Michael J. Paidas, MD
- Associate Professor
- Co-Director, Yale Women and Children? Center for Blood Disorders
- Co-Director, National Hemophilia Foundation?Baxter
- Clinical Fellowship Program at Yale
- Division of Maternal- Fetal Medicine
- Department of Obstetrics, Gynecology, and
- Reproductive Sciences
- Yale University School of Medicine
- New Haven, Connecticut
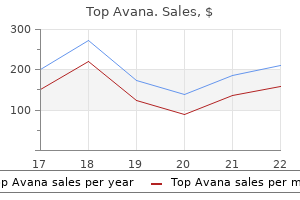
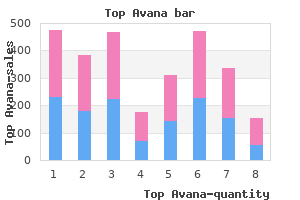
Singh R erectile dysfunction treatment dallas cheap top avana 80mg without prescription, Rambani R erectile dysfunction vitamin d top avana 80 mg free shipping, Kanakaris N laptop causes erectile dysfunction purchase 80mg top avana mastercard, et al: A 2-year expertise erectile dysfunction japan generic top avana 80mg on line, management and outcome of 200 clavicle fractures. Chalidis B, Sachinis N, Samoladas E, et al: Acute administration of clavicle fractures. Myderrizi N, Mema B: the hematoma block: an efficient different for fracture reduction in distal radius fractures. Handoll H, Madhok R, Dodds C: Anaesthesia for treating distal radial fracture in adults. Distal traction is applied (arrow) while decreasing the medial or lateral displacement (arrowheads). Any patient with an open fracture, evidence of neurologic or vascular compromise, or suspicion of a compartment syndrome must be admitted to the hospital after an emergent session with an Orthopedic Surgeon. This is most often a neurapraxia and should involve any of the three nerves crossing the fracture. The neurovascular structures crossing the fracture could become lacerated or entrapped through the reduction. The commonest mechanism of injury includes a fall onto an outstretched hand with the elbow locked in extension. Brahm J, Turner J: A randomized controlled trial of emergency department ultrasound-guided discount of distal radius fractures. Wegmann H, Eberl R, Kraus T, et al: the impact of arterial vessel accidents associated with pediatric supracondylar humeral fractures. Nomura O, Tanji A, Inoue N: A bruised dimple on an injured elbow: what does it imply Neidenback P, Audige L, Wilhelmi-Mock M, et al: the efficacy of closed discount in displaced distal radius fractures. According to Advanced Trauma Life Support tips, the injured extremity should be aligned and immobilized after the appropriate administration of any life-threatening problems. External immobilization with splinting or casting is often the definitive administration of injured extremities within the Emergency Department. Knowledge and expertise on this therapeutic process are important for any Emergency Physician. Splints are commonly used for the immobilization of upper and lower extremity accidents. The major disadvantages of splints are that they provide barely much less rigid immobilization than casting and require an Orthopedic Physician visit within a quantity of days to be replaced with a forged. Casts, that are usually circumferential, are better fitted to the definitive therapy of fractures and ligamentous injuries. Casts present superb immobilization and allow for the upkeep of a reduced fracture. The rigidity of a forged limits the amount of swelling and soft tissue edema in the first 24 to forty eight hours after the injury and is subsequently associated with an increased risk of growing a compartment syndrome. They are often cut up (bivalved) to allow swelling and prevent the development of a compartment syndrome before the affected person is discharged from the Emergency Department. To acquire a three-point mould, place one point of contact over the convex side of the fracture site. The other two factors of pressure are aimed in an wrong way, proximal and distal to the fracture, and from the concave side. This is the classic teaching of Sir John Charnley who famous that "a curved plaster is critical in order to make a straight limb. Casts and splints also depend on hydraulic force to maintain limb size and alignment. One could consider the soft tissues surrounding the damaged bones as constituting a versatile cylinder that contains the underlying fracture, hematoma, and edema. Axial loading of the bones will trigger the delicate tissue to broaden and permit the limb to shorten. A well-applied solid or splint will resist the outward 113 Casts and Splints Eric F. References to plaster use and varied immobilization techniques are scattered throughout historical records. The use of plaster of Paris, additionally referred to as plaster, in fracture administration dates back to the eighteenth century Turkish Empire. Three points of pressure are appearing on the injured extremity in a well-applied solid or splint. Two opposing forces are applied at sites proximal and distal to the fracture and on the concave facet of the fracture (2). The initial neurovascular examination, momentary splinting, and post-splinting neurovascular examination should be carried out earlier than the patient undergoes radiographic studies. Immobilize an extremity within the applicable and definitive splint after diagnosing and stabilizing the fracture. A thorough neurologic and vascular examination of the extremity should be carried out and documented after the placement of the definitive splint. The patient with ligamentous sprains or muscle strains may also receive important pain aid with splint immobilization. Splints are placed following orthopedic or delicate tissue surgical procedure of the extremities. The calcium sulfate is impregnated into muslin sheets containing dextrose or starch. Plaster grades embrace fast-setting and extra-fast-setting plaster, that are helpful for different applications. Long cylindrical crystals kind and interlock because the forged sets to give strength to the cast. Using heat water will speed up the chemical response, harden or set the plaster sooner, and reduce the setting time. Unfortunately, the use of very heat or scorching water will also improve warmth manufacturing while the plaster units. The use of very thick splints or fast-setting plaster may also improve the warmth produced throughout setting. Use cold water to activate the plaster, enhance the setting time, and reduce the warmth produced throughout setting. Great care ought to be taken if heat water is used in applying a cast or splint to an anesthetized affected person, unconscious or altered patient, or an insensate limb. The fiberglass splinting materials consists of cloth impregnated with a plastic, spun glass resin, and a water-activated catalyst. Following reduction of sure fractures, placement of a cast will secure the bones of their correct alignment and permit for a main union. Patients with casts might current to the Emergency Department with various cast-associated issues. The forged may not match properly if the affected extremity has decreased in dimension from discount of swelling. The cast must be eliminated and the affected area examined if the affected person complains of persistent pain. They may be positioned in an acceptable splint and follow-up arranged with an Orthopedic Surgeon for casting. In this setting, the wounds ought to be appropriately dressed, padded, and the splint constructed in order that it might possibly simply be removed and replaced. Similarly, infections of joint spaces or soft tissues should stay uncovered for frequent evaluations. Splinting results in the reduction of ache, reduction of edema, aid of stress on neurovascular structures, and prevention of additional soft tissue injury. Any available materials can be utilized to immobilize or realign the affected extremity in the prehospital setting and within the Emergency Department. A thorough neurologic and vascular examination of the extremity must be performed and documented before briefly splinting the extremity. In common, 1 to 3 inch materials can be used for the arms and digits, 3 to 4 inch wide materials can be utilized for the higher extremity, and four to 5 inch broad materials can be used for the decrease extremity. Alternative materials embrace fiberglass strips and rolls as an alternative of plaster strips.
Left ventricular filling turns into compromised from the dearth of move from the right ventricle and the bulging inward of the interventricular septum erectile dysfunction doctor orlando buy 80mg top avana with visa. Cardiac perfusion ultimately decreases erectile dysfunction young adults order top avana with mastercard, the center contractibility is progressively impaired erectile dysfunction wikihow buy genuine top avana line, and the affected person turns into hypotensive erectile dysfunction causes cures order top avana from india. A progressive decline in cardiac output happens as pericardial fluid accumulates and intrapericardial stress increases. This is adopted by the equilibration of the proper atrial and intrapericardial pressures. Equilibration of diastolic pressure in every heart chamber happens and produces the greatest drop in cardiac output. The cardiac chambers collapse because the intrapericardial stress continues to improve. There is a disproportionate effect of the accumulation of small quantities of fluid on this late stage. The affected person can proceed from secure and compensated to profoundly unstable quite abruptly. It is harmful to depend on central venous strain line monitoring alone to recognize the evolution of cardiac tamponade. It can produce dramatic momentary enhancements in the scientific standing of the affected person if handled by the withdrawal of a small quantity of fluid from the pericardial cavity. Cardiac tamponade is a life-threatening condition that should be diagnosed and handled emergently. A pericardial catheter could be placed for ongoing removal of fluid from inside the pericardium. Pericardiocentesis could additionally be carried out to get hold of pericardial fluid for evaluation, to relieve the strain of a pericardial effusion, to enhance cardiac output, or as a lifesaving measure to relieve a cardiac tamponade. The approach is relatively easy to carry out yet has a major fee of problems. Cardiac tamponade was first described by Riolanus as early as 1649, with pericardiocentesis described in 1827 by Thomas Jowett as an intervention for pericarditis. The outer layer consists of a dense outer fibrous tissue with an inside layer of mesothelial cells generally identified as the parietal pericardium. The fibrous pericardium is connected to the central tendinous portion of the diaphragm inferiorly. The outer fibrous layer blends superiorly with the sheath overlaying the nice vessels. Any penetrating injury involving the "hazard zone" has the potential to trigger a cardiac damage and cardiac tamponade. View of the center and great vessels that can turn out to be injured behind the anterior chest wall. Restlessness, fatigue, tachycardia, and tachypnea are often current in cardiac tamponade. Cardiac tamponade must at all times be considered as a possible explanation for shock within the hypotensive affected person. The differential analysis contains acute myocardial infarction, cardiac shock, constrictive pericarditis, hypothermia, pneumothorax, and pulmonary embolism. Continue deflating the cuff pressure until heart beats are heard continuously in both inspiration and expiration. It could additionally be because of myocardial impairment, pericardial fluid, or restriction of the pericardium. This consists of central venous line placement, displaced fractured ribs, intracardiac injection, migrating pins or needles, pacemaker insertion, penetrating thoracic injuries, pericardiocentesis, surgery, and venous bullet embolization. Variation of the E wave is noted over the respiratory cycle with the bottom and highest velocities recorded as A and B, respectively. Some authors advocate using transesophageal echocardiography, even in unstable patients, due to its superior imaging when compared to transthoracic echocardiography. Use these for steady sufferers when assessing for a pericardial effusion and not cardiac tamponade. The discovering of an enlarged cardiac silhouette on a chest radiograph could additionally be useful in continual pericardial effusions but is usually absent or nonspecific in the acute setting. Pericardiocentesis may be performed to acquire pericardial fluid for diagnostic testing. Any uncorrected anticoagulation from medicines or a bleeding dysfunction shall be an absolute contraindication to performing the procedure in a secure patient. Small, loculated, or posteriorly situated effusions in a steady patient are considered contraindications. Pericardiocentesis is contraindicated in cardiac tamponade associated with myocardial free wall rupture after myocardial infarction, spontaneous aortic dissection, posttraumatic aortic dissection, or rupture of the ascending aorta. Some reports observe the pressure of the intrapericardial blood opposes additional bleeding. The removal of pericardial fluid reduces the strain and should cause further bleeding to occur, often with fatal results. These authors argue that when the analysis is made, the affected person ought to receive a immediate thoracotomy. Some Emergency Departments could not have single guidewires and versatile catheters available to use for a pericardiocentesis. A 6 to 10 French single-lumen central venous line entry kit could additionally be substituted in an emergency. The placement of an arterial line may be helpful for extra monitoring (Chapter 72). Insert a nasogastric tube to decompress the stomach and reduce the chance of gastric perforation by the pericardiocentesis needle (Chapter 75). These embrace beneath the xiphoid process, on the proper sternocostal margin, on the left sternocostal margin. This is the method described all through the "Techniques" section of this chapter. Anesthetize the needle tract with local anesthetic resolution if the affected person is awake. Place a subcutaneous wheal of local anesthetic solution on the web site chosen to insert the needle. Inject local anesthetic answer by way of the pores and skin wheal and into the subcutaneous and deeper tissues of the thoracic wall. Puncture the pores and skin with a #11 scalpel blade between the xiphoid course of and the left costal margin. Advance the spinal needle four to 5 cm whereas applying adverse stress to the syringe and observing the cardiac monitor. The aspiration of free-flowing blood will cease as the needle passes via the ventricular wall. Techniques to confirm the intraventricular placement of the needle tip have been described. There will be a marked enchancment in hemodynamics and clinical standing when the pericardial area is entered and fluid is aspirated. Alternatively, attach a three-way stopcock between the spinal needle and the syringe. The needle is inserted at a 45� angle to the midsagittal plane (A) and at a 45� angle to the abdominal wall (B). An assistant can open and shut the stopcock while the Emergency Physician aspirates fluid and ejects it by way of the extension tubing into a basin. Slowly withdraw the needle 2 to three mm if an harm sample seems on the cardiac monitor. The V1 lead will function an energetic electrode based at the tip of the spinal needle. The presence of a untimely ventricular contraction or a ventricular arrhythmia can signify contact with the myocardium. Slowly withdraw the needle in 1 to 2 mm increments if an damage pattern or premature ventricular complexes are seen. Continue to withdraw the needle in 1 to 2 mm increments until the injury sample resolves. This may be carried out in cases of medical or traumatic pericardial effusions since the pericardial fluid often reaccumulates. An indwelling catheter permits intermittent drainage of pericardial fluid with out the potential problems related to repeated needle sticks from a pericardiocentesis. It is imperative that the tip of the spinal needle be within the pericardial cavity and not within the cardiac chamber.
Generic top avana 80mg on line. Is Erectile Dysfunction Ruining Your Sex Life?.
A paracentesis or "belly tap" is warranted in a affected person with new-onset ascites to establish the etiology of the fluid erectile dysfunction doctor las vegas best top avana 80 mg. A paracentesis could also be therapeutic in patients with cardiorespiratory or gastrointestinal manifestations secondary to tense ascites erectile dysfunction bathroom buy 80mg top avana with amex. Paracentesis is used to manage some patients with hepatorenal syndrome at the facet of the consultant erectile dysfunction treatment food purchase cheap top avana line. This includes sufferers receiving antibiotics erectile dysfunction in teenage cheap top avana generic, chemotherapeutics, and frequent paracenteses. Another position one would possibly consider is having the affected person assume a hand-knee or "crawling" position. Remember that the fluid will pool in dependent areas and the gut will float on top of it, barring any adhesions or lots. Inject 2 to 5 mL of local anesthetic answer subcutaneously and alongside the needle insertion tract. This method should be adopted when using the opposite strategies described below. The pores and skin will return to its normal place when the stress is launched and seals off the pathway of the paracentesis needle. Continue to aspirate till the syringe is one-half to three-fourths filled with fluid. The omentum, a loop of gut, peritoneal fat, or other tissue may be occluding the needle tip if ascitic fluid all of a sudden stops flowing into the syringe. Withdraw the needle to the dermis, reposition it, after which readvance it into the peritoneal cavity. The Caldwell needle appears to be superior to a standard angiocatheter needle in terms of issues with fluid return. Immediately place the fluid into the appropriate assortment tubes and tradition bottles. Connect the opposite finish of the intravenous tubing to a suction bottle or bag to drain off the specified amount of ascitic fluid. Alternative sites are just medial and 4 to 5 cm above the anterior superior iliac spines. It prevents an iatrogenic perforation if the stomach is dilated or if a concomitant gut obstruction is current. The first website is in the midline and 2 cm under the umbilicus through the avascular linea alba. Alternatively, the area 4 to 5 cm superior and simply medial to the anterior superior iliac backbone in one of many decrease quadrants could additionally be used. This location must be lateral to the rectus abdominis muscle to avoid damage to the inferior epigastric artery, which runs vertically along the muscle sheath. Some Emergency Physicians choose the best decrease quadrant to keep away from the sigmoid colon and spleen. Remember to train caution in the regions of caput medusa, outstanding veins, veins, scarring, over an space of inflamed or infected pores and skin to decrease issues. Lying in the proper lateral decubitus place for a proper decrease quadrant approach or mendacity within the left lateral decubitus position for a left lower quadrant method increases dependency of the ascites to a desirable quadrant while displacing the Reichman Section5 p0657-p0774. Consider a compression dressing with an occlusive bandage if fluid is oozing from the puncture web site. The needle used to insert the wire may be brief and a smaller gauge than the catheter. Materials wanted for catheter insertion are commercially available in a prefabricated kit. The Seldinger method is most commonly used for central venous catheter insertion and acquainted to the Emergency Physician. The introducer needle has a tapered hub on the proximal end to guide the wire into the needle lumen. Always have a minimum of one hand holding the guidewire to prevent it from slipping completely into the peritoneal cavity. The syringe is removed and a guidewire is inserted by way of the needle and into the peritoneal cavity. The dilator and sheath are advanced into the peritoneal cavity with a twisting motion. The aspiration of ascitic fluid confirms correct intraperitoneal placement of the sheath. Direct the sharp fringe of the scalpel blade away from the guidewire to avoid nicking the guidewire. Connect the opposite finish of the intravenous tubing to a suction bottle or bag to drain the specified quantity of fluid. An alternative is to attach a three-way stopcock to the distal end of the intravenous tubing. It is easy to be taught and can be performed in a couple of minutes by an skilled Emergency Physician. A flash of fluid in the syringe confirms that the tip of the needle is within the peritoneal cavity. Advance the needle a further 2 to three mm to be positive that the tip of the needle is totally throughout the peritoneal cavity. Immediately place the nondominant thumb over the needle hub to forestall air from entering and fluid from exiting. Advance the catheter through the needle until the desired length of catheter is inside the peritoneal cavity. The needle is advanced into the peritoneal cavity while sustaining negative stress on the syringe. The aspiration of ascitic fluid confirms proper intraperitoneal placement of the catheter. The main drawback of this technique is the chance of the needle tip shearing off the catheter and resulting in a catheter embolism. This could be prevented by not withdrawing the catheter by way of the needle and making use of the needle guard immediately after the needle is withdrawn from the pores and skin. Another drawback is that the contaminated needle must be dealt with to some extent, creating a possible danger for needle stick accidents. They are inexpensive, are available in a variety of diameters and lengths, and are widely available. The catheterover-the-needle is inserted into the peritoneal cavity whereas maintaining unfavorable stress on the syringe. Consider using a Caldwell needle with fenestrations on the facet to help decrease problems with the circulate of fluid. A flash of fluid within the hub of the needle confirms that the tip of the needle is within the peritoneal cavity. Advance the catheter-overthe-needle an additional 2 to 3 mm to make sure that the catheter is within the peritoneal cavity. Connect the other finish of the tubing to a suction bottle or bag to drain the specified amount of fluid. The intestine could also be seen undulating within the ascites as a end result of intestinal peristalsis. A static technique is used to determine the skin puncture website and ascitic fluid location. The the rest of the process is "blind" utilizing one of the above described techniques. Note the quantity of fluid and the presence of any construction that may make a website undesirable. Ascites will outline individual gut loops and appears in lots of places around the stomach. Loculated ascites will often mimic a cyst however will still outline the loops of intestine. The needle (arrows) is inserted via the abdominal wall and into the free fluid.
Alternatively impotence trials france purchase top avana 80mg on line, the dominant index finger can be placed through the tract to direct the chest tube erectile dysfunction treatment pdf discount top avana 80mg overnight delivery. The use of the finger in the tract is the popular technique to guide the chest tube erectile dysfunction over 60 generic 80 mg top avana fast delivery. The finger will have the power to erectile dysfunction treatment old age buy top avana overnight delivery confirm the right intrapleural placement of the chest tube. Release the Kelly clamp and advance the chest tube till all the fenestrations are within the pleural cavity and the preplaced clamp on the chest tube is at the pores and skin incision. The many strategies which were described for securing chest tubes are idiosyncratic and probably equivalent. Wrap the needle finish of the suture firmly around the chest tube three or four occasions. An occlusive dressing has been positioned over the incision and taped to the chest wall. This stitch might be used later to shut the pores and skin incision after the chest tube is removed. Place simple interrupted or horizontal mattress sutures to shut the remainder of the skin incision. Apply petrolatum gauze over the incision site and around the chest tube because it exits the incision. It seals the chest wall incision from the ambiance and prevents air from the ambiance from entering the pleural space from across the chest tube. It has an connected cable tie to wrap across the chest tube and secure it in place. The second chamber contains a small amount of saline or water and acts as a one-way valve. The third chamber controls suction, with a capability of a minimal of 20 cmH2O suction, and attaches to the wall suction system. Aiming superiorly decreases the probability of chest tube placement within the lung fissure. It has been adopted by some to be used in trauma sufferers within the Emergency Department. Insert the catheter-over-the-needle over the superior border of the rib to avoid the neurovascular bundle located on the inferior border of the rib. Hold the guidewire securely to forestall it from falling completely into the pleural cavity. The chest tube could be inserted into the pleural apex (area 1) or pleural base (area 2). A pneumothorax could additionally be more readily identified with the patient positioned supine rather than upright with ultrasound. Aspirate a pneumothorax utilizing the ultrasound much like a pleural effusion (Chapter 52) or insert a chest tube. The chest tube is guided into the pleural cavity through the KatGuide as a substitute of utilizing a finger and Kelly clamp. The KatGuide enhances the possibility of optimal chest tube positioning and reduces the danger of chest tube misplacement. The rounded tip and the insertion direction parallel to the lung surface stop lung damage. Stripping refers to creating adverse pressure inside the tubing to move fluid or clots distally and into the amassing chamber. To milk the tube, clamp or pinch the tubing shut distally while utilizing the opposite hand to compress the tubing and transfer proximally to drive the contents again into the thoracic cavity. To strip the tube, clamp or pinch the tubing shut proximally whereas using the opposite hand to compress the tubing and transfer distally adopted by the sudden release of the proximal tubing. Remove the chest tube and insert a new one if it is bent, kinked, or within the fissure of the lung. If its tip is against the mediastinum, unsecure the tube, withdraw it a number of centimeters, resecure the tube, and procure a repeat radiograph. Never advance a chest tube additional into the thoracic cavity after acquiring a chest radiograph to forestall monitoring infectious materials into the pleural cavity. Persistent bubbling in the system or failure of the lung to reexpand signifies a leak within the system. Place tape over the connections to eliminate leaks and stop the components from becoming dislodged. Examine the chest tube and the radiograph to verify that each one fenestrations are inside the thoracic cavity. An harm to the trachea, mainstem bronchus, a large bronchiole, or the esophagus can cause a persistent air leak. Large or persistent air leaks often characterize proximal tracheobronchial accidents and may require urgent surgical intervention. Have all the necessary tools and provides available in case the patient urgently requires a brand new chest tube. Don gloves, a robe, a face mask with a watch shield or goggles, and a cap to forestall changing into contaminated when the chest tube is removed. Untie the bow securing the free ends of the purse-string suture that was beforehand positioned. Quickly and easily take away the chest tube while the assistant cinches down the knot of the suture to seal the pores and skin incision. This is ideally carried out with petrolatum and standard gauze as the chest tube is being removed. Observe the patient for 4 to 6 hours for any signs of cardiovascular or respiratory compromise. Obtain expiratory posteroanterior and lateral chest radiographs if the affected person stays asymptomatic. Evaluate the radiograph for the presence or recurrence of a hemothorax, hydrothorax, pneumothorax, or pyothorax. Obtain every day serial chest radiographs to monitor for resolution of the inciting course of. The presence of air leaks from the chest tube signifies that the harm has not fully healed and the seal between the parietal and visceral pleurae has not yet been restored. The acceptable minimal daily output from a chest tube as a criterion for elimination varies in accordance with the establishment, the doctor, and the explanation for insertion. It is also unclear whether a trial period of water seal following suction is strictly necessary. There is literature to suggest that suction and water seal protocols for removing chest tubes are efficient and have comparable incidences of recurrent pneumothoraces. The tubing could also be milked or stripped to alleviate the blockage and avoid the want to exchange the chest tube. Injury to the thoracic duct from the chest tube being inserted too deeply may end up in a chylothorax. It is imperative that the Kelly clamp be controlled as it enters the pleural cavity. If the lung is adherent to the chest wall, it may be penetrated by the Kelly clamp or the chest tube. A trocar should never be used to insert a chest tube as it could possibly Reichman Section3 p0301-p0474. Allergic reactions can happen to the skin preparation, local anesthetic answer, or tape. Posttraumatic empyema remains a critical complication of thoracic trauma with incidences ranging from 2% to 25%. A break in sterile method on chest tube insertion, nosocomial pneumonia, superinfected pulmonary contusion, and undrained hemothoraces have all been implicated. Empyemas attributed to the chest tube insertion are utterly preventable problems that can be averted by strict adherence to aseptic technique. Other infectious problems embrace chest wall cellulitis and necrotizing fasciitis.