondepolarizing muscle relaxants in amyotrophic lateral sclerosis: report of two cases. Two consecutive pregnancies in early and late stage of amyotrophic lateral sclerosis. Labor analgesia and anesthesia in a patient with spinal muscular atrophy and vocal cord paralysis. Caesarean part carried out underneath subarachnoid block in two sisters with spinal muscular atrophy. Anesthesia and perioperative medical administration of kids with spinal muscular atrophy. Disorders of pulmonary function, sleep, and the higher airway in Charcot-Marie-Tooth illness. Charcot-Marie-Tooth disease: peripartum management of two contrasting clinical circumstances. Data from the National Health and Nutrition Examination Survey present that in 2015 to 2016, 36. Understanding the pathophysiologic modifications and comorbidities associated with weight problems and being pregnant is crucial for the secure conduct of anesthesia in these high-risk patients. The effects of weight problems and pregnancy on the respiratory and cardiovascular techniques are summarized in Table forty nine. Obesity will increase the burden of the chest wall; thus, higher power expenditure is required throughout air flow to move this mass. Morbidly obese patients as compared with lean controls expend a disproportionately high percentage of complete oxygen consumption on respiratory work, even during quiet respiration. In overweight individuals, frequent shallow respirations may represent a extra efficient breathing pattern than massive tidal volumes. This sample of frequent shallow respirations contrasts to the elevated tidal volumes that typically accompany pregnancy. Decreased chest wall compliance and larger stomach weight promote airway closure within the dependent portion of the lung. In contrast, pulmonary blood flow preferentially occurs within the dependent portion of the lung, resulting in ventilation-perfusion mismatch and hypoxemia. Blood quantity and cardiac output are elevated, the latter owing to increases in each stroke quantity and coronary heart price. Both preload and left ventricular afterload are increased; these adjustments lead to each eccentric and concentric left ventricular hypertrophy. Among morbidly obese pregnant ladies, left atrial size, left ventricular thickness, interventricular septal thickness, and left ventricular mass are elevated compared with nonobese pregnant women. Pulmonary blood volume will increase in proportion to increases in cardiac output and total blood quantity. Gastrointestinal Changes It is unclear whether or not obesity in pregnancy is related to an increase in gastric volume and a lower in gastric pH. Roberts and Shirley15 reported that gastric volumes aspirated from obese laboring girls undergoing cesarean supply had been considerably larger than those obtained from lean controls. Studies within the basic surgical inhabitants, however, reported conflicting results; some confirmed these findings16 and others reported no difference in gastric volume and pH in overweight compared with lean sufferers. Both gastroesophageal reflux and hiatal hernia are extra common in overweight than in nonobese patients. Greater stomach weight restricts diaphragm movement, especially in the supine or Trendelenburg place, thus encouraging smaller tidal volumes. Coagulation Changes Obesity is related to a higher danger for thromboembolic complications. In the United Kingdom, 54% of girls who died from thromboembolic problems in 2009 to 2013 have been overweight or overweight. The risk is additional increased by lowered mobility, comorbidities corresponding to preeclampsia, and an increased frequency of operative delivery.
The biochemical and additional modifications that happen during blood storage can result in medications guide purchase line prometrium complications in the recipient treatment 5th metatarsal avulsion fracture cheap generic prometrium canada, notably when blood products are infused rapidly medicine hat horse buy 200mg prometrium fast delivery, as during massive transfusion for extreme hemorrhage treatment tendonitis prometrium 100mg with amex. The anticoagulant used for blood collection and storage contains citrate treatment 5th metatarsal shaft fracture effective prometrium 100 mg, which binds ionized calcium medicine cabinet home depot prometrium 100mg discount. Hypocalcemia results in decreased cardiac contractility, hypotension, and elevated central venous pressure. Despite the decrease pH, transfusion of blood rarely causes important acidosis so long as tissue perfusion remains adequate. Every affected person could have a different critical oxygen threshold, the point at which metabolism shifts from aerobic to anaerobic. Utilizing symptomatic and physiologic transfusion triggers quite than an absolute hemoglobin degree can target blood transfusion to the wants of the individual affected person. Transfusion practices differ widely227 and infrequently deviate from each nationwide and institutional guidelines. Active hemorrhage may immediate transfusion in some sufferers with a hemoglobin focus higher than 7 g/dL. Many anesthesia providers consider that the potential need for transfusion, and the occasional patient who develops an antibody from fetal antigen publicity during being pregnant, warrant the routine performance of a blood type and display screen on admission to the hospital for childbirth. Others counsel that this take a look at is pointless in wholesome girls without threat components for peripartum hemorrhage and negative antibody screens throughout the being pregnant. Given the low rate of transfusion in this group, the number-needed-to-treat is excessive. Blood Conservation Techniques Iron deficiency anemia is the most common reason for anemia during pregnancy because fetal erythropoiesis occurs at the expense of maternal iron stores (see Chapter 44). Intravenous remedy corrects anemia more quickly and reliably than oral iron remedy. The three methods of autologous transfusion are (1) preoperative (antepartum) donation, (2) normovolemic hemodilution, and (3) intraoperative blood salvage. However, these considerations are unfounded, as modern salvaging processes efficiently remove these contaminants. Furthermore, obstetric hemorrhage may be related to accelerated factor consumption, particularly throughout bleeding from the placental bed. Whole blood is an ideal alternative for sustaining intravascular quantity in the setting of massive hemorrhage. The excessive demand for blood elements such as platelets, plasma, and cryoprecipitate requires fractionation of more than 90% of donor blood into blood elements. Blood component remedy provides the patient with solely those merchandise which are required and helps extend the shelf-life of every unit of donor blood as a result of derivatives from one unit of blood can be utilized to deal with several patients. Characteristics of commonly administered blood products are summarized in Table 37. During massive resuscitation, care must be taken to keep away from hypothermia, acidosis, and hypocalcemia, because these circumstances contribute to coagulopathy. These units are packaged with preservatives and anticoagulant (citrate, phosphate, dextrose, adenine) and have a 42-day shelf-life. A unit of plasma has a quantity of roughly 250 mL and accommodates coagulation elements. In the setting of postpartum hemorrhage, cryoprecipitate is used to exchange fibrinogen, which is rapidly consumed during obstetric hemorrhage. Normal pregnancy is a hypercoagulable state, and coagulation exercise peaks on the time of parturition,260,262 presumably due to an increase in circulating tissue factor focus and enhancement of the tissue factor�dependent coagulation pathway. Patients who developed severe hemorrhage had lower fibrinogen, prothrombin, issue V, and antithrombin ranges in contrast with patients without severe hemorrhage. These early differences have been most hanging for fibrinogen; a fibrinogen concentration lower than 200 mg/dL on the time hemorrhage was identified had a one hundred pc positive predictive value for extreme hemorrhage, whereas a fibrinogen focus higher than 400 mg/dL had a 79% unfavorable predictive worth for subsequent extreme hemorrhage. The coagulation modifications have been according to a consumptive coagulopathy because they had been accompanied by will increase in thrombin-antithrombin complexes and d-dimer ranges, both markers of extreme coagulation. Other investigators have confirmed that decreases in fibrinogen correlate better than different hemostatic measures with the severity of hemorrhage. During active hemorrhage, clinicians should try to preserve the fibrinogen concentration larger than one hundred fifty to 200 mg/dL. Therefore, essentially the most efficient methodology to exchange fibrinogen during obstetric hemorrhage could also be to administer cryoprecipitate. Thrombocytopenia might develop after huge transfusion secondary to dilution, and platelet transfusion might turn out to be necessary when hemorrhage is accompanied by a platelet rely less than 50,000/mm3. This diploma of thrombocytopenia is uncommon unless blood loss exceeds 5000 mL or consumptive coagulopathy is current. In nonbleeding sufferers, a transfusion trigger of 20,000/mm3 has traditionally been instructed, though many clinicians favor to administer platelets earlier than the platelet count decreases to this value. Platelet dysfunction associated with bleeding may necessitate platelet administration. One unit of donor platelets increases the platelet depend by 5000 to 10,000/mm3 in the average grownup. One unit of apheresis platelets is equal to 4 to 6 items of pooled platelets. The investigators identified 246 patients who required large transfusion and separated them into low (median ratio 1: 8), medium (median ratio 1: 2. These authors articulated that deaths within the lowratio group occurred much sooner than deaths in the high-ratio group, raising the likelihood that those in the low-ratio group had more extreme accidents and died earlier than plasma could be thawed and administered. A 2013 publication described the retrospective evaluation of records from 142 women who had postpartum hemorrhage and required transfusion inside 6 hours of supply. However, its offlabel use has been reported in multiple scientific situations, including postpartum hemorrhage. Tranexamic acid binds to plasminogen, blocking its activation, thus inhibiting fibrinolysis. Bleeding postpartum patients display elevated ranges of d-dimer and plasmin-antiplasmin complexes, each markers of fibrinolysis, in contrast with nonbleeding sufferers, and administration of tranexamic acid attenuates these will increase. No differences in adverse events (including venous and arterial thromboembolic events) between the 2 teams had been obvious. More than 7% of those that died from hemorrhage within the research did so without having received any blood products. Uterine tamponade was used in solely 7% of examine topics, and uterine brace sutures in just 3%. These components make it extraordinarily unlikely that the United States will witness related survival advantages from tranexamic acid. The impact of tranexamic acid on hysterectomy charges and preservation of fertility among hemorrhaging women remains unknown. Nevertheless, tranexamic acid administration likely decreases blood loss and transfusion rates, much like its results in other nonobstetric, high�blood loss circumstances. Although data on thromboembolic events from nonobstetric285,286 and obstetric patients288 are reassuring, parturients are hypercoagulable, and caution could also be warranted. A case cluster of renal cortical thrombosis and irreversible kidney harm developed amongst 18 women treated with tranexamic acid for postpartum hemorrhage in France. Practitioners are cautioned to not exceed doses of 1 g administered slowly over 10 minutes; this dose may be repeated once if bleeding continues after 30 minutes. Aortoiliac thrombosis was reported after the concomitant use of tranexamic acid and an intra-arterial balloon catheter throughout urgent cesarean hysterectomy. It appears believable that tranexamic acid could profit ladies who demonstrate hyperfibrinolysis on viscoelastic monitoring. Its impact in high-resource settings is unknown, however it could lower blood loss and transfusion threat. Obstetric admissions to an integrated general intensive care unit in a quaternary maternity facility. Prediction of peripartum hysterectomy and end organ dysfunction in major obstetric haemorrhage. Trends in antagonistic maternal outcomes throughout childbirth: a population-based examine of extreme maternal morbidity. Etiology and risk elements for placenta previa: an outline and meta-analysis of observational research. Early morbidity and neurodevelopmental outcome in low-birthweight infants born after third trimester bleeding. Abnormal placentation: evidence-based analysis and administration of placenta previa, placenta accreta, and vasa previa. Management of the symptomatic placenta previa: a randomized, controlled trial of inpatient versus outpatient expectant administration. Transfusion-service-related activities: pretransfusion testing and storage, monitoring, processing, distribution, and stock management of blood parts. The anaesthetic management of caesarean part for placenta praevia: a questionnaire survey. Etomidate for induction of anaesthesia at caesarean part: comparison with thiopentone. Etomidate versus ketamine for fast sequence intubation in acutely unwell sufferers: a multicentre randomised controlled trial. An international distinction of rates of placental abruption: an age-period-cohort evaluation. Preterm untimely rupture of membranes, intrauterine an infection, and oligohydramnios: danger elements for placental abruption. Clinical utility of sonography in the prognosis and treatment of placental abruption. Placental abruption and placental hemorrhage: correlation of sonographic findings with fetal consequence. Maternal and fetal morbidity associated with uterine rupture of the unscarred uterus. Predicting uterine rupture in ladies present process trial of labor after prior cesarean supply. Sonographic measurement of lower uterine segment thickness to predict uterine rupture throughout a trial of labor in women with previous cesarean section: a meta-analysis. Signs, symptoms and problems of full and partial uterine ruptures throughout pregnancy and delivery. Frequent epidural dosing as a marker for impending uterine rupture in sufferers who try vaginal birth after cesarean supply. Is there a rise of postpartum hemorrhage, and is severe hemorrhage associated with extra frequent use of obstetric interventions Oxytocin publicity throughout labor among ladies with postpartum hemorrhage secondary to uterine atony. Twin deliveries in the United States over three a long time: an age-period-cohort analysis. Prophylactic oxytocin for the third stage of labour to forestall postpartum haemorrhage. The hemodynamics of oxytocin and different vasoactive brokers throughout neuraxial anesthesia for cesarean delivery: findings in six cases. Signs of myocardial ischaemia after injection of oxytocin: a randomized double-blind comparison of oxytocin and methylergometrine throughout caesarean part. Editorial board of the Confidential Enquiries into Maternal Deaths within the United K. An extract from why moms die 1997-1999, the Confidential Enquiries into Maternal Deaths within the United Kingdom. Intravenous oxytocin bolus of 2 models is superior to 5 units during elective caesarean section. Oxytocin bolus versus oxytocin bolus and infusion for control of blood loss at elective caesarean section: double blind, placebo managed, randomised trial. Five unit bolus oxytocin at cesarean supply in girls at danger of atony: a randomized, double-blind, managed trial. Comparison of two oxytocin regimens to stop uterine atony at cesarean supply: a randomized managed trial. Outcomes after establishment of a new oxytocin infusion protocol through the third stage of labor and immediate postpartum period. Impact of temperature publicity on stability of medication in a real-world out-of-hospital setting. Pregnancy-related acute myocardial infarction in Japan: a review of epidemiology, etiology and therapy from case reports. The origin of circulating 13,14-dihydro-15-keto-prostaglandin F2 alpha during delivery. Life-threatening bronchospasm after intramuscular carboprost for postpartum haemorrhage. Misoprostol for preventing and treating postpartum hemorrhage in the community: a better take a glance at the proof. Postpartum hemorrhage: abnormally adherent placenta, uterine inversion, and puerperal hematomas. Severe main postpartum hemorrhage because of genital tract laceration after operative vaginal delivery: profitable therapy with transcatheter arterial embolization. Timing of prophylactic uterotonics for the third stage of labour after vaginal start. Prophylactic antibiotics for guide removing of retained placenta in vaginal birth. Postpartum hemorrhage resulting from uterine atony after vaginal supply: components related to severity. Intravenous nitroglycerin for uterine rest within the postpartum affected person with retained placenta. Risks and penalties of puerperal uterine inversion within the United States, 2004 via 2013. The use of intravenous nitroglycerin for cervico-uterine relaxation: a evaluation of the literature.