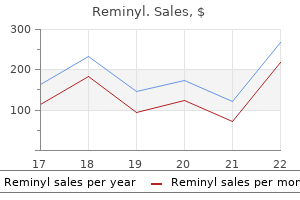
Dr Nicholas Barrett
- Consultant in Intensive Care Medicine
- Guy? and St Thomas?Hospital
- Westminster Bridge Road
- London
This was demonstrated by fluctuations of the detrusor pressure when it reached maximum throughout voiding and resumption of urinary stream at the facet of a pointy fall within the detrusor stress symptoms zinc toxicity buy reminyl 8 mg cheap. The high detrusor pressures throughout voiding are thought to characterize variations among particular person infants in the maturation means of detrusor and sphincter coordination in the course of the first 1 to 2 years of life (Yeung et al treatment canker sore purchase generic reminyl on-line, 1995a treatment 5th metatarsal base fracture purchase 4 mg reminyl with visa, 1998; Holmdahl et al medicine shoppe locations order 8mg reminyl with amex, 1996; Bachelard et al symptoms throat cancer buy reminyl with paypal, 1999; Sillen et al medicine everyday therapy reminyl 8mg on line, 2000). In distinction, resumption of urinary flow was associated with rest of the external urinary sphincter and a paradoxic drop in detrusor strain. Also, the detrusor strain associated with the initiation of urinary flow was usually significantly lower than the maximal detrusor stress throughout micturition (Pdetmax) and the Pdetmax was considerably larger than those recorded in normal adults. During the third trimester of being pregnant, the fetus is voiding on the price of roughly 30 times each 24 hours (Goellner et al, 1981). However, immediately after birth, this drops dramatically for the primary few days of life, solely to improve once more after the primary week to attain a peak by week 2 to 4 to a median of once per hour. Subsequently this fee declines once more to approximately 10 to 15 occasions per day between 6 to 12 months and to about eight to 10 occasions per day by 2 to 3 years (Goellner et al, 1981; Yeung et al, 1995b; Holmdahl et al, 1996). This discount in voiding frequency noticed during the first few years of life seems to be related mainly to an increase in bladder volume in parallel to body progress, which is proportionately larger than simultaneous increase in urine volume manufacturing (Yeates, 1973; Koff, 1997). By the age of 12, the voiding sample is very related to that in an adult and usually comprises four to 6 voids per day. The improve in bladder volume with the growth of the child is a vital step within the development of bladder operate and urinary continence. An sufficient reservoir perform for urine storage is important to meet the elevated rate of urine manufacturing and decreased voiding frequency within the growing child. A delay within the normal maturation of bladder management was attributed to certain circumstances corresponding to main nocturnal enuresis and hence the normal belief that each one enuretics would get higher with age (Nash, 1949). However, more modern studies have indicated that that is an oversimplification of what actually happens. Even in full-term fetuses and newborns, it has been shown that micturition is modulated by higher facilities. Ohel and associates (1995) confirmed that intrauterine micturition virtually exclusively occurs whereas the fetus is awake rather than randomly distributed over various behavioral (sleep/arousal) states. Furthermore, it has been observed that mic- turition in a full-term fetus may be elicited by vibroacoustic stimulation, all of which point out that the micturition reflex might be under greater neural management even at close to gestational term (Zimmer et al, 1993). During sleep the bladder is generally quiescent and secure with lack of facilitation of detrusor contractions, whereas during wakefulness marked detrusor overactivity is observed. Clear electroencephalographic evidence of cortical arousal or actual awakening occurs in response to bladder distention, and sleeping infants are famous to wake up before bladder exercise returns and voiding occurs. However, this arousal interval typically may be transient, with the toddler crying or transferring for a short interval, micturating, and then going again to sleep with out being seen to have woke up. This wakening response to bladder distention in all probability involves more complicated neural pathways and better centers than has been appreciated till now. These outcomes additionally correlate with latest animal studies displaying a sophisticated integration of preexisting central and peripheral neural pathway in micturition management at birth with remodulation occurring within the early postnatal period (Maggi et al, 1986; Thor et al, 1989). Extensive research by de Groat and colleagues (de Groat, 1993; de Groat et al, 1998; Sugaya and de Groat, 1994; Araki and de Groat, 1997; Sugaya et al, 1997) utilizing experimental animals have indicated that early postnatal maturation of bladder function in all probability happens at different ranges: (1) modifications in the properties of detrusor muscle; (2) developmental modifications within the peripheral innervation of the bladder; and (3) alterations in central synaptic circuitry and neuroplasticity within the parasympathetic reflex pathways to the bladder. Recordings of spontaneous exercise in bladder easy muscle in neonatal rats showed a lot larger amplitude and more synchronous rhythmic contractions in comparison with those observed in grownup rats (Sugaya and de Groat, 1994). In addition, peripheral and central neural mechanisms also change extensively throughout this era. In cats (and some other species) micturition through the newborn interval depends on an exteroceptive somatovesical reflex triggered when the mother licks the perineum of the kittens (de Groat et al, 1993, 1998; Araki and de Groat, 1997). This somatovesical reflex, processed in the sacral spinal wire, disappears in older animals however might reappear after spinal twine injury. This interneuron� preganglionic neuron synaptic transmission may be very efficient instantly after birth however could be very abruptly downregulated through the third postnatal week when the mature supraspinal micturition reflexes start to seem (Araki and de Groat, 1997). Transection of the spinal twine prevents this downregulation, indicating that the upper neural centers play an necessary position on this synaptic reworking, which contributes to postnatal improvement of micturition reflexes. The youngster turns into more conscious of the sensation of bladder distention and the urge to urinate, as well as the social norm and embarrassment associated with urinary incontinence. This pure evolution of micturition management mechanisms is dependent upon an intact neural pathway and consciousness of social norms, as well as multiple elements, together with the gradual enhance in practical bladder capability, maturation of detrusor-sphincter coordination and progressive growth of voluntary control over the entire bladder-sphincteric-perineal complicated. The last steps are normally achieved at roughly three to four years of age, when most children have developed the grownup sample of urinary control and shall be dry each day and night. The baby has discovered to inhibit a micturition reflex and postpone voiding and to voluntarily initiate micturition at socially acceptable and handy instances and places. This growth of continence and voluntary micturition also is dependent upon behavioral learning and could be influenced by rest room training, which in turns is determined by the cognitive perception of the maturing urinary tract. It is understandable therefore that this collection of complex events is extremely prone to the development of assorted kinds of dysfunctions. Neurologic control of regular micturition occurs at totally different ranges of the central nervous system, from the spinal cord with the sacral micturition center to the brainstem with the pontine micturition middle, the cerebellum, basal ganglia, limbic system, thalamus and hypothalamus, and cerebral cortex (Blaivas, 1982; McLorie and Husmann, 1987; de Groat, 1993; Fernandes et al, 1994). It should be noted that the bladder is unique amongst visceral organs in that its function is beneath the management of each the somatic and the autonomic nervous systems. Besides acetylcholine and norepinephrine, various different neurotransmitters, together with prostaglandin substance P, opioid peptides, vasoactive intestinal peptide, and neuropeptide Y, are involved throughout bladder stimulation (Fernandes et al, 1994). Simple manipulation of adrenergic and cholinergic receptors may abolish solely partially the effect of neural stimulation, which explains why pharmacologic blockage of the classic neurotransmitters (acetylcholine and norepinephrine) alone might fail to elicit the anticipated full medical response. However, if voiding dysfunctions are persistent nicely past the period of bathroom coaching, especially if related to urinary complications corresponding to recurrent urosepsis, the potential for underlying anatomic and neurologic causes have to be thought-about and duly evaluated. It has been reported that 15% of 6-year-old children have this condition (Hoebeke, 2002). For instance, a girl with dysfunctional voiding may begin with having detrusor overactivity associated with sphincter and pelvic ground overactivity, then steadily evolve to develop fractionated voiding with rising post-micturition residues, and at last develop bladder decompensation and the "lazy bladder" syndrome (van Gool et al, 1992). It additionally should be emphasized that use of the time period non-neuropathic relies purely on the fact that no obvious and neurologic lesions could be recognized. However, situations such because the urofacial syndrome complex (Ochoa syndrome) and the Hinman syndrome (severe bladder and bowel dysfunction) behave almost identically to the everyday neuropathic bladder-sphincter dysfunctions. It is certainly conceivable that they do have an natural underlying neurologic cause, though the exact neuroanatomic lesion has not but been recognized. Hence, the excellence between neuropathic and non-neuropathic bladdersphincteric dysfunctions is probably not as clear as historically thought. In contrast, neural control over the bladder-sphincter unit in kids is age-dependent and is rather more variable and complicated. Various classifications for bladder dysfunctions in kids have been described over the past few a long time (Lapides, 1970; Bellinger, 1996; Wein, 1998). This was subsequently revised in 2006 and most lately in 2014 (Nev�us et al, 2006; Austin et al, 2014). For instance, it has been clearly proven that a major proportion of regular infants exhibit prominent detrusor-sphincter discoordination and interrupted voiding through the first 1 to 2 years of life. This is manifested by a discoordinated and interrupted urine move that even could additionally be delivered to a complete stop for 1 to 2 minutes before restarting, producing a pattern of repeated small voidings in quick succession (Yeung et al, 1995a, 1995b, 1998). Urodynamic findings present affiliation with excessive voiding pressures and interruption of circulate but no impairment of general bladder emptying. The commonality of bowel emptying issues with bladder operate is mirrored on this new terminology. Older phrases similar to Hinman bladder, non-neurogenic neurogenic bladder, occult neurogenic bladder, and dysfunctional elimination syndrome have turn out to be out of date. By this new time period the shut relationship between bowel and bladder function is acknowledged. Thus the significance of bowelrelated terms in relation to bladder function is emphasized. The rectum and urinary bladder have close anatomic proximity, they usually share innervation from parasympathetic S2 to S4 and sympathetic L1 to L3 nerve roots. These sufferers would doubtlessly benefit from a multidisciplinary remedy approach involving urology, gastroenterology, and psychology professionals (Wolfe-Christensen et al, 2013). History Medical History and Questionnaires and Scoring Systems Literature on this topic is sparse. This should embrace related inquiries to exclude neurologic and congenital abnormalities. Bowel dysfunction can coexist in the type of encopresis, constipation, and fecal impaction and must be noted during acquiring the historical past. The urinary historical past should give attention to symptoms associated to both the storage and evacuation of urine. If potential, the historical past is obtained from each the child and the parents/ guardians. Clear distinction ought to be made between steady and intermittent incontinence and between nighttime and daytime urine loss. Quantification of urine loss is subjective, and, if essential, a pad test may help to make it extra goal. The medical history should start with an obstetric historical past asking for possible fetal distress, anoxia, start trauma, prenatal hydronephrosis, and oligohydramnios. Furthermore, voiding frequency, urine loss frequency, urge, and reactions to urge should be assessed. Toilet conduct and subjective quantification of the urinary stream are necessary parameters. Staccato voiding is tough to distinguish by the affected person; nevertheless, fractionated voiding is nicely recognized. Especially in girls, one ought to ask for deviations of urinary stream or eventual compensations in rest room posture. Many ladies with an anterior deflection of the urinary stream take a ahead bent position on the toilet. After screening the wet child by this means, those sufferers who will profit from further urodynamic research may be selected. Urine loss is quantified by recording if clothing needed to be modified after the urine loss (= important urine loss) or not. The chart provides information about fluid intake, variety of voidings, voided quantity, and urine loss. Briefly, a 7-day bowel diary is advisable and includes the Bristol Stool Form Scale. Bowel function (obstipation, soiling) in addition to menstrual and, if relevant, sexual function should be assessed. General historical past taking includes questions related to neurologic and congenital abnormalities. All diagnostic and therapeutic interactions that have been performed previously should be assessed. The first scoring system was used by the International Reflux Study in Children group and described by Jan van Gool and colleagues (1992). This scoring system, developed to interpret knowledge obtained from the International Reflux Study, was not validated and has never been used in day by day practice. A extra lately printed scoring system devised by Akbal and associates (2005) relies on this scoring system. A second scoring system, from the Toronto group, was published in 2000 (Farhat et al, 2000). It is a validated questionnaire consisting of 10 questions with good sensitivity and specificity for diagnosing dysfunctional voiding. The similar group printed a manuscript on the use of their scoring system to predict end result of reflux after therapy of dysfunctional voiding (Upadhyay et al, 2003). The main advantage of using a scoring system is to help people with limited expertise. They are found to be legitimate and dependable (Afshar et al, 2009; Drzewiecki et al, 2012). A validated bladder/bowel dysfunction questionnaire is a helpful gizmo in the pediatric urology medical PhysicalExamination Besides a general pediatric examination, which pays particular attention to belly palpation in search of fecal impaction, perianal and perineal sensation, anal sphincter tone, and bulbocavernosus reflex ought to be assessed. The perineal area is provided by the sacral segments S1 to S4, which also supply part of the bladder and the urethral sphincter. Complete evaluation of the back with special attention for cutaneous manifestations of an underlying occult spinal dysraphism (lipoma, skin discoloration, hair growth) is critical to rule out any underlying neurogenic trigger (Mandell et al, 1980). Examination of lower extremities can present lesions compatible with neurogenic illnesses affecting the lumbar cord. Muscle atrophy, foot deformities, and any asymmetry of the lower extremities should draw our attention. Genital examination, which includes inspection of the introitus in ladies with special attention to the place of the urethral meatus, appearance of the hymen, and inspection of the penis and the meatus urethrae in boys, should be carried out (Hoebeke et al, 1999). Infection may be the consequence of the dysfunctional voiding because turbulence in the urinary stream can milk-back bacteria from the urethra to the bladder. On the opposite hand, an infection may be the origin of some irritative bladder symptoms. The presence of glucose or proteins in urine can detect metabolic or nephrologic diseases that may intrude with bladder perform. In women, lengthening of the urethra and movement of the bladder neck in the course of the symphysis is seen. However, in sufferers with non-neuropathic bladder-sphincter dysfunction, approximately one third of the children were unable to elicit motion of the pelvic flooring or had paradoxic motion. The scientific significance of this remains unclear, however when launched to a period of urotherapy, marked improvement of signs had been reported. Studies have proven that in a proportion of women with hyperlaxity of joints, coughing or straining would end in a large opening of the bladder neck and urethra.
The external oblique fascia is opened within the course of its fibers medications xanax discount 4 mg reminyl otc, with care taken to avoid injuring the ilioinguinal nerve treatment 32 buy reminyl no prescription. In young infants administering medications 8th edition order reminyl 4mg on-line, the inner and exterior inguinal rings are in shut proximity medications beginning with z cheap reminyl, providing sufficient access with out opening of the exterior indirect fascia (Mitchell-Banks technique) (Kurlan et al treatment of bronchitis purchase genuine reminyl line, 1972) symptoms 14 days after iui order 8 mg reminyl otc. For bilateral inguinal hernias, Shih described a median raphe method (Shih and Uen, 2012). Initial data counsel no major differences in success rate or morbidity using the scrotal approach compared with normal inguinal surgical procedure. Fearne and colleagues (2002) ligated the processus vaginalis on the degree of the exterior inguinal ring in 195 boys and saw 1 recurrence (mean follow-up, thirteen months). Laparoscopic Inguinal Hernia Repair Laparoscopic hernia restore utilizing two main techniques-peritoneal closure of the defect (Schier, 2006) and an extraperitoneal method (Takehara et al, 2006; Endo et al, 2009)-has gained curiosity. Alzaham carried out a meta-analysis of 10 comparative research of laparoscopic versus open inguinal hernia repair in 2699 infants and kids. Laparoscopic methods have been associated with a development toward larger recurrence fee, longer operative time for unilateral repairs, and shorter operative time for bilateral repairs. There was a big discount in growth of a contralateral metachronous inguinal hernia within the laparoscopic group (Alzahem, 2011). Surgery can be carried out effectively but the recurrence risk remains greater (up to 4%) than with open repair, although it could decrease with increasing experience (Saranga Bharathi et al, 2008). Conflicting literature exists relating to levels of ache and operative time after laparoscopic repair (Chan et al, 2005; Koivusalo et al, 2009). The incidence of an open contralateral inside ring amongst boys youthful than 1 year and not utilizing a clinical hernia is 10% undergoing laparoscopic orchidopexy (Palmer and Rastinehad, 2008). Among those present process unilateral inguinal hernia repair, the incidence of a contralateral patent processus vaginalis ranges from 57% to 68% during open exploration and 39% to 61% throughout laparoscopic hernia repair (Tepas and Stafford, 1986; Zona, 1996; Miltenburg et al, 1998; Saad et al, 2011). The incidence is inversely related to age; Chin and colleagues (1995) discovered an open contralateral ring in 41% of infants younger than 1 12 months, in about 30% of toddlers aged 2 to 5 years, and in 19% of youngsters older than 10 years. A meta-analysis by Miltenburg and colleagues (1997) of studies together with patients in whom the patency standing of the contralateral ring was unknown reported a 7% threat of creating a metachronous contralateral hernia, with 90% developing within 5 years of the initial restore. Among 1291 kids whose contralateral ring was deemed closed by transinguinal laparoscopy, 2. Unfortunately, these studies offer oblique perception into the pure history of an open inside ring, and the query of the pure history of such a hoop will remain unanswered till a potential examine of recognized open contralateral inside inguinal rings is performed. AbdominoscrotalHydrocele Abdominoscrotal hydroceles are unusual, accounting for 1. These noncommunicating scrotal lots are tense and prolong into the stomach, the place they could be palpable. Abdominoscrotal hydroceles usually manifest in infancy as such or as scrotal hydroceles that enlarge over time (Celayir et al, 2001; Cuervo et al, 2009), enhance (Cozzi et al, 2008), or resolve spontaneously (Upadhyay et al, 2006). Associated diagnoses include cryptorchidism, contralateral hernia, hydrocele, or vanishing testis. The more than likely cause is enlargement and extension of a scrotal hydrocele into the retroperitoneal or properitoneal space after closure of the processus. The aim of contralateral evaluation is avoidance of metachronous hernia growth and its attendant dangers and prices. Historically, routine contralateral exploration was carried out, after which extra selectively in patients considered at excessive danger for metachronous hernia based mostly on age, prematurity, gender, or associated disease. In a survey, 51% of pediatric common surgeons acknowledged that they routinely carry out contralateral exploration in premature infants; 40% carry out exploration in boys younger than 2 years, and 13% in boys ages 2 to 5 years (Levitt et al, 2002). Whereas the usual laparoscopic strategy makes use of three ports, some authors report related outcomes utilizing two ports (Xu et al, 2013) or even a single port (Shen et al, 2010). Turial and associates (2011a) reviewed their experience in 147 infants who weighed 5 kg or much less utilizing both a 5-mm scope or a microlaparoscope and 2-mm devices. No circumstances of testicular atrophy occurred, and high testes requiring surgical procedure occurred in 4%, which was inversely associated to body weight. Esposito and associates (2010) performed outpatient laparoscopic inguinal hernia repair on 50 children younger than 1 12 months. After division of the sac distal to the ring, the peritoneum was closed utilizing a purse-string suture of a nonabsorbable materials. The median working time was 22 minutes (unilateral, 7 to 30; bilateral, 12 to 42) with one recurrence. Recurrence rates may be lower in those youthful than 1 year than in older kids (Choi et al, 2012). Esposito and colleagues (2013) reported their experience with 46 sufferers with an incarcerated hernia (1 month to 8 years), of which over one half have been irreducible. They purport three main benefits of the laparoscopic strategy: aversion of edematous tissue by bypassing the wire buildings; bowel reduction performed under direct visible management; and inspection of the incarcerated organ at case finish. Viral Sterile or traumatic Scrotal edema or erythema Diaper dermatitis, insect bite, or different skin lesions Idiopathic scrotal edema Orchitis Associated with epididymitis with or with out abscess Vasculitis. Massive enlargement could extend into the upper stomach and be associated with hydroureteronephrosis, lower extremity edema, or appendicitis (reviewed by Cuervo et al, 2009). Chamberlain and colleagues (1995) first reported dysmorphic elongation of the testis; this was subsequently confirmed (Bayne et al, 2008) however discovered to be reversible generally (Cozzi et al, 2008). The conventional surgical approach is an inguinal incision with proximal dissection of the sac from its belly attachments and distal complete or partial mobilization, with or without orchidopexy. Some authors advocate orchidopexy to keep away from iatrogenic cryptorchidism (Nagar and Kessler, 1998; Bayne et al, 2008). Aspiration of the scrotal part could facilitate the proximal dissection (Cuervo et al, 2009). Alternative approaches embrace a midline stomach method for large bilateral circumstances (Serels and Kogan, 1996) or laparoscopic decompression of the abdominal part adopted by inguinal excision (Abel et al, 2009). To avert harm to the spermatic cord or vas, a strip of the liner of the sac could also be left alongside the wire (Ferro et al, 1995; Cuervo et al, 2009). Tightening of a patulous inner ring is described, but could also be pointless as a result of the processus vaginalis is invariably closed. Belman (2001) described a major scrotal strategy with drainage and extensive plication with limited dissection; excision is performed. Cozzi and colleagues (2008) reported reduced morbidity and related efficacy for the scrotal (5 patients) strategy compared with the inguinal method (13 patients). Persistent scrotal swelling, hematoma, and undescended and/or hypoplastic testis was reported in 11 inguinal circumstances and an infection in 2 scrotal circumstances. There is a limited differential analysis (Box 146-2) with considerable overlap of indicators and symptoms, which may have an effect on the power to make a definitive diagnosis; some dependable scientific features exist, and adjuvant use of scrotal imaging is useful in making a analysis. Torsion of the appendix testis is the most typical analysis (40% to 60%), followed by spermatic cord torsion (20% to 30% excluding neonates), epididymitis (5% to 15%), and other or no pathology (10%) (Anderson and Giacomantonio, 1985; Sidler et al, 1997; Van Glabeke et al, 1999; Mushtaq et al, 2003; Murphy et al, 2006; M�kel� et al, 2007). Although all of those ailments can happen at any time during childhood, appendage torsion is typically most typical after infancy and before puberty, whereas epididymitis and spermatic twine torsion are most typical within the perinatal and pubertal intervals. SpermaticCordTorsion Acute Intravaginal Spermatic Cord Torsion Predisposing Factors. Intravaginal torsion is usually attributed to excess mobility of the testis within a "bell-clapper deformity" whereby the tunica vaginalis abnormally fixes proximally on the cord. Although found in 12% of males at autopsy (Caesar and Kaplan, 1994a), the prevalence of torsion is much decrease: 8. There is proof for a familial predisposition (Cunningham, 1960; Collins and Broecker, 1989; Cubillos et al, 2011) for which the transmission is unknown. Cubillos and colleagues (2011) found a household history (various relatives) in 10% of probands, including one household with three generations of torsion. The inciting occasion for torsion is unknown but could include cold temperature (Srinivasan et al, 2007; Lyronis et al, 2009; Chiu et al, 2012) or a change in temperature (Chen et al, 2013) activating the cremasteric reflex, and/or rapid testicular development at puberty; but torsion may happen at relaxation or at sleep. Cryptorchid testes are at elevated threat of torsion and troublesome to assess because of the excessive position. Intravaginal testicular torsion might happen at any age, however the vast majority of instances occur after age 10 years with a peak at 12 to sixteen years (Anderson and Giacomantonio, 1985; Sidler et al, 1997; Mushtaq et al, 2003; Mansbach et al, 2005; Murphy et al, 2006; M�kel� et al, 2007). The prevalence of testicular torsion is 1 in 4000 (Williamson, 1976) with left-sided predominance and uncommon bilaterality. Classically, boys complain of acute, severe scrotal pain that happens at rest (even sleep), or with bodily exercise or after trauma. Alternatively, sufferers might have milder, less acute, or even absent scrotal pain or could have inguinal or stomach pain. Nausea and vomiting happen in 10% to 60% of boys (Williamson, 1976; Knight and Vassy, 1984; Jefferson et al, 1997; Sessions et al, 2003; M�kel� et al, 2007). Scrotal edema and erythema could also be present, relying on the period or diploma of torsion. The most typical bodily findings are generalized testicular tenderness, irregular orientation of the testis, and absent cremasteric reflex. The genitofemoral reflex arc, normally current after age 2 years (Caesar and Kaplan, 1994b), is elicited by scratching the inside thigh with resultant testis elevation. Some research report decreased or absent reflex in all cases of testicular torsion (Caldamone et al, 1984; Rabinowitz, 1984; Kadish and Bolte, 1998), nevertheless it was intact in up to 10% of confirmed circumstances of torsion in different collection (Hughes et al, 2001; Nelson et al, 2003; Karmazyn et al, 2005; Murphy et al, 2006). Although anterior epididymal position, thickening of the cord, testicular induration, lack of boundaries between the testis and epididymis, scrotal edema, and/or erythema may be present, landmarks turn out to be obliterated and the examination much less reliable as the duration of torsion increases. Several efforts have been made to offer a better scientific evaluation of testicular torsion in sufferers with the acute scrotum. Using a standardized history and bodily examination kind, Srinivasan and colleagues (2011) found that absence of ipsilateral cremasteric reflex, nausea or vomiting, and scrotal skin modifications on multivariate evaluation were predictive of testicular torsion. According to use of a call device, sufferers with acute (<72 hours) scrotal ache and the entire following had no risk of testicular torsion (100% sensitivity and unfavorable predictive value): regular testicular lie, lack of nausea and vomiting, and age 0 to 10 years (Shah et al, 2013). Barbosa and colleagues (2013) developed a scoring system primarily based on testicular swelling, hard testicle, absent cremasteric reflex, nausea or vomiting, and high-riding testis that wants further validation. Urinalysis is of restricted usefulness in cases of testicular torsion however is used to establish pyuria and/or bacteriuria related to epididymitis, or hematuria, implicating a urinary tract calculus. Before the arrival of dependable and speedy scrotal imaging, immediate scrotal exploration was routine. Radionuclide imaging carried about 90% sensitivity and specificity but was lengthy, was not readily available, and used ionizing radiation and is presently hardly ever used. Ultrasound offered a speedy, available, and protected modality to assess testicular structure, intraparenchymal blood move, and different anatomic particulars (hydrocele, scrotal thickening). Sessions and associates (2003) found that the median diploma of rotation was 540 degrees in orchiectomy testes and 360 levels when the testis was salvaged, with a range of one hundred eighty to 1080 levels in each groups. The threat of delayed atrophy after orchidopexy was less than 10%, 40%, and 75% after less than 12, 12 to 24, and more than 24 hours of pain, respectively (Visser and Heyns, 2003). Partial (<25%) testicular atrophy may happen after operative detorsion even after 4 hours after the onset of pain (Krarup, 1978; Anderson and Williamson, 1986; Tryfonas et al, 1994; Sessions et al, 2003). Preoperative manual twine detorsion could relieve symptoms and permit delayed orchidopexy however might incompletely untwist the cord. One is to keep away from delay and perform exploration in virtually all boys to confirm absence of torsion; this implies many unnecessary surgeries (Anderson and Giacomantonio, 1985; Watkin et al, 1996; Sidler et al, 1997; Mushtaq et al, 2003; M�kel� et al, 2007). Surgical exploration of the testis through a hemiscrotal transverse (dartos pouch) or midline raphe incision ought to first address the affected facet. The testis is delivered and the tunica vaginalis opened to note the colour of the testis, the number of rotations, and the anatomy of the tunica vaginalis. The testis is untwisted, wrapped in heat soaked gauze, and observed for improvement in color whereas the contralateral testis is fastened with nonabsorbable suture to cut back the risk of metachronous torsion. The affected testis is re-examined for potential viability, and the largely subjective determination for orchidopexy or orchiectomy is made. A Doppler flow probe or incision of the tunica albuginea (Arda and Ozyaylali, 2001) with evaluation of bleeding might document intratesticular circulate after detorsion; nonetheless, the reliability of those assessments lacks validation. Kutikov and colleagues (2008) have instructed that a compartment syndrome contributes to testicular harm based on the improved look and lower intraparenchymal pressures seen after detorsion and tunica albuginea incision in three instances. A patch of vascularized tunica vaginalis was positioned in the tunica albuginea defect to preserve lower intraparenchymal stress and to scale back the likelihood of ongoing ischemia. Risk elements for orchiectomy include young age, African-American race, and being on Medicaid or missing insurance coverage (Cost et al, 2011; Zhao et al, 2011). This might replicate the switch of patients, which delayed remedy by seventy five minutes within the examine by Bayne and colleagues (2010). Orchiectomy is carried out by dividing the wire into segments, each of which is ligated with nonabsorbable suture. In cases of orchiectomy, prosthesis placement is usually provided after full healing or later in puberty; however, Bush and Bagrodia (2012) demonstrated the feasibility of performing concurrent prosthetic placement and orchiectomy. However, in other research the sensitivity in confirming decreased or absent blood flow in confirmed circumstances of spermatic wire torsion was solely 63% to 90%, probably because of enhanced detection of flow with newer equipment and/or user-dependent traits (Steinhardt et al, 1993; Stehr and Boehm, 2003; Bentley et al, 2004; Kalfa et al, 2004; Karmazyn et al, 2005). Cassar and colleagues (2008) evaluated Doppler waveforms in instances of torsion with decreased or preserved testicular move and noticed subtle waveform abnormalities, together with increase or decrease in amplitude relative to the normal testis and reversal of diastolic flow. Increased epididymal measurement and/or echogenicity and altered epididymal vascularity, often absent or decreased but sometimes increased, could present additional support for the prognosis of torsion (Nussbaum Blask and Rushton, 2006). However, Karmazyn and coworkers (2005) observed normal testicular blood move and no visible spermatic cord twist in 2 of 41 boys with partial or intermittent torsion. Infrared thermography confirmed vital discount in scrotal temperature by 1 hour after 720-degree torsion and prompt normalization with detorsion in a sheep mannequin (Capraro et al, 2008). Management and Surgical Treatment Testicular torsion is a real surgical emergency because testis viability is inversely associated to period of torsion. Visser and Heyns (2003) amassed data from revealed collection together with 1140 patients and located the chance of orchiectomy was approximately 5%, 20%, 40%, 60%, 80%, and 90% at 0 to 6, 7 to 12, 13 to 18, 19 to 24, greater than 24, and greater than forty eight hours after onset of ache, respectively. The degree of torsion may provide incomplete vascular occlusion, helping to explain the variability of those knowledge. Semen density is often throughout the normal vary however correlates with shorter length of torsion and reduced atrophy (Puri et al, 1985; Fisch et al, 1988; Anderson et al, 1992; Brasso et al, 1993; Arap et al, 2007). The statement that growing duration of torsion inversely correlates with semen high quality and restricted contralateral testicular biopsy knowledge suggest that world testicular dysfunction may exist after torsion (Visser and Heyns, 2003).
Some of the remnant bladder is made right into a small seminal receptaculum and the penis is reconstructed throughout the same procedure medications errors pictures cheap reminyl 8mg without a prescription. In ladies medicine versed order cheapest reminyl and reminyl, the exterior genitalia are reconstructed and anterior fixation of the uterus is performed medicine zithromax buy reminyl overnight. In 1996 6mp medications purchase cheap reminyl on-line, Fisch and colleagues reported long-term outcomes with the Mainz Sigma pouch (Fisch et al medicine 5000 increase order 8 mg reminyl overnight delivery, 1996) medications you can take while breastfeeding buy generic reminyl 4mg line. This was designed to reduce intracolonic pressures and to maintain higher fecal continence. The resultant incontinence with balanced posterior outlet resistance not solely preserves renal operate but also stimulates bladder development. Typically, epispadias restore is now carried out at around 6 months of age, after testosterone stimulation. Bladder neck restore usually occurs when the child is four to 5 years of age, has an enough bladder capability, and, most necessary, is prepared to take part in a postoperative voiding program. Erlangen Approach the Erlangen strategy is clearly essentially the most developed of any of the primary closure strategies. In the Erlangen strategy, developed by Schrott and popularized by Rosch, if the bladder template is deemed of sufficient size, the "complete" restore is completed at eight weeks of age. If the template is too small at birth, the bladder only is closed with bilateral groin exploration, closure of the pubis, epispadias repair, and no osteotomy. In the traditional Erlangen total repair, the bladder is closed together with bilateral reimplantations, bladder neck plasty, bilateral groin exploration, epispadias restore, pubic closure, no osteotomy, and an epidural catheter for 5 days. Thus, the Erlangen repair is really a complete restore, encompassing all phases of exstrophy repair in one setting (Schrott et al, 1984). A strip of mucosa 2 cm extensive, extending from the distal trigone to nicely below the verumontanum within the male and to the extent of the vaginal orifice in the feminine, is printed for prostatic and posterior urethral reconstruction within the male and sufficient urethral closure in the feminine. The male urethral groove may be adequate, during which case no transverse incision of the urethral plate need be performed for urethral lengthening. If so, the urethral groove is lengthened after the manner of Johnston (1974) or Duckett (1977). An appropriate plane is entered just above the umbilicus, and a aircraft is established between the rectus fascia and the bladder. The umbilical vessels are doubly ligated and incised and allowed to fall into the pelvis. The peritoneum is taken off the dome of the bladder at this level in order that the bladder may be placed deep into the pelvis at the time of closure. The plane is sustained caudally down between the bladder and rectus fascia until the urogenital diaphragm fibers are encountered bilaterally. The pubis is encountered at this junction, and a double-pronged skin hook may be inserted into the bone presently and pulled laterally to accentuate the urogenital diaphragm fibers and assist the surgeon radically incise these fibers between the bladder neck, posterior urethra, and pubic bone. Gentle traction on the glans at this level reveals the insertion of the corporeal physique on the lateral inferior facet of the pubis. These urogenital diaphragm fibers are taken down sharply with electrocautery all the way down to the levator hiatus in the pelvic flooring in their entirety. If the urethral plate is left in continuity, it have to be mobilized up to the extent of the prostate to create as a lot further urethral and penile size as attainable. Penile lengthening is achieved by exposing the corpora cavernosa bilaterally and liberating the corpora from their attachments to the suspensory ligaments on the anterior part of the inferior pubic rami. The broad band of fibers and muscular tissue representing the urogenital diaphragm is indifferent subperiosteally from the pubis bilaterally. Reluctance to free the bladder neck and urethra nicely from the inferior ramus of the pubis strikes the neobladder opening cephalad ought to any separation of the pubis occur throughout therapeutic, thus growing the prospect of bladder prolapse. The mucosa and muscle of the bladder, bladder neck, and urethra are then closed properly onto the penis in the midline anteriorly. The function of this tapering is to barely slim and elongate this unit to permit it to be positioned deeply into the pelvis. The dimension of the opening ought to permit sufficient resistance to aid in bladder adaptation and to prevent prolapse but not enough outlet resistance to trigger upper tract changes. The posterior urethra and bladder neck are buttressed with a second layer of local tissue if attainable. The bladder is drained by a suprapubic nonlatex Malecot catheter for a interval of four weeks. Stents present drainage during the first 10 to 14 days after closure, because swelling brought on by the strain of closure of a small bladder can impede the ureters and provides rise to obstruction and transient hypertension. When the bladder and urethra have been closed and the drainage tubes placed, stress over the higher trochanters bilaterally permits the pubic bones to be approximated simply in the midline. Horizontal mattress sutures are placed within the pubis and tied with a knot away from the neourethra. A V-shaped flap of belly skin at a Chapter139 Exstrophy-EpispadiasComplex 3201 level corresponding to the normal position of the umbilicus is tacked right down to the stomach fascia, and a drainage tube exits this orifice. Before and in the course of the process, the affected person is given broad-spectrum antibiotics in an attempt to convert a contaminated field right into a clear surgical wound. As described by Duckett (1977), the groove is then reduce distal to the verumontanum with continuity maintained between the skinny, mucosal, paraexstrophy non�hair-bearing pores and skin adjoining to the posterior urethra and bladder neck and the skin and mucosa of the penile pores and skin and glans. Flaps in the space of the skinny pores and skin are subsequently moved distally and rotated to reconstruct the urethral groove, resurfacing the penis dorsally. In an effort to lower costs, decrease the morbidity associated with multiple operative procedures, and probably have an result on continence, there has been curiosity in performing single-stage reconstruction or combining procedures in appropriately selected sufferers. This technique was first described by Lattimer and Smith (1966) however was abandoned in the 1970s due to high complication and failure charges. The method was revisited by Gearhart and Jeffs (1991a) for failed exstrophy closures and more recently by Grady and Mitchell for new child sufferers (1999). In the mixed exstrophy and epispadias restore, bladder closure is mixed with the modified Cantwell-Ransley epispadias restore (Gearhart and Mathews, 2000; Baird et al, 2005c). This method can be utilized to each delayed primary closure and failed closures. Results have now emerged in teams of boys present process singlestage reconstruction (bladder closure and epispadias repair) in infancy (Gearhart et al, 1998; Baird et al, 2005c). In our opinion, this system should be restricted to boys of older age (older than 6 months) because of evidence indicating that potential complication of these combined procedures is significant lack of penile and corporeal tissue that makes additional reconstruction problematic (Cervellione et al, 2010). Selection ought to keep in mind phallic size and length, depth of the urethral groove, and dimension of the bladder template in those with delayed primary closures, in addition to perivesical and urethral scarring in those that have undergone a prior failed closure (Gearhart and Jeffs, 1991a; Gearhart et al, 1998; Baird et al, 2005c). Before removal of the suprapubic tube, 4 weeks after surgery the bladder outlet is calibrated by a urethral catheter or a urethral sound to ensure free drainage. A full ultrasound examination is performed to verify the standing of the renal pelves and ureters, and appropriate urinary antibiotics are administered as a result of all patients have reflux after closure. Residual urine is estimated by clamping the suprapubic tube, and specimens for culture are obtained earlier than the patient leaves the hospital and at subsequent intervals to detect infection and make certain that the bladder is empty. If the initial ultrasound examination shows good drainage, higher tract imaging by ultrasonography is repeated three months after discharge from the hospital and at intervals of 6 months to 1 12 months during the next 2 to three years to detect any higher tract adjustments caused by reflux, infection, or obstruction. If a helpful continence interval has resulted from the initial closure, an additional operation for incontinence may not be required; nevertheless, this case is sort of uncommon. After the conversion from exstrophy to full epispadias with incontinence, the bladder gradually increases in capacity as inflammatory adjustments in the mucosa resolve. In a latest giant sequence of 82 sufferers reported by Baradaran and colleagues (2012a), 33 delayed closures had been compared with 59 major closures within the neonatal period. Longitudinal analysis of bladder capacities demonstrated that compared with neonatal closures, bladder capacities have been on common 36 mL smaller in repairs delayed because of small templates and 29 mLsmaller in late referrals. Cystoscopy and cystography at yearly intervals are used to evaluate the diploma of reflux noted in nearly 100% of sufferers and to present an estimate of bladder capability (Gearhart and Jeffs, 1998). Even in a very incontinent patient, bladder capability progressively will increase to a degree at which the bladder can be distended at cystography to its true capacity. This have to be done under anesthesia in younger children because the values obtained differ markedly from those obtained when trying to fill the bladder of a crying, squirming toddler on an x-ray table (Gearhart and Jeffs, 1998). If the bladder has not achieved a capacity of no much less than 30 mL by 1 to 2 years, concern should be voiced to the parents in regards to the general capability of the bladder to undergo a continence procedure. Currently, the best parameters out there to predict total success are the dimensions of the bladder template at start and a profitable major closure with absence of infections. Should bladder outlet resistance be such that urine is retained within the bladder and reflux and ureteral dilation develop with infected urine, it could be essential to dilate the urethra or to start intermittent catheterization (Baker et al, 1999). Sometimes the posterior urethral obstruction can be such that it requires a transurethral incision of the stricture to preserve an adequate posterior urethral outlet. If bladder outlet resistance persists and infections proceed, an antireflux procedure may be required as early as 6 months to 1 yr after initial closure (Mathews and Gearhart, 2003). Because of this problem, some items try ureteral reimplantation at the time of bladder closure, however the numbers of patients treated on this fashion is small (Braga et al, 2010). If extreme upper tract changes happen, surgical revision of the bladder outlet by advancing pores and skin flaps into the orifice or even patching the stricture may be essential to stop scarring and additional obstruction. As talked about previously, transurethral incision of the urethral stricture to obtain a balanced outlet should be tried before surgical revision. Judgment is required to know when to avoid makes an attempt at functional closure and to know when to flip to urinary diversion as a way to preserve renal perform. This change of plan is seldom essential if an enough outlet has been constructed at the preliminary closure and if cautious attention has been paid to the details of follow-up of the bladder and posterior urethra. The posterior urethra ought to be rigorously examined anteriorly for erosion of the intrapubic sew, which may be the reason for the recurrent infections (Baker et al, 1999). If the intrapubic stitch is seen within the posterior urethra, a small suprapubic incision must be made and the stitch ought to be removed, or, if it may be grasped, it should be eliminated transurethrally. Husmann and colleagues (1990) have shown very acceptable levels of higher tract operate after main closure as long as prophylactic antibiotics have been used after preliminary closure and elevated urinary residuals have been stored under 50 mL. The second step of the Kelly restore, which differs from different types of repair, is the unconventional soft-tissue mobilization. This is achieved by making an incision across the old bladder closure and by making parallel incisions on the urethral plate extending proximally to halfway between the ureteric orifices and the verumontanum. This maneuver helps expose the corpora laterally as they move over toward their insertion onto the pubis. The mucosa lateral to the urethra is excised, as is a few of the mucosa of the bladder. The initial lateral extension of the incision exposes the dorsal nerves of the penis and the attachment of the corpora to the pubis. The urethral plate is mobilized from the corporeal our bodies and moved to under them to create a penoscrotal hypospadias. Laterally, the extraperitoneal area behind the rectus is entered and the vas retracted. An incision is made in the superior aspect of the pubis downward, creating a "flake" to which medially is attached the corpora of the penis and remnants of the urogenital diaphragm. The incision is carried through the levator muscles both deeply and anteriorly to where the levators insert on the again of the pubis. When it appears the whole course has been decided, the flake of the pubis is incised totally and the urethral and bladder neck area and muscle tissue are brought collectively without rigidity. Mitchell Repair the Mitchell repair, as in all closures, is finest carried out in the newborn interval. The primary difference is that the urethra is separated from its attachments to the underlying corporeal bodies and pelvic diaphragm during the first stage of the process. Mitchell purports that this permits higher posterior positioning of the bladder neck and posterior urethra into the pelvis. This mixed bladder closure with penile repair was originally thought to be adequate for the patient to obtain urinary continence, however this has been discovered to not be the case in that the majority of those sufferers require bladder neck restore (Gearhart et al, 2005; Shoukry et al, 2009; Gargollo et al, 2011). The closure is begun in the usual style, however the incision is carried out onto the urethral plate, taking care to preserve its blood supply and avoiding corporeal damage. The penis is then disassembled into three components-the right corpus, left corpus, and urethral wedge. During commonplace closure of the bladder, the bladder neck is tailored and the urethra is closed in an attempt to transfer the urethra to the tip of the penis. The repair is very similar within the feminine patient, with care taken to mobilize the bladder neck, urethra, and vagina as a single unit. Once the vessels and bone flake are completely free, the tissues of the penis, bladder neck, and urethraarereconstructed. An improve in bladder capability in patients with extremely small bladder capacities after epispadias repair prompted a change in the administration program (Gearhart and Jeffs, 1989a). In a group of patients with a small bladder capability after initial closure, there was a imply improve of fifty five mL in males only 22 months after epispadias restore. Recent data by Kufner and colleagues (2010) clearly demonstrated better eventual general bladder capacity in patients in whom the epispadias repair was completed earlier than 12 months of life. Because most boys with exstrophy have a considerably small penis and a shortage of obtainable penile skin, all patients bear testosterone stimulation before urethroplasty and penile reconstruction (Gearhart and Jeffs, 1987). Current strategies of epispadias restore in bladder exstrophy are the Cantwell-Ransley restore (1989), the modified Cantwell-Ransley restore (1995), and the penile disassembly method described by Mitchell and B�gli (1996). Regardless of the surgical method chosen for reconstruction of the penis in bladder exstrophy, four key issues should be addressed to guarantee a functional and cosmetically pleasing penis. These considerations are (1) correction of dorsal chordee, (2) urethral reconstruction, (3) glanular reconstruction, and (4) penile pores and skin closure. Data of Silver and associates (1997b) clearly showed that this is more of an obvious lengthening of the penis than a true lengthening because the anterior corporeal our bodies in exstrophy sufferers have 50% much less size than age-matched controls. All remnants of the suspensory ligaments and old scar tissue from the preliminary bladder closure must be excised. Further dissection of the corpora cavernosa from the inferior pubic ramus could be achieved. It is commonly shocking how little is accomplished in freeing the corporeal our bodies from the pubis at the time of initial exstrophy closure (Gearhart, 1991). Chordee Besides lengthening of the urethral groove, dorsal chordee have to be addressed.
All of those problems 7 medications that cause incontinence 4mg reminyl fast delivery, together with infection symptoms 3 days dpo buy discount reminyl 4mg on-line, hydronephrosis fungal nail treatment 8 mg reminyl with amex, calculi medications 1-z cheap 4 mg reminyl overnight delivery, spontaneous perforation medicine 10 day 2 times a day chart 8 mg reminyl fast delivery, and tumor medicine omeprazole cheap 4 mg reminyl free shipping, have been reported after continent diversion in adults if not in youngsters. Because more intestine is often required in continent diversion than bladder augmentation, the incidence of issues might in the end be greater than with easy augmentation. Already, serum modifications of elevated chloride, decreased bicarbonate, and acidosis have been famous in some sufferers after continent diversion (Allen et al, 1985; Ashken, 1987; Thuroff et al, 1987; Boyd et al, 1989; McDougal, 1992a). The most common complication in pediatric continent diversion, thus far, has been stomal stenosis. Stenosis occurs extra commonly on the umbilicus with use of appendix in contrast with tapered ileal segments (Fichtner et al, 1997; Kaefer et al, 1999b). Ardelt and associates, after extensive evaluation (2012), discovered no consensus that a single type of efferent limb is superior and suggested that the choice of method must be individualized according to the case. Preoperative analysis should determine upper tract obstruction or vesicoureteral reflux. Such issues should be corrected at the time of surgical procedure, though low-grade secondary reflux will often resolve spontaneously with correction of bladder dysfunction. It is imperative to present the affected person with an sufficient bladder or reservoir, one able to holding at low strain a urinary volume that shall be produced between voidings or catheterizations. This can be achieved by either augmentation or construction of a continent reservoir utilizing any gastrointestinal phase. If adequate outflow resistance is lacking, it must be created on the bladder neck to stop incontinence. Any affected person undergoing reconstructive surgery for bladder or sphincter dysfunction must be ready and capable of performing intermittent catheterization on a reliable foundation; most will require it routinely. The urothelial lining avoids much of the morbidity associated with intestinal segments. If essential, nevertheless, just about any portion of the lower urinary tract could also be reconstructed or changed using gut. Unfortunately, occasional problems do happen when intestinal segments are used in that manner. Patients after reconstruction require a lifetime of follow-up, and that observation ought to embody careful evaluation of their true quality of life. The most necessary factor in avoiding problems with such complicated pediatric sufferers is the motivation of the affected person and family to obtain a successful end result. The efferent phase in continent urinary diversion: a comprehensive evaluation of the literature. Urinary tract refunctionalization after long-term diversion: a 20 12 months expertise with 177 sufferers. Some such surgery will still be necessary, and the sufferers have to be fastidiously evaluated so that every one problems are identified and addressed. Complications of augmentation in children and comparison of gastrointestinal segments. The gastrointestinal composite urinary reservoir in patients with myelomeningocele and exstrophy: long-term metabolic follow-up. Robot-assisted bladder neck reconstruction, bladder neck sling, and appendicovesicostomy in children: description of approach and preliminary outcomes. Using a serosal trough for fashioning a continent catheterizable stoma: technique and outcomes. Results of the rectus fascial sling and wrap procedures for the therapy of neurogenic sphincteric incontinence. Total continence reconstruction utilizing the bogus urinary sphincter and the Malone antegrade continence enema. Detrusor instability: a delayed complication in affiliation with the bogus sphincter. Treatment of intrinsic sphincter deficiency using autologous ear cartilage as a periurethral bulking agent. Outcomes of bladder neck closure for intractable urinary incontinence in patients with neurogenic bladders. Glutaraldehyde cross-lined collagen in the treatment of urinary incontinence in children. Early and late metabolic alterations in children and adolescents with a Kock urinary reservoir. Evaluation of bone mineral density with dual x-ray absorptiometry for osteoporosis in youngsters with bladder augmentation. Renal operate and upper tract configuration following urinary diversion to a continent ileal reservoir (Kock pouch): a prospective 5 to 11 year observe up after reservoir development. Success of the synthetic urinary sphincter after failed surgery for incontinence. Long-term effects of endoscopic injection of dextranomer/hyaluronic acid primarily based implants for remedy of urinary incontinence in children with neurogenic bladder. Detrusor hyperreflexia as a factor in spontaneous perforation of augmentation cystoplasty for neuropathic bladder. Formation of urothelial constructions in vivo from disassociated cells attached to biodegradable polymer scaffolds. Bladder neck sling for remedy of neurogenic incontinence in kids with augmentation cystoplasty: long-term followup. Colocystoplasty for bladder enlargement and bladder substitution: a examine of late ends in 31 cases. Tissue engineering of bladder utilizing vascular endothelial development issue gene-modified endothelial progenitor cells. Biological response of bladders rendered continent by insertion of synthetic sphincter. Physiologic implantation of the severed ureter or frequent bile duct into the intestine. Outcome of continence procedures in the pediatric patient: a single institutional experience. La "petite vessie" des tuberculeaux genitourinaires: essai de classification place et variantes des cysto-intestinoplasties. Ischemic necrosis: a hypothesis to explain the pathogenesis of spontaneously ruptured enterocystoplasty. Cecal tubularization: lengthening method for creation of catheterizable conduit. Is long-term bladder deterioration inevitable following profitable isolated bladder outlet procedures in kids with neuropathic bladder dysfunction A new approach to bladder augmentation in youngsters: seromuscular enterocystoplasty. New utility of the gastrostomy button for scientific and urodynamic evaluation prior to vesicostomy closure. A comparative research between continent diversion and bladder neck closure versus continent diversion and bladder neck reconstruction in children. Evaluation of bone mineral density after ileocystoplasty in youngsters without myelomeningocele. Alterations within the physiological properties of urinary bladder smooth muscle attributable to bladder emptying against an obstruction. Perforation of the augmented urinary bladder in 9 youngsters and adolescents: importance of cystography. Cecoappendicovesicostomy: conduit-lengthening approach to be used in continent urinary reconstruction. Complications of synthetic urinary sphincter around intestinal segments in reconstructed exstrophy patients. Net calcium efflux from reside bone throughout continual metabolic however not respiratory acidosis. Cecal bladder augmentation with a tapered catheterizable stoma: a modification of the Indiana pouch. Long-term followup and end result of continent catheterizable vesicostomy utilizing the Rink modification. Miniature intravesical urethral lengthening procedure for therapy of pediatric neurogenic urinary incontinence. Endoscopic treatment of vesicoureteric reflux and urinary incontinence: technical issues within the paediatric patient. Early development of adenocarcinoma in a younger lady following augmentation cystoplasty for undiversion. Bladder augmentation: partial detrusor excision to augment the bladder without use of bowel. Early administration of oxybutynin improves bladder operate and medical outcomes with posterior urethral valves. Antegrade and retrograde endoscopic dextranomer/hyaluronic acid bladder neck bulking for pediatric incontinence. Radioactive electrolyte absorption studies of small bowel comparison of different segments to be used in urinary diversion. Seromuscular colocystoplasty lined with urothelium protects canines from acidosis during ammonium chloride loading. Ureteral tissue balloon enlargement for laparoscopic bladder augmentation: survival research. Enteric mucosal regrowth after bladder augmentation using demucosalized intestine segments. Transvaginal sling suspension of the bladder neck in feminine patients with neurogenic sphincter incontinence. Endoscopic injection of bulking agents in youngsters with incontinence: dextranomer/hyaluronic acid copolymer versus polytetrafluoroethylene. Laparoscopic seromyotomy (autoaugmentation) for non-neurogenic neurogenic bladder in a toddler: preliminary case report. Perforation of the augmented bladder in patients present process clean intermittent catheterization. Functional consequence and specific problems of gastrocystoplasty for failed bladder exstrophy closure. Catheterizable serous lined urinary outlet in youngsters and adolescents: a selection when different remedies fail. Adenocarcinoma at the website of ureterosigmoidostomies for exstrophy of the bladder. Is nasogastric tube drainage required after reconstructive surgical procedure for neurogenic bladder dysfunction Is bladder biking helpful within the urodynamic evaluation previous to renal transplantation Elevated intravesical pressure causes arterial hypoperfusion in canine colocystoplasty: a fluorometric assessment. Outcome of the Lima periurethral constrictor in youngsters and adolescents: a European prospective. Modified Young-Dees-Leadbetter bladder neck reconstruction: new ideas about old ideas. Implantation of a model new semiautomatic artificial genitourinary sphincter: expertise with major activation and deactivation in forty seven sufferers. Botulinum toxin A intradetrusor injections in youngsters with neurogenic detrusor overactivity: a systematic literature review. Use of abdomen for reconstruction of the lower urinary tract in patients with compromised renal perform. Transverse retubularized ileum: early scientific experience with a new second line Mitrofanoff tube. Treating neuropathic incontinence in children with seromuscular colocystoplasty and a man-made urinary sphincter. Long-term results of the synthetic urinary sphincter in male sufferers with neurogenic bladder. Salvage continent vesicostomy after enterocystoplasty within the absence of the appendix. Direct (nontunneled) ureterocolonic reimplantation in affiliation with continent reservoirs. The Indiana expertise with synthetic urinary sphincters in kids and young adults. Annual endoscopy and urine cytology for surveillance of bladder tumors after enterocystoplasty for congenital bladder anomalies. Placement of artificial urinary sphincter in youngsters and simultaneous gastrocystoplasty. Localization of bacteriuria in patients with enterocystoplasty and nonrefluxing conduits. Pubovaginal slings for the administration of urinary incontinence in feminine adolescents. Refashioned quick bowel segments for the construction of catheterizable channels (the Monti procedure): early medical expertise. Reconstruction and undiversion of the short or severely dilated ureter: the antireflux ileal nipple revisited. Synchronous adenocarcinoma and transitional cell carcinoma of the bladder associated with augmentation: case report and evaluate of the literature. Long term outcomes of bladder neck reconstruction with out augmentation cystoplasty in youngsters. Decreased linear progress related to intestinal bladder augmentation in youngsters with bladder exstrophy. The worth of intermittent self catheterization within the early administration of traumatic paraplegia and tetraplegia. Endoscopic injection with polydimethylsiloxane for the treatment of pediatric urinary incontinence within the neurogenic bladder: long-term outcomes. Endoscopic remedy of urinary incontinence: long-term evaluation of the outcomes. Use of polydimethylsiloxane for endoscopic remedy of neurogenic urinary incontinence in youngsters. Lower extremity bone mineral density in youngsters with congenital spinal dysfunction. A single-centre long-term end result evaluation of synthetic urinary sphincter placement in youngsters. Long-term analysis of metabolic profile and bone mineral density after ileocystoplasty in youngsters.
Purchase reminyl uk. CDC’s HIV Treatment Works: Ryan’s Story.