Thomas Zgonis, DPM, FACFAS
- Associate Professor, Department of Orthopaedic Surgery
- Chief, Division of Podiatric Medicine and Surgery
- Director, Podiatric Surgical Residency and Reconstructive Foot and
- Ankle Fellowship
- The University of Texas Health Science Center at San Antonio
- San Antonio, Texas
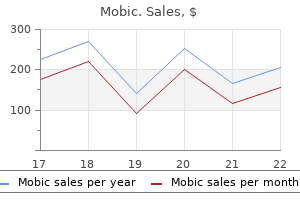
Stereotactic radiotherapy for intracranial nonacoustic schwannomas together with facial nerve schwannoma does arthritis in dogs go away discount mobic online american express. Elective carotid artery resection for superior squamous cell carcinoma of the neck can you have arthritis in your neck 15 mg mobic. Endovascular removable balloon embolization remedy of cavernous carotid artery aneurysms: results in 87 instances arthritis in dogs and walking generic mobic 7.5 mg with mastercard. Treatment of inoperable carotid aneurysms with endovascular carotid occlusion after extracranial-intracranial bypass surgery arthritis at 20 discount 15 mg mobic overnight delivery. Temporary balloon test occlusion of the inner carotid artery: experience in 500 circumstances arthritis in neck care order mobic 15 mg with mastercard. Principles of aneurysm surgical procedure: cerebral ischemic safety arthritis in the knee purchase generic mobic on line, hypothermia, and circulatory arrest. Petrous carotid-tointradural carotid saphenous vein graft for intracavernous large aneurysm, tumor, and occlusive cerebrovascular disease. Surgical therapy of extracranial carotid artery aneurysms: long-term outcomes over a 24-year interval. Extracranial-intracranial bypass for reconstruction of internal carotid artery within the administration of head and neck cancer. Carotid resection and replacement with autogenous arterial graft throughout operation for neck malignancy. Failure of a saphenous vein extracranial-intracranial bypass graft to protect against bilateral center cerebral artery ischemia after carotid artery occlusion: case report. Conduits for cerebrovascular bypass and lessons learned from the cardiovascular experience. Treatment of large intracranial aneurysms with saphenous vein extracranial-to-intracranial bypass grafting: indications, operative method, and results in 29 sufferers. Venous and arterial bypass grafts for troublesome tumors, aneurysms, and occlusive vascular lesions: evolution of surgical treatment and improved graft outcomes. Late patency of lengthy saphenous vein bypass grafts to the anterior and posterior cerebral circulation. Maximizing patency and saphenous vein bypass grafts: ideas of preparation discovered from coronary and peripheral vascular surgery. Results of microsurgical extra-intracranial arterial bypass in the treatment of cerebral ischemia. Possible prevention of brain stem stroke by microvascular anastomosis within the vertebrobasilar system. Occipital artery to posterior inferior cerebellar artery bypass for vertebrobasilar ischemia. Anastomosis of the anterior temporal artery to a secondary trunk of the middle cerebral artery for treatment of an enormous M1 segment aneurysm. End-to-end suture of the posterior inferior cerebellar artery after the excision of a big aneurysm: case report. The microsurgical anterior interhemispheric approach suitably utilized to ruptured aneurysms of the anterior speaking artery within the acute stage. Giant peripheral aneurysm of the posterior inferior cerebellar artery handled with excision and end-to-end anastomosis. End-to-end anastomosis of the anterior cerebral artery after excision of a large aneurysm. Rupture of a large basilar aneurysm after saphenous vein interposition graft to the posterior cerebral artery. Long-term patency of radial artery graft bypass for reconstruction of the interior carotid artery. Midterm medical and angiographic outcomes of radial artery grafts used for myocardial revascularization. These feeders can retract into surrounding mind throughout attempted coagulation and are a known cause of postoperative morbidity. Unfortunately, these feeders typically arise from deep and perforating feeding arteries that may be difficult to catheterize and are also associated with greater danger of issues on account of possible reflux of embolic material into branches feeding eloquent areas. Several modern collection have detailed outcomes and issues of preoperative adjunctive embolization for microsurgery (Table 398-1). Among the sufferers who underwent preoperative embolization, seven experienced hemorrhage before surgical procedure. Among those sufferers, 10% of those who had undergone embolization and 36% of those who had undergone surgical procedure experienced nondisabling neurological deficits. Disabling deficits have been seen in 2% and 3% of postembolization and postsurgical sufferers, respectively. Similarly, among the prospectively adopted sufferers of the multicenter Scottish Audit of Intracranial Vascular Malformations, 34% (35/103) underwent multimodality therapy: 12 sufferers undergoing adjunctive embolization for microsurgery, 20 present process mixed embolization and radiosurgery, 2 patients undergoing microsurgery and radiosurgery, and 1 patient undergoing all forms of remedies. Preoperative embolization may additionally be useful in eliminating high flow via direct fistulous connections. D, Post-embolization lateral angiogram exhibits nidal reduction underneath the difficult-to-reach nidus underlying the big venous outflow. These outcomes counsel that as particular person surgeon expertise will increase, embolization may turn into useful. With developments in embolization techniques and supplies, one therapeutic technique has accordingly developed to reducing the dimensions of the nidus via embolization, making it extra amenable to subsequent radiosurgical treatment. No convincing studies have proved this technique to be efficient, and embolization in preparation for radiosurgery, though extensively utilized, is controversial. The researchers of this study found that a nidus volume larger than 8 cm3 was associated with greater posttreatment threat of hemorrhage. No difference between the two teams was seen within the 2% annual rate of hemorrhage after radiosurgery. They hypothesized that this reduction in radiation-induced neurological deficits might be as a result of aid of venous congestion induced by radiosurgery. The problems of embolization included stroke or severe incapacity in 5 patients and dying after hemorrhage in three. A staged multimodality remedy plan was utilized in 51 patients: embolization and surgery in 5, embolization and radiosurgery in 23, and embolization, microsurgery, and radiosurgery in 23. Eight patients died following their treatments, 5 of whom experienced hemorrhages. Four hemorrhages were reported within the interval, with surgical procedure following a mean of 5. Large single-institution collection provide some proof of the protection and efficacy of adjunctive embolization for microsurgery and radiosurgery (Table 398-2; see additionally Table 398-1). A, A proper ophthalmic aneurysm was noted on the lateral angiogram obtained following an intraparenchymal hemorrhage (arrow). Follow-up angiography for this whole series demonstrated 68% obliteration and 24% circulate discount rates with three treatment failures. Radiologic follow-up demonstrated obliteration in 12 of 15 patients and circulate reduction in the remaining three. In order to preserve the security of the process, only particles with a diameter greater than a hundred and fifty �m are used, to stop migration of the embolic materials by way of the small "dangerous" externalinternal and external-vertebral collateral pathways. It can also be attainable, although unproven, that embolization of the most important exterior carotid artery feeders could improve the effectiveness of radiosurgery in obliterating the fistula, by eliminating high-flow feeders to the lesion. Partial coiling (leaving residual aneurysm neck) may be a reasonable technique in choose circumstances of ruptured aneurysms or extreme vasospasm during which the affected person has a poor scientific condition or grave prognosis. A, She was referred to our establishment after partial ethylene vinyl alcohol copolymer (Onyx) embolization (arrow, inset). Polyvinyl alcohol particle embolization was carried out to palliate her signs and cut back total move via the fistula. B, Follow-up angiography confirmed diminished circulate from the occipital and posterior auricular arteries. Staged radiosurgery with a marginal dose of 16 Gy and a maximum dose of 32 Gy was carried out 2 days later. C and D, the 3-year follow-up angiogram confirmed full resolution of the fistula (C), and she had a superb clinical consequence, with preservation of the patency of the ipsilateral sinus (D). Despite their appeal, these planned mixed methods have gotten much less and fewer frequent as newer endovascular methods have been developed to take care of aneurysms once thought-about unsuitable for major endovascular remedy. Nowadays, the more widespread situation in which a multimodality strategy to intracranial aneurysms is utilized is after failure of major endovascular or surgical therapy. Neurosurgeons are sometimes confronted with the issue of recurrent aneurysms after major coiling. In the early days, coil extraction adopted by aneurysm clipping was the primary strategy. This strategy makes use of the upper closing force adjoining to the fenestration, akin to the clipping of calcified aneurysms. The major issues for surgical therapy of a previously coiled aneurysm are the presence or absence of a residual neck and the time elapsed from the final embolization. Stereotactic radiosurgery for arteriovenous malformations after embolization: a case-control study. Multimodality remedy of intracranial dural arteriovenous fistulas within the Onyx era: a single middle experience. Microsurgery for cerebral arteriovenous malformations: postoperative outcomes and predictors of issues in 264 cases. Determinants of staged endovascular and surgical treatment consequence of mind arteriovenous malformations. Role of surgery in the management of mind arteriovenous malformations: potential cohort examine. Letter: Intracranial cyanoacrylate: a model new catheter therapy for arteriovenous malformation. Stereotactic radiosurgery with and without embolization for intracranial arteriovenous malformations: a scientific evaluate and meta-analysis. Effect of prior embolization on cerebral arteriovenous malformation radiosurgery outcomes: a casecontrol study. Combined endovascular embolization and stereotactic radiosurgery in the therapy of huge arteriovenous malformations. Stereotactic radiosurgery with neoadjuvant embolization of larger arteriovenous malformations: an institutional expertise. Deep arteriovenous malformations in the basal ganglia, thalamus, and insula: multimodality administration, patient selection, and results. Radiosurgery facilitates resection of mind arteriovenous malformations and reduces surgical morbidity. Changing medical and therapeutic trends in tentorial dural arteriovenous fistulas: a systematic evaluate. Results of mixed stereotactic radiosurgery and transarterial embolization for dural arteriovenous fistulas of the transverse and sigmoid sinuses. Safety and efficacy of microsurgical therapy of beforehand coiled aneurysms: a scientific evaluation and meta-analysis. Neurosurgical administration of cerebral aneurysms following unsuccessful or incomplete endovascular embolization. Treatment for brain arteriovenous malformation within the 1998-2011 interval and evaluation of the literature. Multimodality treatment of brain arteriovenous malformations with microsurgery after embolization with Onyx: single-center expertise and technical nuances. Alexander West Traumatic intracranial aneurysms could additionally be the outcome of both penetrating or nonpenetrating trauma. Traumatic cerebral aneurysm has even been reported within the pediatric affected person in a case of shaken baby syndrome. South Africa has supplied a lot of the literature with regard to low-velocity injuries, which are prevalent on this region; stab wounds to the mind account for as a lot as 6% of all trauma admissions. The aneurysm can result immediately from harm to an underlying vessel by depressed bone fragments or dispersion of bone fragments attributable to a penetrating harm. With regard to missile accidents, conflicts in Lebanon, Iraq, and Iran have demonstrated aneurysm formation in zero. The incidence is expounded to velocity: lower velocity shrapnel injuries cause the next incidence of aneurysm formation than do higher velocity bullet accidents. The aneurysm confirmed lack of the interior elastic lamina and easy muscle in the media and a rise in measurement of the adventitia. True aneurysms reveal outpouching of the intima through the media, along with fragmentation of the interior elastic membrane; as a result, the aneurysm wall consists of intima separated from the adventitia by fibrous tissue. In contrast, false aneurysms, which constitute the majority of traumatic intracranial aneurysms, are essentially contained hematomas with disruption of all three layers of the vessel wall. The more inclusive time period pseudoaneurysm is often used to describe aneurysms associated to trauma. Traumatic aneurysms occur distally in the vascular tree, in distinction to the proximal bifurcation site of saccular aneurysms. The anterior circulation is most often affected; the peripheral branches of the middle cerebral artery are essentially the most frequent site, adopted by branches of the pericallosal vessels. For example, traumatic aneurysms are 14 instances more prone to develop with shrapnel injuries than with bullet injuries, which are of upper velocity. Bullets with larger velocity and thus larger kinetic harm are extra doubtless to rupture a vessel than merely damage the wall. Traumatic fistulas are abnormal connections between the intracranial arterial and venous circulation that can happen after extreme or even comparatively minor nonpenetrating trauma. On event, they result from penetrating trauma, the most common location being the cavernous sinus with the formation of a carotid-cavernous fistula: an acquired communication between the intracranial carotid artery and the cavernous sinus. In this sort of fistula, the irregular communication between the intracranial arterial and venous circulation lies inside the dura. The findings are from a patient who suffered a severe traumatic brain harm with bilateral cranium fractures that necessitated evacuation of a subdural hematoma on the proper. A, Sagittal computed tomographic angiogram exhibiting a largely thrombosed traumatic aneurysm in the left frontal area. B, Cerebral angiogram demonstrating a traumatic aneurysm in the distal left middle cerebral artery pial artery (arrow).
First arthritis problem means order generic mobic on-line, massive branches of the external carotid artery rheumatoid arthritis diet to loss weight purchase mobic overnight delivery, ideally the inner maxillary artery or occipital artery arthritis pain when sleeping mobic 7.5mg discount, ought to be used for exchange maneuvers can arthritis in neck cause lightheadedness purchase mobic 7.5 mg on-line. Second arthritis in neck and shoulder symptoms 7.5mg mobic overnight delivery, rupture of a department of the carotid artery can result in psoriatic arthritis in feet order mobic 15mg otc life-threatening airway emergencies. A doctor who can intubate the patient or carry out an emergency tracheostomy to establish an airway must be readily accessible. Third, carotid interventionists must be snug with microcatheters and embolic brokers corresponding to n-butyl cyanoacrylate, coils, silk, Gelfoam (Pfizer, New York), and even autologous clot as a means to stop bleeding from vessel perforations. Although a uncommon occasion, perforation of a department of the external carotid artery can quickly result in airway compromise if not recognized and handled promptly. An equally rare occasion is external carotid artery embolism to carotid ophthalmic collateral vessels, which may lead to retinal embolism and blindness. Anatomically, this could occur by way of a number of avenues: (1) middle meningeal and superficial temporal collateral vessels to the ophthalmic artery, (2) after inner carotid artery reconstitution, and (3) retrograde embolization by way of the external carotid artery to ophthalmic and retinal AorticorBrachiocephalicAccess In the method of obtaining entry to the widespread carotid artery with a information catheter, injury to any of the main aortic branches and brachiocephalic vessels can occur and end in dissection, thrombotic occlusion, embolic infarction, or a mix of those. Many patients with carotid stenosis have severe atherosclerotic particles throughout their arterial timber. Therefore, care should be taken in obtaining entry to the proximal carotid artery. Minor, non�flow-limiting dissections of the proximal brachiocephalic vessels can be observed, regardless of whether the patient is receiving a heparin infusion. If it is a concern, however the decision is made not to place a stent in a dissection flap, repeated angiography within 24 hours may be indicated. If wire access is misplaced, a microcatheter and a gentle wire could additionally be used to locate the distal true lumen, with angiography carried out via the microcatheter to be positive that the distal wire is certainly within the true lumen. If a sudden neurological change develops, the diagnosis ought to embrace hemorrhage and ischemia (most usually brought on by embolism). The surgeon ought to obtain rapid access to the vessel suspected of harboring the problem, according to the findings of the neurological examination. If loss of vision happens, angiography should be carried out immediately to determine the placement of the occlusion. Central retinal artery occlusions can generally be treated by direct infusion of antiplatelet brokers into the ophthalmic artery. Chen and associates115 demonstrated a excessive fee of microemboli detection, particularly throughout distal filter deployment (>8000 microemboli) and stent deployment (>7000 microemboli). However, using a distal embolic safety device significantly lowered the frequency of Doppler study�detected microembolic signal. The indication or indications for proximal versus distal protection use have but to be clearly outlined. This suggests that proximal safety may be safer in patients with hypoechoic plaques. If the true lumen can be entered with the distal embolic protection device, it ought to be crossed and stented along with the stenosis. Then the true lumen could be recognized with a microcatheter angiographic run, and the safety system may be introduced into position. Contrast materials remaining within the arterial wall ought to cause concern for dissection. For circumstances of small, asymptomatic, and non�flow-limiting dissections, scientific statement is really helpful. Rapid entry to the distal intracranial vasculature enables embolectomy or direct delivery of pharmacologic remedy, or each. In addition, as said previously, if crossing a lesion continues to be troublesome or impossible, the procedure should be reassessed and endarterectomy thought-about. Ideally, the filter ought to be deployed in a straight section of the interior carotid artery distal to the stenosis and nicely against the carotid wall. Most usually, this occurs when the operator advances the wire but not the housing sheath of the distal embolic safety system. In this case, the distal embolic safety device must be recaptured and redeployed distally. In these instances, pushing the filter back into the internal carotid artery and above the lesion is commonly a better choice than dragging the whole system by way of the lesion. An alternative technique for retrieval is to exchange the preliminary distal embolic protection device sheath for a 4 French angled catheter up the wire, utilizing it to recapture the misdeployed system. Filter devices have been sheared off during recapturing, which has resulted in distal embolization of the filter and its contents. In these dire settings, relying on the situation, choices include snare retrieval into the information catheter, stenting to anchor the filter against the vessel lumen, or operative retrieval. Filter location within the bony/skull base segments of the internal carotid artery might make operative retrieval unimaginable. However, earlier than any retrieval maneuvers are undertaken, the surgeon ought to consider quickly arresting circulate to avoid additional distal intracranial embolization. Carotid vasospasm may happen, notably when the distal embolic safety filter undergoes important motion or in cases during which a kink has been introduced. Typically, this stays clinically and angiographically inconsequential; nonetheless, stroke has been described in conjunction with sudden extreme spasm immediately after the deployment of an AngioGuard embolic safety system. Rather, the operation should be completed and the filter recaptured in the regular method. Spasm related to a vessel kink attributable to filter placement typically resolves when the device is recaptured. In flow-limiting conditions or if significant time has handed and the spasm persists, intra-arterially administered nitroglycerin (100200 �g) or verapamil (5-10 mg) is usually efficient. These pharmacologic injections could potentiate any ongoing hypotension; intravenous pressors should be at hand to keep normotension if essential. Particular attention ought to be paid to blood pressure reduction throughout angioplasty due to the carotid baroreceptor response. Patients with baseline heart charges of less than 70 beats per minute could benefit from 0. Postdilation angioplasty also is related to a excessive risk for each embolic phenomena and one or more extreme baroreceptor responses. In the case of postdilation angioplasty, the balloon size is chosen according to the measurement of the stent in the distal inside carotid artery. It is necessary to remember that atropine may alleviate severe bradycardia however has little effect on hypotension. When problem is encountered, however, dissections, stent movement, and shearing of the filter system can occur. Difficulty during recapturing is most commonly skilled after deployment of an open-cell stent or when the filter is situated in a tortuous vessel or on a big curve. We have employed the following systematic approach for recapturing the distal embolic safety system and have discovered that it generally proves profitable: 1. Advancing the information catheter into the stent, which will bias the wire away from the stent wall, thereby allowing the recapture sheath to pass 2. If the sheath is impeded by a stent tine, redilation with a bigger balloon or spinning the sheath with ahead pressure, which helps flatten the tine or allows passage of the sheath four. If other maneuvers fail, passing a 4 or 5 French angled glide catheter over the distal embolic safety device wire and using it to seize the filter Stent-AssociatedComplications Immediate complications related to stenting are uncommon. With dual antiplatelet therapy for 12 weeks and with arteries bigger than 3 mm, acute and subacute thrombosis is unusual. According to the cardiology literature, early stent thrombosis in all probability outcomes from a dissection unrecognized throughout therapy or an undersized or expanded stent; late thrombosis in all probability results from mismatch of the stent to the artery, from hypersensitivity, from abnormal endothelialization, or from poor compliance with the antiplatelet treatment routine. Some diploma of irregular endothelialization was most likely present in this case, and a hypercoagulable state could have been implicated. A twin antiplatelet routine 12 weeks after the process and lifetime aspirin use appear important for maintaining stent patency. If arterial occlusion occurs acutely in the course of the process, the analysis includes extreme spasm, dissection, thrombosis from plaque or platelet aggregation, and filling of a filter with embolic materials. If the filter is full of embolic debris, a utility catheter can be utilized to carry out a suction thrombectomy. The filter ought to be rigorously captured and introduced via the stent in order to not disturb the captured particles. We achieve this by incompletely capturing the filter so as to enable its passage by way of the stent however to not squeeze out the captured embolic particles. Successful outcomes were reported for a small collection of patients undergoing operative rescue after acute or subacute stent thrombosis. Intracranial Complications the intracranial problems of carotid stenting can arise from massive vessel occlusion, shower of emboli, and hemorrhage. All three sources should be thought of in a affected person with an acute or delayed neurological change not defined at the cervical degree. In the acute setting, cerebral angiography should be performed to look for vessel cutoff or gradual circulate. If a large vessel cutoff can be seen clearly, the surgeon ought to immediately attempt to recanalize the occluded vessel. One possibility is to use a stent retriever as the preliminary maneuver to obviate the need for additional exchange maneuvers. Intracranial hemorrhage can manifest as sluggish move; it might appear as a bathe of emboli earlier than enlargement of the hematoma or the development of great mass impact. During this time, strict blood pressure control is crucial to keep away from hemorrhagic complications; we usually keep systolic blood strain at lower than 160 mm Hg. Evacuation should be thought of within the setting of life-threatening hematomas in neurologically salvageable patients. Most intracranial hematomas broaden within the first 12 hours124; due to this fact, careful monitoring is important throughout this period. Hemorrhage that occurs after the process, particularly when the treated vessel previously was severely stenotic, might end result from reperfusion injury. The source of reperfusion hemorrhage stays debatable: some authorities imagine in a hyperperfusion origin, whereas others have advised hemorrhagic conversion of a bathe of emboli. On occasion, a affected person presents with an intracranial aneurysm ipsilateral to a critically extreme carotid stenosis. An exhaustive evaluation of contrast-induced nephropathy128 gave a few practical pointers for renal prophylaxis in sufferers with preexisting elevated creatinine ranges: hydration with regular saline for 2 to 12 hours at a degree of 1 mL/kg/hour before administration of contrast materials and using low doses of lowosmolar distinction agents (such as iodixanol). Doses larger than 5 mL/kg of physique weight divided by serum creatinine stage are related to higher risk. Dissection Carotid artery dissections can happen spontaneously, after seemingly minor trauma. The dissection flap could trigger a significant lower in flow, leading to thrombus or occlusion, or both; conversely, it could result in delicate stasis of contrast materials with primarily regular hemodynamics. Traditionally, carotid artery dissection has been treated with heparin and warfarin therapies for 2 causes: most sufferers in giant retrospective series have done well with these drugs, and little else was available till the maturation of methods for carotid stenting because the early 2000s. An aortic arch run with a 5 French pigtail catheter can often assist identify the proximal extent of the dissection. The wire should move easily into the true lumen; resistance means that the wire or catheter is in the false lumen. When this happens, the microcatheter system must be brought well again into the proximal regular artery and then access of the true lumen must be reattempted. Once access to the distal true lumen is obtained, the distal anatomic boundaries of the dissection can be recognized. For dissections extending into the intracranial compartment, solely balloon-mounted cardiac stents had been traditionally available. Acute aortic dissection with nice vessel involvement carries a high mortality price with medical and surgical administration. Systemic Complications Systemic complications of endoluminal carotid intervention embrace seizures, myocardial infarction, contrast-induced nephropathy, and allergy to contrast materials. If a affected person has a seizure throughout angiography, attention ought to first be paid to basic life assist and pharmacologic seizure management, which encompass the establishment of an airway and administration of lorazepam (2 mg) and a phosphenytoin loading dose (18-20 mg/kg of physique weight). The differential analysis consists of embolism (air, necrotic debris), ischemia from vessel occlusion or vasospasm, intracranial hemorrhage, hyperperfusion, and sensitivity to distinction material (this is much less frequent with agents with a decrease osmolar load). Standard measures, including nitrate infusion, beta blockade, and heparin administration, must be initiated if a myocardial infarction happens. A cardiologist must be consulted early because sufferers in whom Q-wave infarction is seen on the electrocardiogram often require acute revascularization. Acute allergy to distinction material is another setting by which airway security is paramount. Methylprednisolone (120 mg given parenterally) and epinephrine (1 mg) are administered as necessary. Patients with identified allergic reactions to distinction media are treated with 30 mg of prednisone at 12 hours after which 1 hour earlier than the procedure, along with 50 mg of diphenhydramine (Benadryl). However, sufferers can develop secondary dissections and symptomatic stenosis that necessitate remedy. A secondary dissection usually tracks high in the cervical section of the carotid artery, inhibiting filter placement in this area. The determination to treat such sufferers ought to be fastidiously weighed towards the risks of additional vessel dissection. IntraluminalThrombus Intraluminal thrombus of the inner carotid artery is an ominous lesion, carrying a high threat of stroke. In patients with intraluminal thrombus, the 1-year dangers of stroke for those surgically handled and people medically handled were 16% and 25. In these patients, Jahromi and associates placed a PercuSurge balloon outside the guide sheath in the exterior carotid artery and then positioned a balloon information in the common carotid artery and followed this with move reversal, which was used to cross the intraluminal thrombus with yet another PercuSurge balloon placed within the distal cervical inner carotid artery. Therefore, with these vessels beneath complete move arrest, they placed a stent throughout the thrombus.
Cheap mobic. Point name dish effective remedies arthritis medicine.
Relationship of perfusion strain and dimension to risk of hemorrhage from arteriovenous malformations arthritis pain cannabis discount 15 mg mobic amex. Association of infratentorial brain arteriovenous malformations with hemorrhage at preliminary presentation arthritis neck visual disturbance 7.5 mg mobic amex. Epilepsy related to cerebral arteriovenous malformations: a multivariate analysis of angioarchitectural traits zen arthritis spray order genuine mobic. Cerebral arteriovenous malformations and epilepsy: components within the development of epilepsy arthritis in back lumbar discount mobic 7.5 mg visa. Effects of cerebral angiomas on perifocal and distant tissue: a multivariate positron emission tomography examine arthritis in back and ribs discount 15mg mobic overnight delivery. Comparison of two approaches for figuring out the natural history danger of brain arteriovenous malformation rupture arthritis in back and neck purchase generic mobic line. Longitudinal risk of intracranial hemorrhage in patients with arteriovenous malformation of the brain inside a defined inhabitants. Angioarchitectural factors current in mind arteriovenous malformations related to hemorrhagic presentation. Seizure threat from cavernous or arteriovenous malformations: potential population-based examine. Angiographic follow-up examine of cerebral arteriovenous malformation close to their enlargement and progression. Unruptured intracranial aneurysms and vascular malformations: frequency of intracranial hemorrhage and relationship of lesions. Outcome following hemorrhage from mind arteriovenous malformations at presentation and during follow up: is it worse than we expect Intracranial hemorrhage from aneurysms and arteriovenous malformations throughout being pregnant and the puerperium. Current therapy options for cerebral arteriovenous malformations in pregnancy: a evaluation of the literature. Exceptional multiplicity of cerebral arterniovenous malformations related to hereitary hemorrhagic telangiectasia (Osler Weber Rendu). Appearance of a cavernous hemangioma within the cerebral cortex after a biopsy of a deeper lesion. Progression of a number of cryptic vascular malformations associated with anomalous venous drainage. The affiliation of venous developmental anomalies and cavernous malformations:pathophysiological, diagnostic, and surgical issues. A gene liable for cavernous malformations of the brain maps to chromosome 7q. Clinical, radiological, and pathological spectrum of angiographically occult intracranialvascular malformations. Value of gradient-echo magnetic resonance imaging within the prognosis of familial cerebral cavernous malformation. Dynamic permeability and quantitative susceptibility: related imaging biomarkers in cerebral cavernous malformations. The web site, construction and frequency of intracranial aneurysms, angiomas and arteriovenous abnormalities. Untreated scientific course of cerebral cavernous malformations: a prospective, population-based cohort examine. Seasonal variation in hemorrhage and focal neurologic deficit as a end result of intracerebral cavernous malformations. Report of four circumstances and discussion of the pathophysiological, diagnostic, and therapeutic implications. Cavernomas of the central nervous system: scientific and neuroimaging manifestations in forty seven sufferers. Early radiologically proven rebleeding from intracranial cavernous angiomas: report of 6 instances and evaluation of the literature. A comparison of the medical profile of cavernous malformations with and without associated venous malformations. Predictive elements for intracerebral hemorrhage in patients with cavernous angiomas. Spectrum of genotype and scientific manifestations in cerebral cavernous malformations. Factors predisposing to clinical incapacity in sufferers with cavernous malformations of the brain. Recurrent intraparenchymal hemorrhages from angiographically occult vascular malformations. Clinical shows of vascular malformations of the brain stem: comparability of angiographically optimistic and adverse sorts. Intracranial cavernous angioma initially presenting in pregnancy with new-onset seizures. Etiological analysis of dural arteriovenous malformations of the lateral and sigmoid sinuses primarily based on histopathological examinations. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for therapy. Superselective arteriographic embolization by the femoral route in neuroradiology. Borden-Shucart Type I dural arteriovenous fistulas: clinical course together with danger of conversion to higher-grade fistulas. Diffuse capillary telangiectasia of the brain manifested as a slowly progressive course. Arteriovenous malformation affecting the transverse dural venous sinus an qcquired lesion. Intracranial dural arteriovenous fistulas with or without cerebral sinus thrombosis: evaluation of sixty nine sufferers. Meningioma in sigmoid sinus groove related to dural arteriovenous malformation: case report. Post-traumatic arteriovenous fistula between the exterior carotid arteries and the superior longitudinal sinus: report of a case. Two cases of dural arteriovenous malformation occurring after intracranial surgery. Thrombophilic abnormalities among sufferers with cranial dural arteriovenous fistulas. Natural historical past, present concepts, classification, elements impacting endovascular remedy, and pathophysiology of cerebral and spinal dural arteriovenous fistulas. Intracranial hemorrhage from dural arteriovenous fistulas: clinical features and outcome. Dural arteriovenous fistulas with cortical venous drainage: incidence, scientific presentation, and therapy. The natural history of cranial dural arteriovenous fistulae with cortical venous reflux-the significance of venous ectasia. Cranial dural arteriovenous fistulas: modification of angiographic classification scales primarily based on new natural historical past information. Benign cranial dural arteriovenous fistulas: consequence of conservative administration based mostly on the pure historical past of the lesion. Venous angiomas of the posterior fossa should be considered as anomalous venous drainage. Association of developmental venous anomalies with perfusion abnormalities on arterial spin labeling and bolus perfusion-weighted imaging. Angiography and computed tomography in the evaluation of cerebral venous malformations. The radiological analysis of cerebral venous angioma: cerebral angiography and computed tomography. Regional parenchymal enhancement with blended cavernous/venous malformations of the brain. Assocation of venous and true arteriovenous malformation: a rare entity amongst mixed vascular malformations of the brain. Venous angiomas with arteriovenous shunts: report of three circumstances and review of the literature. Developmental venous anomaly, cavernous malformation, and capillary telangiectasia: spectrum of a single disease. The association between cerebral developmental venous anomaly and concomitant cavernous malformation: an observational examine utilizing magnetic resonance imaging. The angioarchitectural factors of the cerebral developmental venous anomaly: can they be the causes of concurrent sporadic cavernous malformation Venous malformation of the aqueduct of Sylvius handled by interventriculostomy: 15 years follow-up. Intracerebral haemorrhage from a venous angioma following thrombosis of a draining vein. Thrombosis of a developmental venous anomaly causing venous infarction and pontine hemorrhage. Rapidly progressive hippocampal atrophy: evidence for a seizure-induced mechanism. Cerebellar venous angioma related to angiographically occult mind stem vascular malformation: report of two cases. Surgical extirpation of a venous angioma of the medulla oblongata simulating a quantity of sclerosis. Cerebellar infarct attributable to spontaneous thrombosis of a developmental venous anomaly of the posterior fossa. Venous infarction from a venous angioma occurring after thrombosis of a drainage vein. Slow-flow vascular malformation of the pons: congenital or acquired capillary telangiectasia. Asymptomatic radiation-induced telangiectasia in youngsters after cranial irradiation: frequency, latency, and dose relation. Capillary telangiectasias: clinical, radiographic, and histopathological features. Clinically aggressive diffuse capillary telangiectasia of the brain stem: a clinical radiologicpathologic case study. Symptomatic unruptured capillary telangiectasia of the brain stem: report of three instances and evaluation of the literature. Intracerebral capillary telangiectasia and venous malformation: a uncommon affiliation. The potential of capillary birthmarks as a big marker for capillary malformationarteriovenous malformation syndrome in children who had nontraumatic cerebral hemorrhage. Racial/ethnic variations in longitudinal danger of intracranial hemorrhage in brain arteriovenous malformation sufferers. Grading venous restrictive disease in patients with dural arteriovenous fistulas of the transverse/ sigmoid sinus. Walter Dandy declared that to "extirpate considered one of these aneurysmal angioma in its lively state would be unthinkable. The limited high-class proof for a most well-liked management pathway accentuates the issue of choices. Competence and experience of the medical group, availability of technical assist, and, importantly, the wishes of the patient all must be considered. For some sufferers, no deficit is the precedence; for others, avoidance of dying is the precedence. These priorities have to be mentioned with the affected person and thought of with regard to the pathway of management. Further discussions associated to these matters are covered in Chapters 403, 404, 405, 406, and 269. To guide which management pathway to advocate, a stepwise determination process is undertaken. The ideas guiding this course of contain a negotiation between efficient obliteration with inherent risks and affected person safety. Furthermore, as a end result of surgery presents a speedy and definitive path to remedy, the surgical dangers are thought-about before other obliteration treatments. Finally, alternate and ancillary treatments with focused irradiation and embolization need to be understood. To know the true danger of surgery, each type of process would have to be carried out and included in the analysis. Therefore, providing a single point estimate primarily based on results (a helpful metric to evaluate and to benchmark performance among treating centers) may not be one of the only ways of conveying data to sufferers. However, we will calculate from our expertise the vary inside which the danger is prone to fall. Biasing the danger to emphasize danger or, alternatively, an excessively optimistic end result might dissuade sufferers from choosing the management choice that most precisely fits them. Of course, the important thing to having the flexibility to present this info is that steady audit is rigorously maintained by the surgeon and the team. Such conservatism could embrace considering alternative administration pathways or referral to a specialised neurovascular center. Gross and Du, in a meta-analysis of risk of future hemorrhage, concluded that the annual fee of future hemorrhage was 2. Gross and Du concluded that previous hemorrhage, deep location, completely deep venous drainage, and associated aneurysm had been statistically important elements growing the chance of subsequent hemorrhage. This is as a end result of the elevated danger associated with these characteristics among the various studies was inconsistent; the subgroup evaluation was carried out with a low event price; and the number in danger for every of these subgroups was small after a short time period. This may account for each the elevated fee of hemorrhage in older patients and an absence of an aneurysm effect past the primary 12 months found in the examine by Kim and colleagues. That aneurysms are prone to remain a risk for hemorrhage past 12 months has been instructed by earlier studies22,23 during which treating groups had been largely na�ve to the impact of aneurysms, in addition to by recent proof for the continuing higher risk of hemorrhage with the presence of aneurysms as seen through the latent interval after initiation of radiosurgery. The 95% confidence intervals (calculated by modified Wald technique) are supplied for the end of the 25-year interval. This is overlaid with the cumulative instances undergoing preoperative embolization (dotted red line).
This situation forces predominant reliance on data obtained from the therapy of a more heterogenous and likely extra sophisticated group of aneurysms as a baseline can arthritis in feet cause swelling order mobic 7.5mg without prescription. When faced with an aneurysm recurrence what does arthritis in fingers look like cheap mobic 15mg amex, the surgeon should initially determine whether or not the aneurysm is massive sufficient to be a candidate for re-treatment arthritis in knee worse at night discount mobic 15 mg amex. Then she or he should weigh the attendant risks of re-treatment in opposition to the perceived danger of aneurysm rupture degenerative arthritis in neck and back buy mobic 7.5mg. Given related charges of main aneurysm recurrences arthritis flare up purchase 15mg mobic otc, North American centers had the next fee of re-treatment (21% in ruptured aneurysms arthritis pain relief walgreens order generic mobic online, 10. Angiographic outcomes are the subject of much scrutiny due to the idea that full occlusion of an aneurysm mitigates the chance of hemorrhage. Unfortunately, recurrences and/or rehemorrhages can occur in aneurysms that were initially thought to be fully occluded. Primary coil embolization remains the preferred methodology of endovascular treatment of those aneurysms and is the muse on which extra sophisticated treatments are primarily based. Selection of cerebral aneurysms for treatment utilizing Guglielmi detachable coils: the preliminary University of Illinois at Chicago experience. Endovascular therapy of posterior circulation aneurysms by electrothrombosis utilizing electrically detachable coils. Intravascular stent and endovascular coil placement for a ruptured fusiform aneurysm of the basilar artery. Natural historical past of unruptured intracranial aneurysms: Probability of and threat factors for aneurysm rupture. Endovascular occlusion of intracranial aneurysms with Guglielmi detachable coils: Correlation between coil packing density and coil compaction. Lifelong rupture risk of intracranial aneurysms is dependent upon threat components: A potential finnish cohort research. Cerecyte coil trial: Angiographic outcomes of a prospective randomized trial comparing endovascular coiling of cerebral aneurysms with both Cerecyte or bare platinum coils. Balloon-assisted coil embolization of intracranial aneurysms: incidence, issues, and angiography results. Unruptured intracranial aneurysms: risk of rupture and dangers of surgical intervention. Endovascular remedy of fusiform aneurysms with stents and coils: technical feasibility in a swine model. Curative cerebrovascular reconstruction with the Pipeline Embolization Device: the emergence of definitive endovascular remedy for intracranial aneurysms. International subarachnoid aneurysm trial 2009: endovascular coiling of ruptured intracranial aneurysms has no important advantage over neurosurgical clipping. Length of keep and complete hospital charges of clipping versus coiling for ruptured and unruptured adult cerebral aneurysms in the Nationwide Inpatient Sample database 2002 to 2006. Impact of International Subarachnoid Aneurysm Trial results on treatment of ruptured intracranial aneurysms in the United States. Geographic variation and regional trends in adoption of endovascular techniques for cerebral aneurysms. Lifelong rupture risk of intracranial aneurysms depends on risk factors: a potential Finnish cohort research. Risk of rupture of small anterior speaking artery aneurysms is similar to posterior circulation aneurysms. Aneurysm geometry: an important criterion in selecting patients for Guglielmi detachable coiling. Safety and efficacy of balloon reworking approach during endovascular remedy of intracranial 391 3371. Use of the Outreach distal access catheter as an intracranial platform facilitates coil embolization of select intracranial aneurysms: technical observe. Balloon help as a routine adjunct to the endovascular treatment of cerebral aneurysms. Use of the Ascent balloon for a 2-in-1 reworking technique: feasibility and initial experience: case report. HyperForm remodelingballoon for endovascular treatment of wide-neck intracranial aneurysms. Balloon reworking of advanced anterior communicating artery aneurysms: technical considerations and issues. Angles between A1 and A2 segments of the anterior cerebral artery visualized by threedimensional computed tomographic angiography and affiliation of anterior communicating artery aneurysms. Impact of anatomical variations of the circle of Willis on the incidence of aneurysms and their recurrence fee following endovascular therapy. Endovascular remedy of difficult ruptured anterior communicating artery aneurysms based mostly on the anatomical features of the anterior communicating artery complex. Feasibility and limitations of endovascular coil embolization of anterior communicating artery aneurysms: morphological issues. Endovascular coiling as the first therapy technique for ruptured pericallosal artery aneurysms: outcomes, problems, and observe up. The influence of configuration and location of ruptured distal cerebral anterior artery aneurysms on their remedy modality and results: evaluation of our casuistry and literature evaluate. Endovascular therapy of ophthalmic artery aneurysms: assessing balloon check occlusion and preservation of vision in coil embolization. Branch retinal artery occlusion after coil embolization of a paraclinoid aneurysm. Temporary balloon occlusion to test adequacy of collateral move to the retina and tolerance for endovascular aneurysmal coiling. Retinal artery occlusion following coil embolization of carotid-ophthalmic aneurysms. Clinical and anatomic outcomes after endovascular coiling of middle cerebral artery aneurysms: report on 30 handled aneurysms and evaluate of the literature. Endovascular remedy with naked platinum coils for center cerebral artery aneurysms. Endovascular administration of dissecting vertebrobasilar artery aneurysms in patients presenting with acute subarachnoid hemorrhage. Relation between aneurysm quantity, packing, and compaction in a hundred forty five cerebral aneurysms treated with coils. Endovascular occlusion of intracranial aneurysms with Guglielmi detachable coils: correlation between coil packing density and coil compaction. Finite component modeling of embolic coil deployment: multifactor characterization of therapy results on cerebral aneurysm hemodynamics. A digital coiling approach for image-based aneurysm models by dynamic path planning. How do coil configuration and packing density affect intra-aneurysmal hemodynamics Critical affect of framing coil orientation on intra-aneurysmal and neck region hemodynamics in a sidewall aneurysm model. Modeling the interplay of coils with the local blood move after coil embolization of intracranial aneurysms. Hemodynamics of cerebral aneurysms: computational analyses of aneurysm progress and therapy. Long-term end result of endovascular reconstruction with the Pipeline Embolization Device within the administration of unruptured dissecting aneurysms of the intracranial vertebral artery. Endovascular therapy of advanced aneurysms on the vertebrobasilar junction with flowdiverting stents: initial experience. Cost comparability of endovascular remedy of anterior circulation aneurysms with the Pipeline Embolization Device and stent-assisted coiling. Endovascular treatment of intracranial unruptured aneurysms: systematic evaluate and 96. Sixteen-year single-surgeon experience with coil embolization for ruptured intracranial aneurysms: recurrence charges and incidence of late rebleeding. Cerecyte coil trial: angiographic outcomes of a potential randomized trial comparing endovascular coiling of cerebral aneurysms with both Cerecyte or bare platinum coils. McDougall Wide-necked aneurysms are typically defined as lesions with necks 4 mm or more wide or with dome/neck ratios of less than 2. Historically, wide-necked aneurysms have been thought-about untreatable by endovascular means due to the risk of coil herniation into the parent vessel. Coil embolization depends on intraaneurysmal occlusion, and periprocedural and long-term outcomes with this system are affected by neck width. Finally, the stent may be placed on the end of the procedure after coils have been placed with balloon assistance. A second stent is then superior by way of the first stent and into the contralateral department vessel, forming a "Y" form with the opening of the "Y" dealing with the aneurysm neck. The intersection of the stents types a scaffold upon which coils may be placed into the aneurysm with out parent vessel herniation. In the "kissing" Y-stent method, every stent is deployed from each department vessel into the mother or father artery in parallel. In addition, use of dual antiplatelet therapy usually inhibits quick aneurysmal thrombosis. However, at follow-up in most sequence, researchers have reported charges of full occlusion between 54% and 81%. In one evaluation,12 the overall incidence of complications was reported to be 19% and the mortality price to be 2. Thromboembolic issues were the first contributor, liable for roughly 10% of the general complication fee and leading to demise in 0. Stent placement acts in much the same means that balloons do: the stent stabilizes a coil mass within the dome of the lesion and minimizes the danger of coil herniation. However, closed-cell stents are limited in their capability to adapt to vessel curvature because of their unsegmented design, which may result in flattening or kinking of the stent and subsequently incomplete stent apposition in tortuous vessels. The most common is to first microcatheterize the aneurysm and then "jail" the coiling microcatheter within the aneurysm dome, between the stent and the father or mother vessel wall, earlier than coiling. This, in turn, can assist in achieving denser packing, thereby minimizing the chance of coil compaction in wide-necked aneurysms. In addition, complexity of lesions that necessitate reworking might diminish the added benefit of balloon transforming. Earlier knowledge advised that use of the balloon transforming method for all intracranial aneurysms was associated with larger intraprocedural complication rates; nonetheless, more modern prospective trials have demonstrated similar charges of complications for balloon transforming and primary coil embolization. Balloon transforming approach with the utilization of an ipsilateral trajectory from the A1 to A2 segments of the best anterior cerebral artery. Balloon reworking method with using a contralateral trajectory from the A1 segment of the left anterior cerebral artery to the A2 phase of the proper anterior cerebral artery. Balloon remodeling technique with the utilization of two crossing balloons from bilateral A1 segments of the anterior cerebral artery to an anomalous left A2 complex. Although remedy of unruptured aneurysms carries a decrease threat of intracranial and extracranial hemorrhagic problems with antiplatelet remedy than does that of ruptured lesions, avoidance of antiplatelet therapy remains preferable, particularly in view of complications arising from patient noncompliance or antiplatelet resistance. Published rates range, relying on how problems are defined; transient/minor procedural complications have been reported in as much as 28. The danger of thromboembolic complications from endovascular remedy may be larger in the setting of subarachnoid hemorrhage. This design maintains most, however not all, blood circulate via the stent and normal mother or father vessel by lowering pulsatile arterial influx, whereas preserving the patency of branching and perforating arteries. Although wide-necked aneurysms pose a problem for any therapy modality, the growth of tools and strategies allows protected and effective endovascular treatment of these lesions. The surgeon must fastidiously think about the dangers related to stenting of ruptured wide-necked aneurysms. Review of 2 many years of aneurysm-recurrence literature, half 1: lowering recurrence after endovascular coiling. Histopathological assessment of deadly ipsilateral intraparenchymal hemorrhages after the remedy of supraclinoid aneurysms with the Pipeline Embolization Device. Treatment of intracranial aneurysms with the Enterprise stent: a multicenter registry. The Pipeline Embolization Device for the intracranial therapy of aneurysms trial. Analysis of problems and recurrences of aneurysm coiling with special emphasis on the stentassisted technique. Procedural complications of coiling of ruptured intracranial aneurysms: incidence and risk elements in a consecutive sequence of 681 patients. Balloons and stents in the endovascular remedy of cerebral aneurysms: vascular anatomy reworked. Our capricious vessels: the affect of stent design and vessel geometry on the mechanics of intracranial aneurysm stent deployment. X-configured stent-assisted coiling in the endovascular remedy of advanced anterior communicating artery aneurysms: a novel reconstructive technique. A novel endovascular therapy of a wide-necked basilar apex aneurysm by using a Y-configuration, double-stent technique. X-configuration intersecting Enterprise stents for vascular remodeling and assisted coil embolization of a large neck anterior communicating artery aneurysm. Incidence of cerebral ischemic occasions after discontinuation of clopidogrel in patients with intracranial aneurysms treated with stent-assisted techniques. Clopidogrel resistance is associated with thromboembolic complications in patients undergoing neurovascular stenting. Endovascular therapy of unruptured intracranial aneurysms: comparability of safety of remodeling approach and commonplace therapy with coils. Safety and efficacy of balloon remodeling approach throughout endovascular treatment of intracranial aneurysms: critical evaluation of the literature. Evaluation of the soundness of aneurysms after embolization using removable coils: correlation between stability of aneurysms and embolized quantity of aneurysms. Impact of anatomic features in the endovascular embolization of 181 anterior communicating artery aneurysms.